Asian Case Reports in Pediatrics
Vol.1 No.2(2013), Article ID:11767,2 pages DOI:10.12677/ACRP.2013.12004
Intracranial Fungal Granuloma: A Case Report
1Department of Pediatrics, West China Second University Hospital, Sichuan University, Chengdu
2Department of Pathology, West China Second University Hospital, Sichuan University, Chengdu
Email: carolyn18@126.com, huaxigaoshan@163.com, *liuhengru@yahoo.com.cn, xulian@foxmail.com
Received: Dec. 17th, 2012; revised: Jan. 9th, 2013; accepted: Jan. 28th, 2013
Copyright © 2013 Linmin Kang et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT:
Background: Fungi can intrude into brain, meninges and intracranial blood vessels in different ways, causing several diseases including intracranial fungal granuloma (IFG), which is not common but has a high mortality rate (50% - 63%). Domestic literature about IFG is mostly reported in adult population other than children population. Methods: A 11 year-old female was admitted to the inpatient apartment of pediatrics. The patient showed repeated right occiput pain for more than 3 months, aggravated with vomiting for 15 days. Physical examination on admission revealed no abnormalities. MRI revealed intracranial space-occupying lesions. Then we gave her surgical treatment. The postoperative diagnosis was intracranial fungal granuloma, so that we gave her the antifungal treatment and nursing. Results: The patient showed no more headache ever since the surgery. Until the date of sending out this paper, the patient showed no abnormal clinical manifestations. Conclusion: At present, surgery combined with antifungal therapy should still be considered as the ultimate choice of IFG treatment.
