Advances in Clinical Medicine
Vol.
13
No.
11
(
2023
), Article ID:
76245
,
5
pages
10.12677/ACM.2023.13112591
1例非功能性盆腔神经内分泌肿瘤的病例报告
张舒瑶1,李建辉2*
1西安医学院研究生院,陕西 西安
2陕西省人民医院肿瘤外科,陕西 西安
收稿日期:2023年10月28日;录用日期:2023年11月23日;发布日期:2023年11月29日

摘要
神经内分泌肿瘤是一种较为罕见的肿瘤类型,与肿瘤发生的位置无关,由肿瘤细胞起源的细胞种类有关,通常由能分泌多肽激素的神经内分泌细胞构成,肿瘤的临床症状通常与其的压迫部位及分泌的激素的不同而存在较大差异,压迫症状通常与压迫部位有关,包括腹胀腹痛、咳嗽气喘及尿频尿急等相关症状;激素分泌过度症状通常较为复杂,包括卓–艾综合征、肌无力综合征及库欣综合征等,在怀疑可能存在神经内分泌瘤时可通过CT、B超及相关激素血清含量进行诊断。非功能性神经内分泌瘤症状较轻,疾病指向性不明显,往往需要病理活检后才能诊断。外科手术治疗是神经内分泌瘤的主要治疗手段,手术的方式根据不同的肿瘤部位、大小及病理情况而定,本文报道1例我院收治的盆腔神经内分泌肿瘤临床治疗过程并进行文献回顾,为同道提供参考。
关键词
神经内分泌瘤,诊断,治疗

A Case Report of Nonfunctional Pelvic Neuroendocrine Tumor
Shuyao Zhang1, Jianhui Li2*
1Graduate School of Xi’an Medical University, Xi’an Shaanxi
2Cancer Surgery Department of Shaanxi Provincial People’s Hospital, Xi’an Shaanxi
Received: Oct. 28th, 2023; accepted: Nov. 23rd, 2023; published: Nov. 29th, 2023

ABSTRACT
Neuroendocrine tumor is a rare tumor type, which has nothing to do with the location of the tumor, but is related to the cell type from which the tumor cells originated. It is usually composed of neuroendocrine cells that can secrete polypeptide hormones, and the clinical symptoms of the tumor are usually quite different from the compression sites and hormones secreted. The compression symptoms are usually related to the compression site, including abdominal distension, abdominal pain, cough, asthma, frequent urination and urgency. The symptoms of hypersecretion of hormones are usually complex, including Zollinger-Ellison syndrome, Lambert-Eaton Myasthenic Syndrome and Cushing syndrome, etc. When neuroendocrine tumors are suspected, CT scan, B-ultrasound and serum levels of related hormones can be diagnosed. The symptoms of non-functional neuroendocrine tumors are mild, the disease orientation is not obvious, and need to be diagnosed after pathological biopsy. Surgical treatment is the main treatment for neuroendocrine tumors, and the surgical method depends on different tumor locations, sizes and pathological conditions. This paper reports the clinical treatment process of a pelvic neuroendocrine tumor admitted to our hospital and reviews the literature, so as to provide reference for fellow practitioners.
