Asian Case Reports in Pediatrics
Vol.1 No.3(2013), Article ID:12177,3 pages DOI:10.12677/ACRP.2013.13009
Diagnosis of Abernethy Malformation in 2 Cases
1Department of Radiology, Union Hospital, Wuhan
2Department of Pediatrics, Union Hospital, Wuhan
Email: feng_windlover@163.com
Received: Mar. 19th, 2013 revised: Mar. 21st, 2013; accepted: Apr. 9th, 2013
Copyright © 2013 Feng Pan et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT:
Objective: To explore methods for diagnosis of Abernethy malformation. Methods: 2 cases of Abernethy malformation were collected from 2005 to 2012 and analyzed. Results: Symptoms and signs in patients of Abernethy malformation were lack of specificity. Ultra-sound examination could be used to detect the atresia of portal vein. CTA, MRA and DSA could be accurately used to diagnose and classify Abernethy malformation, which could also be used to estimate the whole malformation of abdominal arteries and veins. Conclusion: Abdominal ultra-sound examination could be a very good screening method for Abernethy malformation’s diagnosis; CTA, MRA and DSA could be used to accurately diagnosis and classify Abernethy malformation.
Keywords: Portal Vein; Congenital Abnormalities
2例Abernethy畸形的诊断分析
潘 峰1,周东风2,Sandya Adevi2,梁惠民1,孔祥泉1
1协和医院放射科,武汉
2协和医院儿科,武汉
Email: feng_windlover@163.com
摘 要:
目的:探讨Abernethy畸形的诊断方法。方法:回顾2005年至2012年共计2例Abernethy畸形患者的诊治情况,并对其进行分析。结果:Abernethy畸形临床表现及体征缺乏特异性,超声检查可以有效的发现门静脉闭锁的情况;CTA、MRA及DSA造影可以对Abernethy畸形进行准确诊断及分型,并可全面评估患者腹腔静脉血管畸形情况。结论:腹部超声检查有助于Abernethy综合征的早期筛查;CTA、MRA及DSA造影均可以作为Abernethy畸形的最佳确诊及分型方法。
收稿日期:2013年3月19日;修回日期:2013年3月21日;录用日期:2013年4月9日
关键词:门静脉;先天发育异常
1. 引言
Abernethy畸形是一种十分罕见的先天性门静脉闭锁伴肝外门体静脉分流畸形[1],目前国内外文献报道的仅30例左右。现对武汉市协和医院2005年至2012年间诊治的2例Abernethy畸形患者进行报道分析。
2. 临床资料
2.1. 一般资料
患者1,女,19岁。因右侧季肋部疼痛2年余,于2005年11月23日入院就诊。患者既往患者偶有全身浮肿症状,无肝炎及其他特殊病史。发育良好,查体未见明显异常体征。血常规检查正常;肝肾功能检查示:TB 36.6 umol/L,ALT 49 U/L,AST 91 U/L,γ-GGT 81 U/L,白蛋白30 g/L,余无异常;AFP正常。既往已报道[2]。
患者2,男,9岁。间断鲜血便1年余,肉眼血尿1月余,于2012年7月14日入院。患儿既往有臀部、盆腔弥漫分布海绵状血管瘤病史,范围大。发育良好,查体示左侧臀部、会阴部及外生殖器局部可见较广泛突出于皮面不规则包块影,质软,无压痛,皮肤颜色正常,余查体未见明显异常。血常规检查示:HGB 87 g/L;肝肾功能正常;AFP正常。
2.2. 辅诊资料