Keywords: Intracranial Fungal Granuloma; Aspergillus; Therapy
颅内单纯真菌性肉芽肿1例报告
康琳敏1,高 珊1,罗 蓉1*,徐 炼2
1四川大学华西第二医院儿科,成都
4四川大学华西第二医院病理科,成都
Email: carolyn18@126.com, huaxigaoshan@163.com, *liuhengru@yahoo.com.cn, xulian@foxmail.com
摘 要:
背景:真菌以不同方式和程度累及脑组织、脑膜和颅内血管,其中颅内真菌性肉芽肿(intracranial fungal granuloma, IFG)并不常见,但死亡率高(50%~63%)。国内IFG文献多见于成人病例的个案报道,少见儿童报道。方法:11岁大女性患儿1例,因“反复右枕部疼痛3个月,加重伴呕吐半月”入院,入院查体无异常,MRI提示颅内占位性病变,遂给予手术处理,术后诊断颅内真菌性肉芽肿,并给予术后抗真菌治疗及护理。结果:术后患儿头痛症状消失,至本文投送之日,患儿无临床症状再次出现。结论:手术联合抗真菌治疗IFG仍应作为目前首选治疗方案。
收稿日期:2012年12月17日;修回日期:2013年1月9日;录用日期:2013年1月28日
关键词:颅内真菌性肉芽肿;曲霉菌;治疗
1. 病例报告
患儿女,11岁,因“反复右枕部疼痛3个月,加重伴呕吐半月”入院。入院查体:未见任何异常。MRI (图1)示:右小脑半球及右枕部不规则肿块影。病灶大小约4.2 × 6.5 cm,右小脑半球病灶大小2.8 × 2.9 cm。诊断:1) 右小脑半球占位;2) 右枕部占位。于

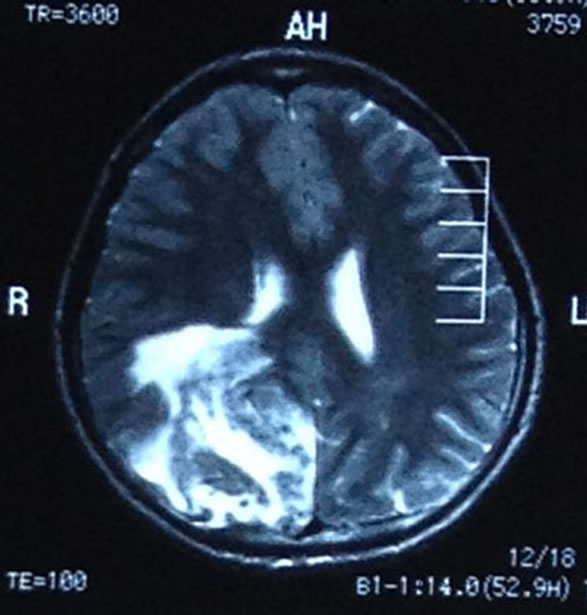
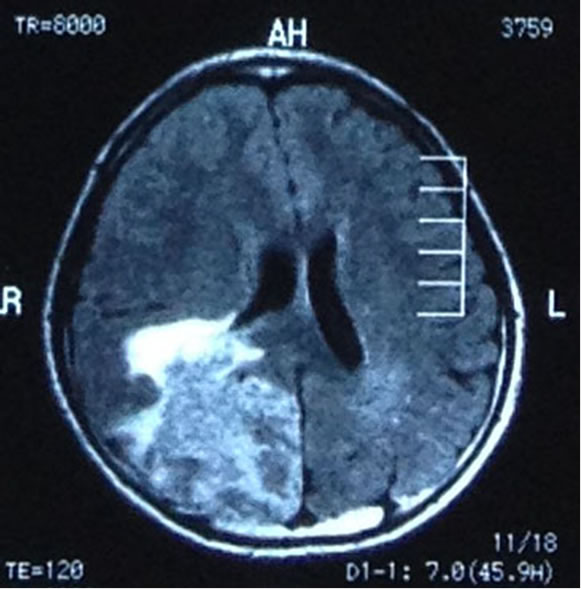
Figure 1. Imaging (CT\MRI): Signson CTandMRI The CT and the MRI scan shows irregular mass lesions in the right cerebellar hemisphere and the right occiput
图1. 影像(CT\MRI):右小脑半球及右枕部不规则肿块影
2012.5.25全麻下行幕上浅部病变切除术 + 右侧小脑半球占位切除术 + 开颅颅内减压术 + 颅内压监护传感器置入术。术中见:脑脊液清亮,颅内压稍高,幕上右侧占位病变,大小约7 × 7 cm。边界欠清晰,鱼肉样,局灶硬化结节。右侧小脑半球病灶约3 × 2 cm 大小。术中冰冻提示:炎性病变或肉芽肿可能。术后病检(图2和3)证实2012.5.26(右枕、右小脑半球)坏死
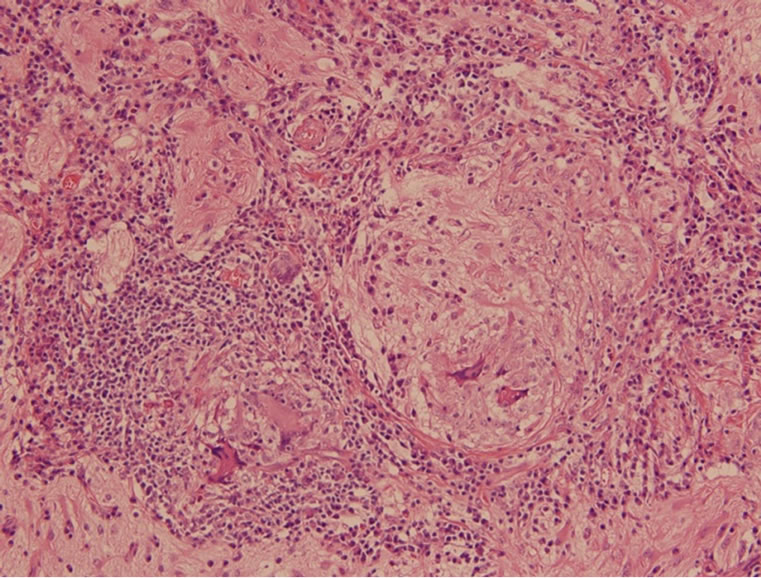
Figure 2. Microscopic appearance of multinucleated giant cell granuloma of the brain (HE stain, ×400)