Keywords:Neuroendocrine Tumor, Diagnosis, Treatment

Copyright © 2023 by author(s) and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/


1. 病例资料
患者,男,47岁,因“检查发现盆腔占位1月余”入住陕西省人民医院泌尿外科。患者1月前体检时B超提示:盆腔腹腔腹膜后间隙以囊为主,囊实混合回声包块,大小约14.9*13 cm,边界清,暗区内可见分隔光带及密集弱光点回声及团絮状中强回声,CDFI示周边可见少许点条状血流信号,考虑:1) 骶前囊肿,2) 畸胎瘤或其他占位性病变,建议进一步检查。未诉特殊不适感,无头晕、头疼,无尿频、尿急及尿痛,无寒战、发热,无腰酸、腰痛,无晕厥、黑朦。入院诊断为:盆腔占位待查。入院后完善相关检查,血常规、肝肾功能、肿瘤系列、胸苷激酶I、心电图、胸部CT、心脏彩色超声、上腹部彩超、肺功能提示异常。上下腹部 + 盆腔CT增强示:腰骶椎前、腹主动脉分叉下方囊实性占位,考虑肿瘤性病变(神经源性肿瘤?) (见图1)。检测血压及血糖在正常范围内波动,未见高血压或低血压症状,未见高血

Figure 1. Preoperative CT in patients with pelvic neuroendocrine tumors revealed cystic and solid space occupying lesions in the presacral region of the lumbar spine
图1. 盆腔神经内分泌肿瘤患者术前CT提示腰椎骶前可见囊实性占位
糖或低血糖症状。胃泌素、多巴胺、去甲肾上腺素及肾上腺素水平均未提示异常。超声造影提示:骶前囊实性包块,二维结合超声造影,考虑占位性病变(其内无灌注实性成分,考虑无活性组织,血凝块?囊腔内液体稠厚,合并出血?)。于2022年08月05日在全麻下行机器人辅助腹膜后肿瘤切除术 + 广泛肠粘连松解术。术中可见骶骨前方一15 cm囊性占位(见图2),位于膀胱后方,表面光滑,肿物底部与骶骨关系紧密。手术后病理提示:(盆腔)神经内分泌肿瘤,核分裂像1个/10HPF,并见小灶坏死。免疫组化:CK (+)、Vimentin (−)、Syn (+)、CgA少数(+)、CD56弱(+)、CR (−)、MC少数(+)、SATB2 (−)、SF-1 (−)、SSTR2 (1+)、Ki-67指数约2%。结合患者临床症状、检验检查结果及病理考虑诊断:非功能性盆腔神经内分泌肿瘤(见图3)。
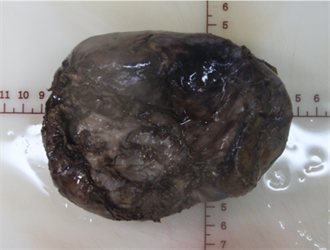
Figure 2. Patients with pelvic neuroendocrine tumors had an intraoperative tumor volume of 14*11*5 cm, which was cystic and solid
图2. 盆腔神经内分泌肿瘤患者术中肿瘤体积14*11*5 cm,呈囊实性
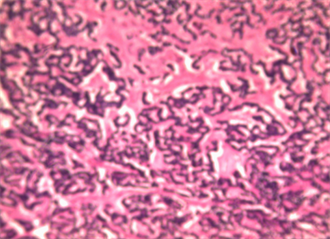
Figure 3. Under the light microscope, the cancer cells were arranged in nests
图3. 光镜下可见癌细胞呈巢团状排列
2. 讨论
神经内分泌肿瘤(neuroendocrine neoplasm, NEN)是一种起源于肽能神经元或神经内分泌细胞的肿瘤,在临床工作中是一种较为少见的肿瘤类型,它可以分泌一些生物活性胺或是多肽激素。NEN在全身多处器官或组织中均可发生,而在消化系统中,尤其是胃肠胰腺处好发,约占发生率的70%,其次是呼吸系统,约占发生率的25%,其他系统的发生率合计为5% [1] [2] 。其临床症状根据分泌激素的不同而相差各异,NEN可表现为惰性、缓慢生长的良性肿瘤,也可表现为低度恶性的肿瘤,也有高转移性、显著恶性的肿瘤,根据激素分泌及患者症状的有无,将其分为功能性神经内分泌肿瘤和非功能性神经内分泌肿瘤。
NEN的诊断需要结合临床症状、影像学和病理学等检查,电子计算机断层扫描仪器(CT)或磁共振成像(MRI)是评估患者病情及判断手术与否的基本影像学技术 [3] [4] ,CT/MRI能检出肿块的大小、与周围血管、器官的关系,有无淋巴结的转移。在一些分化差、侵袭性强的神经内分泌癌中,常采用18F-FDG PET-CT等灵敏度较高的方式诊断 [5] 。病理免疫组织化学是确诊NEN的重要指标 [6] [7] ,常见病理类型有胰岛素瘤和胃泌素瘤,一些较为罕见的病例类型包括胰高血糖素瘤、生长抑素瘤、血管活性肽瘤(VIP瘤)、ACTH瘤及一些无功能性NEN。
临床上NEN通常被视为一种罕见疾病,随着近年来诊疗水平的提高,NEN的检出率逐年上升, [8] Yao JC进行的回顾性研究表明,NEN的发病率升至5.25/10万。根据世界卫生组织2019年发布的第5版分类和分级标准,通过核分裂象数及Ki~67指数可将神经内分泌肿瘤可分为低级别G1期、中级别G2期和高级别G3期 [9] 。G1期分化程度最好,最安全,进展慢,不容易转移,本身恶性程度低;G2期分化程度较高,也比较安全,本身恶性程度低,不容易转移,进展慢;G3期分化程度较低,恶性程度较高,进展迅速 [10] 。