2名患者超声检查均提示肝内glisson鞘增厚,门静脉主干及分支未见;肝内均发现占位性病灶。患者1,CT平扫示肝右叶前下段一直径约5 cm类圆形稍低密度影,中心呈星芒状低密度区,增强扫描示病灶呈周边向中心强化趋势;MRI检查同样发现肝右叶前下段一直径近5 cm大小团状异常信号影;CTA检查及CE-MRA (contrast enhanced MRA)检查均示肠系膜上静脉近端纤细,与脾静脉汇合成细窄的门静脉,门静脉较早分为左右两支,且分支纤细、稀少,可见脾静脉–左肾静脉分流形成;肠系膜下静脉呈异常瘤样扩张、扭曲,并汇入左肾静脉下方下腔静脉[2](图1)。肝占位组织活检示为局灶性结节增生(focal nodular hyperplasia, FNH)。
患者2,MRI平扫 + 增强提示双侧臀部、骶部、会阴部、盆腔内脏器及其周围组织广泛分布异常信号影,T1WI呈高、低混杂信号,T2WI呈高信号,以左侧臀部为主,呈匍匐性生长,边界不清,考虑海绵状血管瘤(图1);扫描所及肝脏、脾脏可见多个异常结节影,肝内及肝门区未见门静脉主干及分支(图2)。CE-MRA检查见腹腔、盆腔内可见一迂曲的巨大血管影,未见正常门静脉显影,考虑门静脉闭锁,伴肠系膜下静脉与下腔静脉门腔分流形成(图2);患儿三支肝静脉通畅。DSA摄影示腹腔干及肠系膜上动脉分别发出一根肝右动脉,且动脉明显增粗;门静脉主干及分支未显影,可见脾静脉与肠系膜上、下静脉汇合至异常增粗扭曲的分流静脉,后者逆流汇合至下腔静脉;肠系膜下动脉造影示降结肠、乙状结肠及直肠区域广泛血管畸形(图3)。
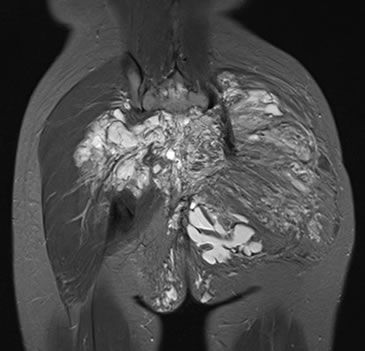
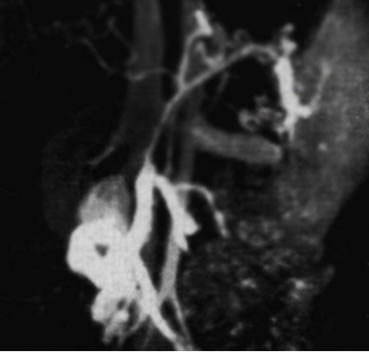
Figure 1. In case 1(left), CE-MRA demonstrated that splenic vein and superior mesenteric vein were converged to slender portal vein, and portal vein is divided into 2 branches with rare and slender intrahepatic vessels. The abnormal carices were imported into gastric coronary vein and left renal vein from the splenic vein. Inferior mesenteric vein was abnormally dilatated and twisted, and then flowed into the left renal vein and inferior vena cava. In case 2(right), MRI scan demonstrated diffused patchy abnormal signals in the subcutaneously gluteal tissue, sacrococcygeal tissue and the perineum with left superiority, which were with nodular, cord shape or cystic forms and creeping growth. The lesion was with obscure boundary and mixed signal in T1WI and high signal in T2WI
图1. 患者1(左图) CE-MRA检查示纤细的脾静脉与肠系膜上静脉汇合成纤细的门静脉,门静脉较早分为左右2支,且肝内分支纤细而稀少,脾静脉汇合前发出异常引流血管与汇入胃冠状静脉及左肾静脉,肠系膜下静脉呈异常瘤样扩张、扭曲,并最终汇入左肾静脉下方下腔静脉。患者2(右图) MRI骨盆平扫示臀部皮下、骶尾部及会阴部见弥漫分布大片状异常信号灶,呈条状、结节状及囊状多形态表现并呈匍匐性生长,边界不清,信号混杂,T1WI呈高、低混杂信号,T2WI呈高信号,病变以左臀部为明显

Figure 2. CE-MRI scan demonstrated atresia of portal vein trunk and intrahepatic branches with normal hepatic vein and inferior vena cava. Multiple nodules were found in liver and spleen by enhanced CT scan, which were moderate enhanced. Volume rendering with vascular reconstruction demonstrated a dilated and tortuous malformated vein linking the dilated left internal iliac vein, dilated splenic vein and superior mesenteric vein, and a abnormal vein beside the ascending colon. No normal portal vein was demonstrated and inferior vena cava was irregularly partial aneurismal dilated