图2. 病理(HE染色):显示多核巨细胞肉芽肿性炎形成
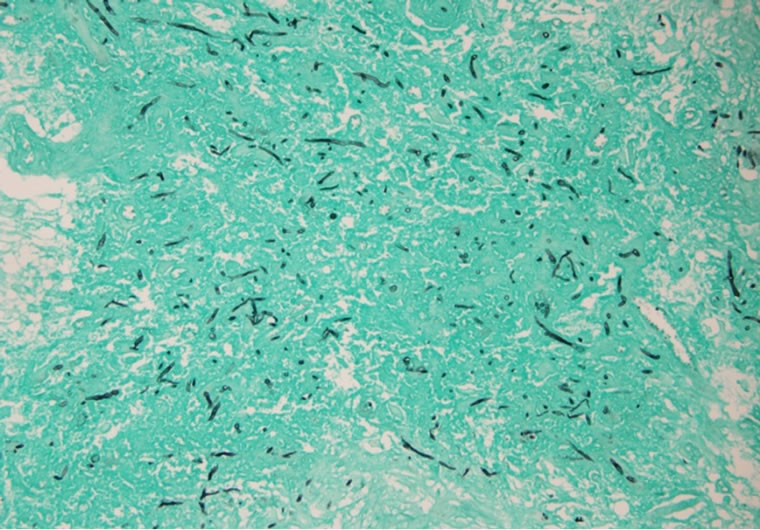
Figure 3. Photomicrograph showing the fungal hyphae and spores on Gomori silver methenamine silver (GMS) stain (GMS Stain, ×400)
图3. 病理(六胺银染色)病变组织中六胺银染色阳性的真菌菌丝及孢子,致病菌丝长短不一,粗细较一致,形态倾向曲霉菌
和肉芽肿(含多核巨细胞)。PAS和六胺银染色查见大量真菌菌丝,支持为真菌感染。Warthin-Starry染色未见明确阳性病原体。抗酸染色(−)。结核杆菌PCR检测(−)。免疫组化示背景脑组织呈GFAP(+)/Oligo- 2(+),NeuN(−)、IDH1(−)、CD1a(−);散在Ki67阳性细胞。术后第二天,患儿头痛症状即消失。术后诊断:右枕部、右小脑半球真菌感染。术后10天(2012. 6. 5)转至我科。入院后患儿体温始终正常,查体未见异常,否认既往脑部外伤史、鸟类接触史、及传染病史,实验室及其他辅助检查提示:血、骨髓、CSF涂片及培养均未见细菌及真菌,真菌G试验结果阴性。CD3、CD4、CD3/CD4正常。
2. 诊断
1) 颅内真菌性肉芽肿:曲霉菌感染?2) 幕上浅部病变切除术 + 右侧小脑半球占位切除术后。术后给予伏立康唑0.186~0.279 g Q12 h静滴10天,随后更换为两性霉素B脂质体4.5~140 mg Qd静滴26天,停用两性霉素B脂质体后给予伏立康唑0.2~0.4 gbid口服至术后2个月。至本文投送之日,患儿无临床症状再次出现。
3. 讨论
真菌以不同方式和程度累及脑组织、脑膜和颅内血管,其中颅内真菌性肉芽肿(intracranial fungal granuloma, IFG)并不常见,但死亡率高(50%~ 63%)[1],脑膜脑炎是最主要的死亡原因,感觉缺损、肉芽肿中有脓性成分、严重脑水肿,均提示预后差。另外,实质性肉芽肿常伴发血管炎和血管内血栓形成,一旦发生,其死亡风险更高,考虑可能的原因是化学药物极可能对难以逆转的血管内侵袭和继发性梗阻无效[2]。但在儿童群体中的疾病结局极可能优于成人[3]。国内IFG文献多见于成人病例的个案报道,少见儿童报道。IFG最常见的症状是头痛、呕吐、凸眼、视力障碍及视乳头水肿[1]。,临床症状及体征无特异性,CT、MRI扫描往往无特征性表现,有文献提示CT上的“开环征”可能对诊断有一定的特异性[4],本患儿无CT开环征。病理染色可明确诊断真菌感染,但不能确认具体病原,需要培养结果,但中枢神经系统感染真菌者,脑脊液真菌培养阳性率往往并不高(31%)[5];病理确诊的IFG患者血/尿的涂片/培养的阳性率约60%[3]。本例患儿病理切片六胺银染色证实为真菌感染,结合临床及病理表现特点病原菌可能为曲霉菌属(图2和3)。曲霉菌是形成IFG最常见的病原菌,IFG感染途径主要有:1) 直接感染:如开放性外伤感染;2) 血行播散;3) 邻近感染:如鼻窦炎;4) 姻缘性。真菌感染的易感因素包括营养状况差、滥用药物(抗生素、镇痛药、抗结核、激素、免疫抑制剂)、高龄、患恶性肿瘤、免疫功能缺陷和寄生虫感染等。没有发现可能的感染途径和易感因素是本例患儿的特征之一。仅为限局性肉芽肿并位于枕部、右小脑半球是本例患儿特征之二,因IFG最常见部位为额叶、颞叶,其他部位为顶叶、颞顶叶、前颅窝、中颅窝、鞍区和鞍旁区、后颅窝[1]。本个案血、骨髓、CSF涂片及培养均未见细菌及真菌,真菌G试验结果也为阴性。原因可能为:1) 该患儿除头痛、呕吐外,一般情况良好,除局灶占位性改变外,并无大量真菌进入血液及其他体液中,故出现上述病理与实验室检查结果的背离;2) 任何实验室检查均可能有假阴性结果的存在。