手术治疗是NEN最主要的治疗方案,手术目的旨在尽可能减少肿瘤负荷及激素分泌引起的症状,手术方案则需要综合评估肿瘤大小、部位及与周围血管、器官的关系后确定。以NEN中较为常见的胰岛素瘤为例,在肿瘤大小 < 2 mm,且肿瘤位置较为表浅,可保留主胰管时,应尽量选择在超声或CT引导下行腹腔镜下肿物剜除术;肿瘤位置较深,可根据肿瘤的部位行腹腔镜下胰腺部分切除术;在肿瘤大小 > 2 cm或有恶性倾向的NEN,无论有功能与否,均应行根治性切除术 + 周围淋巴结清扫,对少数特殊病例可行胰十二指肠切除术 [11] 。
对于手术后的NEN患者,可以通过肿瘤标志物检测肿瘤负荷的变化或预后的标志,临床上最常用的肿瘤标志物是嗜铬粒蛋白A (CgA) [12] [13] ,在小肠NEN中,血浆CgA可以作为判断其预后的主要指征 [14] ,复查血浆CgA时出现轻微波动是正常现象,在复查血浆CgA水平增加超过既往水平的25%时应警惕复发可能,重测CgA结果不变或仍升高后,建议使用CT/MRI明确有无肿瘤复发或进展 [15] 。
本文案例患者以发现盆腔占位入院,无特异性临床表现及不适症状,术前超声造影提示:骶前囊实性包块,考虑占位性病变;盆腔增强CT示:神经源性肿瘤可能。由于患者并未出现相关激素升高等不适症状,且入院检查血压血糖等未提示异常,因此除儿茶酚胺外并未完善其余激素检查。结合影像学检查及检验结果,最终确定手术术式为机器人辅助腹膜后肿瘤切除术 + 广泛肠粘连松解术,术中可见肿瘤与骶骨关系紧密,为避免手术后复发风险,请普外科主任术中会诊协助手术后完整切除肿物,加固并缝合骶骨表面。根据手术中所见及术后病理结果,该患者符合神经内分泌瘤诊断标准。术后1年随访,患者健在,未见肿瘤复发。
该病例是一例罕见的无功能性NEN,通过患者肿瘤的诊疗过程也使我们认识到了对疾病认识的不足之处。由于NEN的发病率较低,且无功能性神经内分泌肿瘤没有功能性肿瘤分泌激素的指向性,因此诊断时较易忽略。 [16] Simron Singh在2017年的国际调查中发现,无功能性神经内分泌肿瘤也会在出现一些非特异性症状,如胃炎、焦虑及肠易激综合征等,通常会被归于其他诊断之中,在患者出现相关症状时,应尽早完善相关检查,避免延误诊断。
文章引用
张舒瑶,李建辉. 1例非功能性盆腔神经内分泌肿瘤的病例报告
A Case Report of Nonfunctional Pelvic Neuroendocrine Tumor[J]. 临床医学进展, 2023, 13(11): 18448-18452. https://doi.org/10.12677/ACM.2023.13112591
参考文献
- 1. Klöppel, G. (2017) Neuroendocrine Neoplasms: Dichotomy, Origin and Classifications. Visceral Medicine, 33, 324-330. https://doi.org/10.1159/000481390
- 2. Pan, W.-X., Zhang, X.-M., Hao, S.-L., et al. (2023) Progress in Immuno-therapy for Neuroendocrine Neoplasm of the Digestive System. World Journal of Gastroenterology, 29, 4174-4185. https://doi.org/10.3748/wjg.v29.i26.4174
- 3. Singh, S., Asa, S.L., Dey, C., et al. (2016) Diagnosis and Manage-ment of Gastrointestinal Neuroendocrine Tumors: An Evidence-Based Canadian Consensus. Cancer Treatment Reviews, 47, 32-45. https://doi.org/10.1016/j.ctrv.2016.05.003
- 4. Ambrosini, V., Kunikowska, J., Baudin, E., et al. (2021) Consen-sus on Molecular Imaging and Theranostics in Neuroendocrine Neoplasms. European Journal of Cancer, 146, 56-73. https://doi.org/10.1016/j.ejca.2021.01.008
- 5. 高雨菡, 王萱, 薛华丹. 影像学在神经内分泌肿瘤合并肝转移患者早期治疗评价中的作用: 从解剖学到功能学[J]. 中国医学科学院学报, 2021, 43(6): 956-961.