图2. CE-MRI扫描可见肝内门静脉主干及分支均完全闭锁,肝静脉及下腔静脉肝段均发育良好;肝、脾可见多发结节影,增强扫描肝结节影呈中度强化改变;血管重建见腹腔–盆腔内一迂曲的巨大血管影,其下端与迂曲增粗的左侧髂内静脉相连,上端与增粗的脾静脉、肠系膜上静脉相连,升结肠旁见一增粗的血管影与上述巨大畸形血管相连,未见正常门静脉显影;下腔静脉局部呈不规则瘤样扩张

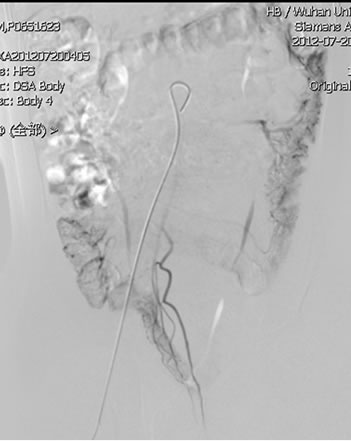
Figure 3. The inferior mesenteric artery DSA angiography showed the right shift with sigmoid colon, and cord stain in descending colon, sigmoid colon and rectum and thick draining vein were emerged in substance phase. Splenic artery DSA angiography showed atresia of portal vein trunk and branche. Splenic vein and superior mesenteric vein were converged to abnormal dilated malformated vein, which flowed into the left iliac vein, passing the inferior vena cava to right atrium
图3. 肠系膜下动脉DSA造影可见,乙状结肠向右方移位,实质期降结肠、乙状结肠及直肠可见不规则条索状染色,可见较粗大回流静脉早显;脾动脉DSA造影示门静脉主干及分支未显影;脾静脉、肠系膜上静脉汇合至异常增粗畸形静脉,最终汇入左侧髂静脉,通过下腔静脉回流至右心房
2.3. 诊断分型
Abernethy畸形临床上分为I型和II型两种[1]。I型:肝脏完全无门静脉血灌注,例如门静脉缺失,胃肠静脉血完全向腔静脉分流;II型:门静脉血部分向肝脏灌注。I型又分Ia和Ib亚型,Ia型:肠系膜上静脉与脾静脉无汇合;Ib型:肠系膜上静脉与脾静脉汇合。
3. 结果
患者1,CTA及MRA检查提示门静脉主干及分支纤细,合并脾静脉–左肾静脉分流及肠系膜下静脉–下腔静脉两种门体分流情况,故诊断Abernethy畸形II型;患者2,MRA及DSA检查示门静脉完全闭锁,且肠系膜上静脉与脾静脉汇合,存在肠系膜下静脉–左髂内静脉门体分流方式,故诊断Abernethy畸形Ib型。
4. 讨论
Abernethy畸形是一种罕见的先天门静脉闭锁畸形伴肝外门体分流情况[1],由Abernethy于1793年首次报道,1997年由Edward对该畸形命名为Abernethy畸形。病因学上考虑与由卵黄静脉系统发育异常相关,肠周卵黄静脉丛有选择性的退化和保留发生异常时,可能会导致门静脉的先天性缺如。
Abernethy畸形临床表现不典型,文献报道的临床症状包括下消化道出血、腹壁静脉曲张等[3,4]。其可能并发有全身多发血管畸形、胆道闭锁及心脏缺陷等情况[5,6]。2例患者起病均十分隐匿,尤其是患者2,因臀部血管瘤于本院复查MRI时意外发现该畸形情况,结合患者DSA造影表现,考虑长期慢性血便及血尿症状与会阴部及结直肠血管畸形导致的出血可能性较大,之前已有文献报告类似症状[4]。因门静脉闭锁畸形情况存在,故Abernethy患者多会出现慢性肝功能受损情况,患者1实验室检查即提示肝功能慢性受损改变;而患者2肝功能正常的原因可能与其肝动脉代偿较好有关。因该病病例报告较为少见,尚缺少预后相关的信息,已经发现的严重并发症包括肺动脉高压、肝脏恶性肿瘤、肝肺综合征和肝性脑病[7-9]。2例患者影像学检查均发现肝占位性病变,其中患者1已行肝占位活检,提示FNH,但仍不除外将来发生肝恶性肿瘤可能。针对Abernethy畸形的治疗,目前尚无定论,肝移植可能是目前已知的根治Abernethy畸形的最有效方法[7]。
