Hans Journal of Ophthalmology
Vol.05 No.04(2016), Article ID:18809,6
pages
10.12677/HJO.2016.54016
Observed Axial Change in Axial High Myopia Eyes after Phacoemulsification
Lilun Chen*, Jionglin Bao, Wenjuan Wang, Guoqi Guan, Jing Zang#
Department of Ophthalmology, The First Affiliated Hospital of Guangdong Pharmaceutical University, Guangzhou Guangdong

Received: Sep. 30th, 2016; accepted: Oct. 24th, 2016; published: Oct. 27th, 2016
Copyright © 2016 by authors and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



ABSTRACT
Objective: To discuss and observe initial axis oculi changes under the condition of no adjustment in patients with high axial myopia, who underwent phacoemulsification of caligo lentis with intraocular lens implantation, so as to provide preliminary ideas and plans for the prevention and treatment of myopia in the future. Methodology: 55 cases (83 eyes) with high axial myopia, who received caligo lentis surgery in our hospital from January 2014 to March 2015, were enrolled, with the average age of 65.15 ± 11.23 (40 to 90) years old. There were 28 males and 27 females. All subjects were received overall examinations on their eyes before the surgery, and the length changes of axis oculi were measured and recorded with partial coherence interferometry (PCI) technique of IOL-Master before and after the surgery, which were compared with those of before operation and 1 day, 7 days, 3 months, and 1 year after operation. Rank sum test on the data of completely randomized design, i.e. Wilcoxon’s rank sum test, was used to analyze changes of axis oculi. Result: In comparison of axis oculi lengths before the surgery, the reduced lengths of axis oculi suggest statistical significance (p < 0.001) 1 day, 1 week, 3 months and 1 year after the surgery; compared with lengths of axis oculi 1 day after the surgery, the decreased lengths of axis oculi indicate statistical significance (p < 0.001) 1 week, 3 months, and 1 year after the surgery; compared with lengths of axis oculi 1 week after the surgery, no statistical significance is observed in the diminished lengths of axis oculi 3 months and 1 year after the surgery; in comparison of axis oculi lengths 3 months after the surgery, no statistical significance is noticed in the increased lengths of axis oculi 1 year after the surgery (p = 0.001). Conclusion: Patients with high axial myopia have shown stable refraction state and changes of axis oculi after the surgery of phacoemulsification with intraocular lens implantation, which is a superior treatment means.
