Asian Case Reports in Surgery
Vol.05 No.04(2016), Article ID:19557,4
pages
10.12677/ACRS.2016.54006
Liver Inflammatory Pseudotumor with “Edema Rime Sign” on CT Scanning: Report of a Case
Hanzhang Huang, Feng Zhou, Zengrong Jia, Pengfei Wang, Zhou Du, Shaoliang Han*
Department of Gastrointestinal Surgery, The First Affiliate Hospital of Wenzhou Medical University, Wenzhou Zhejiang

Received: Jan. 3rd, 2017; accepted: Jan. 15th, 2017; published: Jan. 18th, 2017
Copyright © 2016 by authors and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



ABSTRACT
A 57 years old male patient’s chief complaint is the right epigastric discomfort associated with dull pain, no past history of hepatitis. On physical examination, he was in good general condition, no yellow stain of skin and sclera, soft abdomen with impalpable liver and spleen. Laboratory examination revealed that WBC was 9.0 × 109/L, Hb 97 g/L, serum albumin 33.4 g/L, serum globulin 35.3 g/L, alanine aminotransferase 20 IU/L, alpha-fetoprotein (AFP) 2.6 μg/L (0 - 20.0 μg/L), carcinoembryonic antigen (CEA) 3.0 μg/L, and carbohydrate CA19-9 16 μg/L. Ultrasonography revealed that a hypoechoic tumor about 55 × 47 mm located at left liver, with clear boundary, and uneven the echo in the tumor, and blood stream was detectable, suggesting left liver occupying lesion with the predominance of liver cancer. A tumor of 34 mm with elliptical density rang in the left liver on plain CT scanning, and hypodensity band around the tumor was found, it was enhanced by enhanced CT scanning (“edema rime sign”). The multiple liver and kidney cyst were also found, and the diagnosis was left liver occupying lesion with the predominance of liver cancer, with multiple liver and kidney cyst. An irregular hepatectomy was performed under general anesthesia, and a tumor about 6.5 cm in diameter was found in the left liver, with gray surface and clear boundary. The postoperative histopathology demonstrated an amount of lymphocytes and plasma cells infiltration in the tumor and hyperplasia of fibrous tissues. The recovery after surgery was smoothly, and there was no recurrence case on 10-year follow-up.
Keywords:Inflammatory Pseudotumor, Liver, Edema Rime Sign

CT表现为“水肿环征”的肝脏炎性假瘤: 一例报道
黄瀚章,周锋,贾曾荣,王鹏飞,杜舟,韩少良*
温州医学院附属第一医院胃肠外科,浙江 温州

收稿日期:2017年1月3日;录用日期:2017年1月15日;发布日期:2017年1月18日

摘 要
男,57岁,主诉右上腹不适伴右肝区隐痛1个月,既往无肝炎。体检:一般情况良好,皮肤巩膜无黄染,腹软,肝脾未触及。化验:WBC 9.0 × 109/L,Hb 97 g/L,白蛋白33.4 g/L,球蛋白35.3 g/L,丙氨酸转氨酶20 IU/L。甲胎蛋白(AFP) 2.6 μg/L (0~20.0 μg/L)、癌胚抗原(CEA) 3.0 μg/L、糖类抗原CA19-9 16 μg/L。B超检查见左肝内叶有55 × 47 mm大小低回声团块,境界尚清楚,其内部回声不均匀,可探及动脉型血流信号,提示左肝占位性病变、肝癌首先考虑。CT扫描提示左肝内叶可探及34 mm椭圆形等密度灶,病灶周边见环形低密度带,增强扫描后更为清楚(“水肿环征”),余肝内多发小囊状低密度影,左肾也见小囊肿,诊断为左肝内占位性病变(肝癌首先考虑)、右肝多发小囊肿及左肾小囊肿。全身麻醉下剖腹探查行不规则肝切除,术中见左肝内叶有一个6.5 cm大小肿物,表面呈灰白色,边界清楚。术后病理组织学检查见大量淋巴细胞和浆细胞浸润以及纤维肉芽组织增生,符合炎性假瘤。术后恢复顺利,随诊10年无复发。
关键词 :炎性假瘤,肝脏,水肿环征