因Abernethy畸形临床表现及并发症的非典型性,影像学检查是最重要的诊断方法。其主要影像学表现为:门静脉主干及肝内门静脉闭锁,伴脾静脉、肠系膜上静脉及肠系膜下静脉以各种形式与肾静脉、髂静脉或下腔静脉形成的异常分流道,部分患者可能存在肝外残存门静脉端瘤样改变[10,11]。超声检查可以作为一种有效的诊断方法。2例患者超声检查均提示门静脉主干及分支闭锁情况。但是,超声检查难以全面了解全腹部血管畸形情况,尤其是腹腔静脉分流情况。CTA、MRA及DSA检查均可以清晰全面地显示腹部门静脉系统情况,尤其是腹腔静脉门体分流情况,从而可以预测患者门脉高压性消化道出血可能性及指导相关手术治疗方案。2例患者均存在多种门体分流形式,包括脾静脉–左肾静脉分流、肠系膜下静脉–下腔静脉分流、肠系膜下静脉–左侧髂总静脉分流三种分流形式,且分流量均较大,故临床上尚未出现因门静脉系统高压引起的消化道大出血情况。总之,超声检查作为一种价格相对低廉的检查,可以作为Abernethy综合征的一种早期筛查方法,其提示问题后,进一步的CTA、MRA或DSA检查均可以作为其确诊检查方法。
参考文献 (References)
[1] E. R. Howard, M. Davenport. Congenital extrahepatic portocaval shunts—The Abernethy malformation. Journal of Pediatric Surgery, 1997, 32(3): 494-497.
[2] 黄劲柏, 徐海波, 孔祥泉等. Abernethy畸形一例[J]. 中华放射学杂志, 2006, 40(10): 1112-1113.
[3] 王小川, 王蕾, 贾苍松. Abernethy畸形1例[J]. 中华妇幼临床医学杂志(电子版), 2011, 2: 168-169.
[4] 李震, 汪忠镐, 赵克等. Abernethy畸形致下消化道出血的诊治[J]. 中国普外基础与临床杂志, 2010, 1: 83-84.
[5] C. Ratnasamy, A. Kurbegov, S. Swaminathan. Cardiac anomalies in the setting of the Abernethy malformation of the portal vein. Cardiology in the Young, 2007, 17(2): 212-214.
[6] A. Singhal, A. Srivastava, N. Goyal, et al. Successful living donor liver transplant in a child with Abernethy malformation with biliary atresia, ventricular septal defect and intrapulmonary shunting. Pediatric Transplantation, 2009, 13(8): 1041-1047.
[7] K. Ringe, E. Schirg, M. Melter, et al. Congenital absence of the portal vein (CAPV). Two cases of Abernethy malformation type 1 and review of the literature. Radiologe, 2008, 48(5): 493-502.
[8] M. J. Osorio, A. Bonow, G. J. Bond, et al. Abernethy malformation complicated by hepatopulmonary syndrome and a liver mass successfully treated by liver transplantation. Pediatric Transplantation, 2011, 15(7): E149-E151.
[9] T. Hori, Y. Yonekawa, S. Okamoto, et al. Pediatric orthotopic living-donor liver transplantation cures pulmonary hypertension caused by Abernethy malformation type Ib. Pediatric Transplantation, 2011, 15(3): e47-e52.
[10] A. Kumar, J. Kumar, R. Aggarwal, et al. Abernethy malformation with portal vein aneurysm. Diagnostic and Interventional Radiology, 2008, 14(3): 143-146.
[11] S. H. Chandrashekhara, A. S. Bhalla, A. K. Gupta, et al. Abernethy malformation with portal vein aneurysm in a child. Journal of Indian Association of Pediatric Surgeons, 2011, 16(1): 21-23.