- 6. Mete, O. and Wenig, B.M. (2022) Update from the 5th Edition of the World Health Organization Classification of Head and Neck Tumors: Overview of the 2022 WHO Classification of Head and Neck Neuroendocrine Neoplasms. Head and Neck Pa-thology, 16, 123-142. https://doi.org/10.1007/s12105-022-01435-8
- 7. Duan, K. and Mete, O. (2016) Algorithmic Approach to Neuroendocrine Tumors in Targeted Biopsies: Practical Applications of Immunohistochemical Markers. Cancer Cytopathology, 124, 871-884. https://doi.org/10.1002/cncy.21765
- 8. Yao, J.C., Hassan, M., Phan, A., et al. (2008) One Hundred Years after “Carcinoid”: Epidemiology of and Prognostic Factors for Neuroendocrine Tumors in 35,825 Cases in the United States. Journal of Clinical Oncology, 26, 3063-3072. https://doi.org/10.1200/JCO.2007.15.4377
- 9. La Rosa, S. and Uccella, S. (2020) Classification of Neuroendo-crine Neoplasms: Lights and Shadows. Reviews in Endocrine and Metabolic Disorders, 22, 527-538. https://doi.org/10.1007/s11154-020-09612-2
- 10. Cui, J., Zhang, Y., Ren, X., et al. (2021) TBX1 Functions as a Tumor Activator in Prostate Cancer by Promoting Ribosome RNA Gene Transcription. Frontiers in Oncology, 10. https://doi.org/10.3389/fonc.2020.616173
- 11. 徐建明, 梁后杰, 秦叔逵, 等. 中国胃肠胰神经内分泌肿瘤专家共识(2016年版) [J]. 临床肿瘤学杂志, 2016, 21(10): 927-946.
- 12. Janson, E.T., Holmberg. L., Stridsberg. M., et al. (1997) Carcinoid Tumors: Analysis of Prognostic Factors and Survival in 301 Patients from a Referral Center. Annals of Oncology, 8, 685-690. https://doi.org/10.1023/A:1008215730767
- 13. Jensen, K.H., Hilsted, L., Jensen, C., et al. (2012) Chromogranin A is a Sensitive Marker of Progression or Regression in Ileo-Cecal Neuroendocrine Tumors. Scandinavian Journal of Gastroenterology, 48, 70-77. https://doi.org/10.3109/00365521.2012.733953
- 14. Welin, S., Stridsberg, M., Cunningham, J., et al. (2009) Ele-vated Plasma Chromogranin A Is the First Indication of Recurrence in Radically Operated Midgut Carcinoid Tumors. Neuroendocrinology, 89, 302-307. https://doi.org/10.1159/000179900
- 15. Arnold, R., Wilke, A., Rinke, A., et al. (2008) Plasma Chromogranin A as Marker for Survival in Patients with Metastatic Endocrine Gastroenteropancreatic Tumors. Clinical Gastroenterology and Hepatology, 6, 820-827. https://doi.org/10.1016/j.cgh.2008.02.052
- 16. Singh, S., Granberg, D., Wolin, E., et al. (2016) Patient-Reported Burden of a Neuroendocrine Tumor (NET) Diagnosis: Results From. JCO Global Oncology, 3, 43-53. https://doi.org/10.1200/JGO.2015.002980
NOTES
*通讯作者。