1. 病例报告
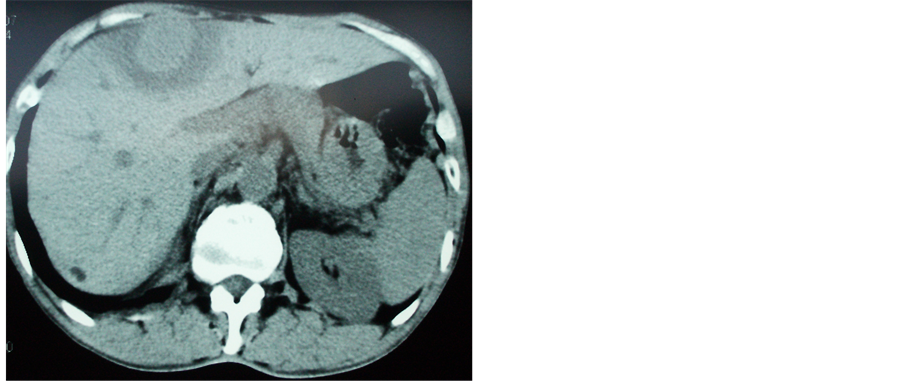
男,57岁,2007年11月因右上腹不适伴右肝区隐痛1个月,在外院实施查B超检查提示右肝内实质性占位,考虑肝脏肿瘤,转入我院。患者既往体健,无肝炎、结核病及牧区生活史。体检:体温37.4℃,一般情况良好,皮肤巩膜无黄染,表浅淋巴结未触及,腹软,肝脾未触及,移动性浊音(-)。化验:WBC 9.0 × 109/L,Hb 97 g/L,血沉25 mm/h,总蛋白68.3 g/L,白蛋白33.4 g/L,球蛋白35.3 g/L,丙氨酸转氨酶20 IU/L。大便常规,培养正常,潜血阴性。甲胎蛋白(AFP) 2.6 μg/L (0~20.0 μg/L)、癌胚抗原(CEA) 3.0 μg/L (0~5.0 μg/L)、糖类抗原CA19-9 16 μg/L (0~37.0 μg/L)。B超检查见左肝内叶有55 × 47 mm大小低回声团块,境界尚清楚,其内部回声不均匀,可探及动脉型血流信号,提示左肝占位性病变、肝癌首先考虑。CT扫描提示左肝内叶可探及34 mm椭圆形等密度灶,病灶周边见环形低密度带(图1(a)),增强扫描后更为清楚(“水肿环征”) (图1(b)),增强后动脉期强化不明显,门脉期及延迟期呈持续等强化,余肝内多发小囊状低密度影,无明显强化,左肾也见小囊肿,诊断为左肝内占位性病变(肝癌首先考虑)、右肝多发小囊肿及左肾小囊肿。

 (a) (b)
(a) (b)
Figure 1. A round-like lesion was found at the left lobe of the liver on plain CT scanning, with hypodensity band around the tumor presented as “edema rime sign” (a), and the “edema rime sign” became more clear on enhanced CT (b)
图1. 肝脏炎性假瘤CT扫描所见:平扫见左肝内叶类圆形病灶,周边环状低密度带表现为“水肿环征”(a);增强后“水肿环征”更清晰(b)