Keywords:High Myopia, Axial Length, IOL-Master, Phacoemulsification

轴性高度近视眼白内障超声乳化术后 眼轴变化观察
陈立伦*,鲍炯琳,王文娟,管国奇,臧晶#
广东药学院第一附属医院眼科,广东 广州

收稿日期:2016年9月30日;录用日期:2016年10月24日;发布日期:2016年10月27日

摘 要
目的:探讨轴性高度近视眼患者,行白内障超声乳化摘除伴人工晶状体植入术后,无调节状态下眼轴变化做初步观察,对未来近视眼防控及治疗领域提供初步思路及设想。方法:收集2014年1月~2015年3月在我院行白内障手术的轴性高度近视眼患者55例83眼,平均年龄65.15 ± 11.23岁(40~90岁),其中男28例、女27例。所有研究对象术前均行眼部全面检查,并应用IOL-Master的部分相干干涉测量(partial coherence interferometry, PCI)技术测量记录术前及术后眼轴长度变化,并将其按术前与术后1天、7天、3个月、1年进行比较。采用完全随机设计资料的秩和检验(Wilcoxon秩和检验)法分析眼轴变化情况。结果:眼轴变化与术前眼轴长度相比,术后1日、术后1周、术后3月和术后1年的眼轴长度减少均具有统计学意义(p < 0.001);与术后1日相比,术后1周、术后3月及术后1年眼轴长度减少均具有统计学意义(p < 0.001);与术后1周相比,术后3月和术后1年眼轴长度减少尚未发现统计学意义;与术后3月相比,术后1年眼轴长度增加无统计学意义(p = 0.001)。结论:轴性高度近视眼患者,经超声乳化伴人工晶体植入术后屈光状态及眼轴变化稳定,是较理想的治疗手段。
关键词 :高度近视,眼轴,IOL-Master,白内障超声乳化

1. 引言
随着白内障小切口超声乳化技术的普及和完善,现已发展到屈光手术的阶段,高度近视合并白内障的患者,在摘除混浊晶体的同时达到矫正屈光的目的,是较理想的治疗手段 [1] 。而术后无调节状态下,患者长期的屈光稳定与否成为病人术后视功能恢复的重要影响因素。因此,我们通过轴性高度近视眼患者行白内障术后,在无调节力状态下眼轴增长情况及屈光变化进行观察,报道如下:
2. 对象和方法
收集2014年1月~2015年3月在我院行白内障手术的轴性高度近视眼患者55例83眼,研究对象年龄40~90岁,平均年龄65.15 ± 11.23岁,其中男28例、女27例,右眼43眼,左眼40眼。入选标准:轴性高度近视眼伴白内障患者(≥−6.0 D);眼轴 ≥ 26 mm;白内障术中、术后无并发症。排除标准:既往眼部手術史(玻璃体切除术、巩膜扣带术、小梁切除術、准分子激光术、飞秒激光术);眼压 ≥ 21 mmHg或青光眼病史;眼外伤、肿瘤、辐射史;屈光介质疾病史(圆锥角膜、玻璃体出血等等)、固视不良等影响检查者;IOL-Master无法进行测量的患者。
所有受检者检查:各项白内障术前常规检查、裸眼视力和最佳矫正视力、眼压、眼前节、眼底散瞳检查、角膜曲率、角膜内皮细胞计数、角膜地形图、电脑自动验光仪及IOL-Master检查,为了避免检测差异,以上均由同一位经验丰富操作者完成检查;白内障超生乳化摘除伴人工晶体植入术,由同一位经验丰富的手术医生完成手术,术中植入Bausch & Lomb Akreos Adapt (A常数:118.4)、Bausch & Lomb Akreos Adapt-AO (A常数:118.3)、Rayner 920H (A常数:118.6)人工晶体;术后1天、7天、3个月、1年回诊复查,用IOL-Master进行眼轴测量、电脑自动验光仪(AR
统计分析应用SPSS13.0统计软件包处理统计资料,分类变量的描述采用百分比,术前屈光,术前散光,角膜k1和角膜k2采用中位数和四分位数进行描述。眼轴长度和屈光采用中位数和四分位数间距进行描述。采用配对资料的秩和检验(Wilcoxon秩和检验)法比较术后1日、术后1周、术后3月、术后1年的眼轴长度与术前眼轴长度,并比较术后1周、术后1年屈光与术前屈光。p值与校正后的p值进行比较。手术前后眼轴长度比较,当p < 0.005有统计学意义;手术前后屈光比较,当p < 0.017时有统计学意义。
3. 结果
(1) 分类变量的描述采用百分比,术前屈光,术前散光,角膜k1和角膜k2采用中位数和四分位数进行描述。男性28例(占50.91%),女性27例(占40.09%)。右眼43例(占51.81%),左眼40例(占48.19%)。术前屈光中位数为3.41 (3.10~3.63) D,术前散光−1.89 (−2.50~−1.00) D,角膜k1为43.55 (42.35~44.47) D,角膜k2为45.00 (43.72~45.73) D,见表1。