手术联合抗真菌治疗是目前首选治疗方案。外科病灶切除疗效确切,可减轻颅内压迫和降低颅内压,防止发生严重的CNS后遗症,改善预后。术后抗真菌治疗应当早期、足量,足够疗程。初始全身治疗首选伏立康唑,康唑不能耐受或治疗无效的患者,可替代选用伊曲康唑、泊沙康唑或LFABs(包括两性霉素B脂质体复合物)。本例患儿手术后次日临床症状即完全消失,随访至稿件投送之时,患儿无临床症状反复,据此我们考虑是否应视为单纯手术效果好。该病例也再次证明目前主流观点的正确性,即虽然没有决定性的证据证明根治性和激进的手术能够促进颅内真菌性肉芽肿患者的治疗结局,但是每当手术可行,且不会导致严重的并发症等恶性结局时,仍应采取恰当而彻底的手术[6]。
参考文献 (References)
[1] A. R. Dubey, V. Patwardhan, S. Sampth, et al. Intracranial fungal granuloma: Analysis of 40 patients and review of the literature. Surgical Neurology, 2005, 63(3): 254-260.
[2] B. S. Sharma, V. K. Khosla, V. K. Kak, et al. Intracranial fungal granuloma. Surgical, 1997, 47(5): 489-497.
[3] J. Dotis,E. Iosifidis, E. Roilides, et al. Central nervous system aspergillosis in children: A systematic review of reported cases. International Journal of Infectious Diseases, 2007, 11(5): 381- 393.
[4] 陈永华, 何玉麟, 李五根, 夏国金. 颅内真菌感染的CT和MRI表现[J]. 中国医药导报, 2010, 7(17): 66-68.
[5] C. Sundaram, P. Umabala, et al. Pathology of fungal infections of the central nervous system: 17 years’ experience from Southern India. Histopathology, 2006, 49(4): 396-405.
[6] A. A. Siddiqui, A. A. Shah and S. H. Bashir. Craniocerebralaspergillosis of sinonasal origin in immunocompetent patients: Clinical spectrum and outcome in 25 cases. Neurosurgery, 2004, 55(3): 602-613.
NOTES
*通讯作者。