Figure 2. A tumor about 6.5 cm in size was found in the left liver, with gray surface and clear boundary
图2. 肝脏炎性假瘤术中照片:肝脏左肝内叶可见一个约6.5 cm大小、灰白色、边界清楚的质硬肿块
浆细胞浸润以及纤维肉芽组织增生,符合炎性假瘤。术后恢复顺利,随诊10年无复发。
2. 讨论
肝脏炎性假瘤(inflammatory pseudotumor of the liver, IPL)是由各种致炎因子引起的肝脏局部组织炎性细胞浸润、凝固坏死、肉芽肿形成和纤维组织增生为病理特征的肿瘤样病变,较为少见 [1] [2] [3] [4] 。本病确切病因不清,目前多认为与感染、自身免疫、血管病变和过敏等有关 [1] [2] 。影像学检查仍是IPL的主要诊断手段,由于此炎性肿块术前定性诊断困难,在临床上易与恶性肿瘤相混淆。据报告此病误诊率大于90%,最终确诊依据为病理学检查 [3] [4] 。B超多表现为低回声病灶、边界可辨、内部回声不均,多无声晕,部分病例可见管道样结构穿过其中。CT平扫时IPL多表现为边界不清的低密度灶,密度不均匀;而在增强扫描的门脉期及延迟期扫描时出现病灶边缘强化,因炎性假瘤周边有较多的纤维组织包绕,个别病灶因周边纤维组织较多,强化后和肝实质密度一致,因而可产生病灶缩小的感觉 [2] [3] [4] 。本例CT扫描表现为病变中央低密度不规则增强,病灶周边可见环形低密度带,且增强扫描显示更为清楚的“水肿环征”非常少见,需要与肝癌、肝血管瘤、肝脓肿及肝腺瘤等相鉴别。
由于IPL缺乏特异的临床和影像学表现,作者认为以下几点应考虑为肝脏炎性假瘤的可能:① 一般病程较长,症状较轻,全身情况好,可伴有不明原因的发热;② 多数无肝炎、肝硬化病史,肝功能和AFP正常;③ B超多表现为低回声实性肿块,边界清楚,有时可见包膜。CT平扫多为边界不清的低密度区、密度不均匀,动态增强扫描在门静脉期及延迟期病灶边缘强化,部分病例可伴有闭塞性静脉炎;④ B超和CT可见门静脉支穿过或包绕病灶,呈闭塞性静脉炎表现;⑤ B超或CT引导下穿刺活检为纤维组织和慢性炎性细胞为主,无肿瘤细胞 [1] [2] [3] [4] [5] 。Kawaguchi等 [3] 报道经皮肝脏穿刺活检确诊肝脏及脾脏炎性假瘤、并应用类固醇激素治愈一例。
由于本病定性诊断困难,手术切除仍是目前首选的治疗方法,具体手术方式应根据病灶位置及范围而定,可行局部切除或肝叶、段切除。但如果术前获得确诊,可采取非手术治疗(如环孢霉素A、糖皮质激素、抗生素治疗)使炎性假瘤病灶缩小 [2] [3] [4] [5] 。Park等 [4] 收集多中心治疗的45例肝脏炎性假瘤,其中外科切除10例及保守治疗(激素 ± 抗生素) 35例,全部治愈。
本病预后良好,并有文献报道可自行消退 [6] ,但也有切除术后复发的报道。
文章引用
黄瀚章,周 锋,贾曾荣,王鹏飞,杜 舟,韩少良. CT表现为“水肿环征”的肝脏炎性假瘤:一例报道
Liver Inflammatory Pseudotumor with “Edema Rime Sign” on CT Scanning: Report of a Case[J]. 亚洲外科手术病例研究, 2016, 05(04): 28-31. http://dx.doi.org/10.12677/ACRS.2016.54006
参考文献 (References)
- 1. Obana, T., Yamasaki, S., Nishio, K., et al. (2015) A Case of Hepatic Inflammatory Pseudotumor Protruding from the Liver Surface. Clinical Journal of Gastroenterology, 8, 340-344. https://doi.org/10.1007/s12328-015-0605-8
- 2. Al-Hussaini, H., Azouz, H. and Abu-Zaid, A. (2015) Hepatic Inflammatory Pseudotumor Presenting in an 8-Year-Old Boy: A Case Report and Review of Literature. World Journal of Gastroenterology, 21, 8730-8738. https://doi.org/10.3748/wjg.v21.i28.8730
- 3. Kawaguchi, T., Mochizuki, K., Kizu, T., et al. (2012) Inflammatory Pseudotumor of the Liver and Spleen Diagnosed by Percutaneous Needle Biopsy. World Journal of Gastroenterology, 18, 90-95. https://doi.org/10.3748/wjg.v18.i1.90
- 4. Park, J.Y., Choi, M.S., Lim, Y.S., et al. (2014) Clinical Features, Image Findings, and Prognosis of Inflammatory Pseudotumor of the Liver: A Multicenter Experience of 45 Cases. Gut and Liver, 8, 58-63. https://doi.org/10.5009/gnl.2014.8.1.58
- 5. Chen, C.B., Chou, C.T., Hsueh, C., et al. (2013) Hepatic Inflammatory Pseudotumor Mimicking Hepatocellular Carcinoma. Journal of the Chinese Medical Association, 76, 299-301. https://doi.org/10.1016/j.jcma.2013.01.004
- 6. Yamaguchi, J., Sakamoto, Y., Sano, T., et al. (2007) Spontaneous Regression of Inflammatory Pseudotumor of the Liver: Report of Three Cases. Surgery Today, 37, 525-529. https://doi.org/10.1007/s00595-006-3433-0
NOTES
*通讯作者。