(2) 术前,术后1日,术后1周,术后3月和术后1年的眼轴长度分别为27.67 (26.83~29.52) mm,27.55 (26.64~29.33) mm,27.48 (26.57~29.26) mm,27.47 (26.61~29.19) mm,27.49 (26.62~29.20) mm。与术前眼轴长度相比,术后1日、术后1周、术后3月和术后1年的眼轴长度减少均具有统计学意义(p < 0.001);与术后1日相比,术后1周、术后3月及术后1年眼轴长度减少均具有统计学意义(p < 0.001);与术后1周相比,术后3月和术后1年眼轴长度减少尚未发现统计学意义;与术后3月相比,术后1年眼轴长度增加无统计学意义(p = 0.001)。见表2、图1。
术前屈光,术后1周和术后1年屈光中位数分别为−10.85 (−16.7~−7.0) D,−0.66 (−1.29~−0.08) D和−0.82 (−1.29~−0.2) D。与术前屈光相比,术后1周和术后1年的屈光差异有统计学意义(p < 0.001);与术后1周相比,术后1年屈光变化无统计学意义(p = 0.61),见表2、图2。
Table 1. Sample basic situation
表1. 样本的基本情况
4. 讨论
轴性近视是指眼轴进行性增长所导致的病理性屈光不正,好发于30岁以上人群 [1] [2] 。轴性近视的形成归咎于遗传和环境因素。环境因素是近视眼进展的核心要素,其中包括调节和离焦,两者互为因果 [3] 。TROILO和SCHMID等,观察阻断调节后鸡的眼轴变化,结果表明除了调节外尚有其他因素参与眼球增长 [4] [5] 。MORGAN与WINAWER和WALLMAN等的动物实验研究中,发现近视离焦及远视离焦
Table 2. Comparison of ocular axial length and refraction before and after surgery
表2. 手术前后眼轴长度和屈光比较
*采用Wilcoxon符号秩和检验比较手术前后眼轴长度和屈光的变化,p < 0.05/比较次数时有统计学意义;♂表示术后1周、术后3月、术后1年与术后1日眼轴长度比较,术后1周、术后1年与术前屈光比较;♀表示术后3月、术后1年与术后1周眼轴长度进行比较,术后1年与术后1周屈光进行比较;※表示术后1年与术后3月比较
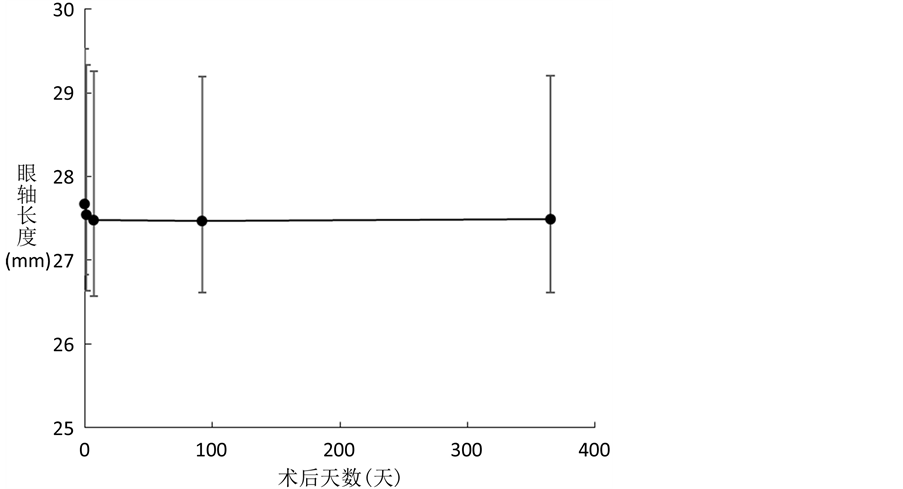
Figure 1. Changes in axial length of the eyes after operation
图1. 术后眼轴长度变化趋势
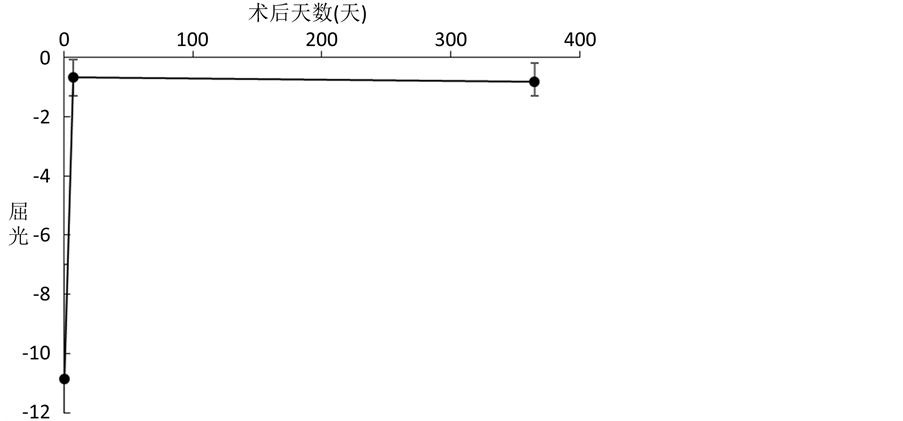
Figure 2. Trend of refractive changes after surgery
图2. 术后屈光变化趋势
均对眼轴变化产生影响,且近视离焦作用比远视离焦强 [3] [6] 。HUANG和SMITH等,指出屈光状态改变并不依赖中心视觉影响,周边形觉剥夺亦可引起近视状态 [7] ,此结论使周边离焦在近视进展中的作用受到重视。在动物模型实验中得到具有参考价值的研究结果,但考虑种属差异及实验对像依从性差 [8] ,我们应在人类身上找出更符合条件的观察模型,以将种属差异及实验配合度等影响因素降至最低。
1944年自STEPHEN BRINT提出了屈光性白内障手术理念后 [9] ,超声乳化技术在临床应用中已逐渐成熟,在摘除浑浊晶状体矫正屈光状态的同时建立无调节状态的观察模型,本研究对此无调节状态下眼轴增长变化进行观察结果示,白内障超声乳化手术后1日眼轴减少幅度最大,与其它时间段眼轴变化相比较有统计学意义(p < 0.001),而术后1周至1年期间眼轴变化趋于稳定状态,各时段比较无统计学意义(p = 0.001),见表2、图1。术后屈光状态在术后1周与术后1年相比较,尽管在图2中可见到随着观察时间的延长,屈光状态有近视漂移趋势,但两者相比较仍无统计学意义(p = 0.61),见表2、图2。
1980年O’DONNELL等研究指出,核性白内障是导致中、青年高度近视眼患者,视力丧失的主要原因 [10] ,这与KUBO等研究结果相同,表明当眼轴长度 > 24 mm和近视度数增加时,容易促使以核性为主的白内障发生 [11] 。随着屈光性白内障超声乳化技术开展至今,通过术前详细检查、术中精细操作及术后定期随访,已将术后并发症出现概率将至最低,在去除调节的同时患者术后长时间的屈光状态稳定,眼轴未见增长趋势,与众多屈光矫正手术相比是较理想的治疗手段。
本研究尚存在不足,如总体样本量较小,尚需增加样本量后结果才更具有代表性。本研究中并未对其它屈光矫正手术后的眼轴进行对比观察评价,这些都是未来我们的研究方向。今后将通过更大样本的多中心研究,将目前临床常用的屈光手术进行术后长时间的追踪观察,根据不同屈光手术所建立的调节、离焦状态对轴性近视眼眼轴变化进行观察,寻找成年轴性高度近视眼患者最佳的预防和治疗方案,对未来轴性高度近视眼防控及治疗提供思路及设想。
文章引用
陈立伦,鲍炯琳,王文娟,管国奇,臧 晶. 轴性高度近视眼白内障超声乳化术后眼轴变化观察
Observed Axial Change in Axial High Myopia Eyes after Phacoemulsification[J]. 眼科学, 2016, 05(04): 89-94. http://dx.doi.org/10.12677/HJO.2016.54016
参考文献 (References)
- 1. 王幼生, 廖瑞端, 刘泉, 甄兆忠. 现代眼视光学[M]. 广州: 广东科技出版社, 2004: 131-134.
- 2. Sayegh, F.N. (2009) Age and Refraction in 46,000 Patients as a Potential Predictor of Refractive Stability after Refractive Surgery. Journal of Refractive Surgery, 25, 747-751. http://dx.doi.org/10.3928/1081597X-20090707-10
- 3. Morgan, I. and Megaw, P. (2004) Using Natural STOP Growth Signals to Prevent Excessive Axial Elongation and the Development of Myopia. Annals Academy of Medicine Singapore, 33, 16-20.
- 4. Schmid, K.L. and Wildsoet, C.F. (1996) Effects on the Compensatory Responses to Positive and Negative Lenses of Intermittent lens Wear and Ciliary Nerve Section in Chicks. Vision Research, 36, 1023-1036. http://dx.doi.org/10.1016/0042-6989(95)00191-3
- 5. Troilo, D., Gottlieb, M.D. and Wallman, J. (1987) Visual Deprivation Causes Myopia in Chicks with Optic Nerve Section. Current Eye Research, 6, 993-999. http://dx.doi.org/10.3109/02713688709034870
- 6. Winawer, J. and Wallman, J. (2002) Temporal Constraints on Lens Com-pensation in Chicks. Vision Research, 42, 2651-2668. http://dx.doi.org/10.1016/S0042-6989(02)00300-0
- 7. Huang, J., Hung, L.F. and Smith III, E.L. (2011) Effects of Foveal Ablation on the Pattern of Peripheral Refractive Errors in Normal and Form-Deprived Infant Rhesus Monkeys (Macaca mulatta). Investigative Ophthalmology, 52, 6428- 6434. http://dx.doi.org/10.1167/iovs.10-6757
- 8. Meng, W.H., Butterworth, J., Malecaze, F. and Calvas, P. (2011) Axial Length of Myopia: A Review of Current Research. Ophthalmologica, 225, 127-134. http://dx.doi.org/10.1159/000317072
- 9. Brint, S.F. (1994) Refractive Cataract Surgery. International Ophthalmology Clinics, 34, 1-11. http://dx.doi.org/10.1097/00004397-199403440-00003
- 10. O’Donnell Jr., F.E. and Maumenee, A.E. (1980) “Unexplained” Visual Loss in Axial Myopia: Cases Caused by Mid Nuclear Sclerotic Cataract. Ophthalmic Surgery, 11, 99-101.
- 11. Kubo, E., Kumamtoto, Y., Tsuzuki, S. and Akagi, Y. (2006) Axial Length, Myopia and Severity of Lens Opacity at the Time of Cataract Surgery. Archives of Ophthalmology, 124, 1586-1590. http://dx.doi.org/10.1001/archopht.124.11.1586
