Advances in Clinical Medicine
Vol.
13
No.
12
(
2023
), Article ID:
78434
,
14
pages
10.12677/ACM.2023.13122878
改良Karlsson术治疗踝外侧副韧带急性与慢性损伤的疗效对比
匡鑫1*,孟晔2#
1青岛大学医学部,山东 青岛
2青岛市市立医院运动医学科,山东 青岛
收稿日期:2023年11月25日;录用日期:2023年12月19日;发布日期:2023年12月29日

摘要
目的:探讨改良Karlsson术治疗踝关节外侧副韧带急性与慢性损伤的临床疗效对比。方法:回顾性研究我院于2020年6月至2022年6月收治的75例踝外侧副韧带损伤手术患者,按照首次受伤至手术时间分为慢性损伤组36例、急性损伤组39例,两组均采用改良Karlsson术解剖修复踝关节外侧副韧带,对比手术前后影像学资料以及AOFAS、VAS及Karlsson踝关节功能评分进行评估,对比其临床疗效。结果:两组患者均获得1年以上随访,随访期间均未发生感染、神经损伤及踝关节活动障碍等并发症。末次随访时,两组患者的满意度均较高,未出现不满意或疗效差的患者,两组之间比较差异无统计学意义(P > 0.05)。两组患者的AOFAS评分、VAS评分及Karlsson评分均较术前明显改善,差异有统计学意义(P < 0.05),相应时间节点,两组之间比较差异无统计学意义(P > 0.05)。测量两组患者的距骨倾斜角及距骨前移距离,末次随访时均较术前明显改善,差异有统计学意义(P < 0.05),两组患者之间比较,差异无统计学意义(P > 0.05)。在相应时间节点,比较两组患者的重返日常生活比例及重返运动比例,差异无统计学意义(P > 0.05)。结论:改良Karlsson术治疗踝外侧副韧带急性与慢性损伤均可取得满意的临床疗效,且急性损伤与慢性损伤的临床疗效对比没有明显差异。
关键词
改良Karlsson术,踝外侧副韧带,急性,慢性

Comparison of the Therapeutic Effects of Modified Karlsson Procedure on Acute and Chronic Injuries of the Lateral Collateral Ligament of the Ankle
Xin Kuang1*, Ye Meng2#
1Medical Department, Qingdao University, Qingdao Shandong
2Department of Sports Medicine of Qingdao Municipal Hospital, Qingdao Shandong
Received: Nov. 25th, 2023; accepted: Dec. 19th, 2023; published: Dec. 29th, 2023

ABSTRACT
Objective: To explore the clinical efficacy comparison of modified Karlsson procedure in the treatment of acute and chronic injuries to the lateral collateral ligament of the ankle. Method: A retrospective study was conducted on 75 patients with lateral collateral ligament injury of the ankle who underwent surgery in our hospital from June 2020 to June 2022. They were divided into a chronic injury group of 36 cases and an acute injury group of 39 cases according to the time from the first injury to the surgery. Both groups used the modified Karlsson procedure for anatomical repair of the lateral collateral ligament of the ankle, Compare preoperative and postoperative imaging data, as well as AOFAS, VAS, and Karlsson ankle joint function scores, to evaluate their clinical efficacy. Result: Both groups of patients were followed up for more than 1 year, and no complications such as infection, nerve injury, or ankle joint dysfunction occurred during the follow-up period. At the last follow-up, the satisfaction of both groups of patients was high, and there were no patients who were dissatisfied or had poor efficacy. There was no statistically significant difference between the two groups (P > 0.05). The AOFAS score, VAS score, and Karlsson score of the two groups of patients were significantly improved compared to before surgery, with a statistically significant difference (P < 0.05). At the corresponding time point, there was no statistically significant difference between the two groups (P > 0.05). The talus inclination angle and talus anterior displacement distance of the two groups of patients were measured. At the last follow-up, there was a significant improvement compared to before surgery, and the difference was statistically significant (P < 0.05). There was no statistically significant difference between the two groups of patients (P > 0.05). At the corresponding time nodes, there was no statistically significant difference in the proportion of patients returning to daily life and returning to exercise between the two groups (P > 0.05). Conclusion: The improved Karlsson procedure can achieve satisfactory clinical efficacy in the treatment of acute and chronic injuries to the lateral collateral ligament of the ankle, and there is no significant difference in clinical efficacy between acute and chronic injuries.
Keywords:Modified Karlsson Procedure, Lateral Collateral Ligament of Ankle, Acute, Chronic

Copyright © 2023 by author(s) and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/


1. 引言
踝关节扭伤是一种常见的运动性损伤,占所有运动损伤性疾病的15%~20% [1] ,尤以跖屈内翻性损伤多见 [2] ,进而导致踝关节外侧副韧带受损,严重时会出现踝外侧副韧带的部分或完全撕裂。踝外侧副韧带由距腓前韧带(Anterior Talofibular Ligament, ATFL)、跟腓韧带(Calcaneal Fibular Ligament, CFL)及距腓后韧带(Posterior Talofibular Ligament, PTFL)组成 [3] ,以距腓前韧带损伤多见,约占90%,其次为距腓前韧带和跟腓韧带的复合型损伤,距腓后韧带损伤罕见 [4] 。急性踝关节扭伤首选冰敷、制动、功能训练及石膏绷带等保守治疗,约80%能够取到较好的治疗效果,但仍有约20%的急性损伤患者会进展为慢性踝关节外侧不稳(Chronic Ankle Instability, CAI),出现踝外侧疼痛、肿胀、反复扭伤、易疲劳及“打软腿”等慢性损伤表现,进一步损伤软骨组织,发展为创伤性关节炎或继发性粘连性关节炎 [5] [6] 。解剖修复距腓前韧带或跟腓韧带仍是当前治疗踝外侧副韧带损伤的标准术式,以改良Karlsson术为代表 [7] [8] 。有相关研究表明,用该术式修复急性损伤的新鲜韧带与慢性持续性损伤的陈旧性韧带,两者术后的临床疗效存在争议。故本研究采用改良Karlsson术治疗踝外侧副韧带损伤,以进一步探讨该术式的可行性及临床疗效,同时比较急性与慢性损伤患者的疗效差异。
2. 临床资料
2.1. 纳入与排除标准
2.1.1. 纳入标准
1) 有明确的踝关节外伤史;
2) 踝外侧疼痛、肿胀,影响活动,踝关节不稳感;
3) 术前踝关节应力位X片下距骨倾斜角或距骨前移距离(+) (见图1),尤以在麻醉下,前抽屉试验或内翻应力试验(+);
4) MR提示距腓前韧带或跟腓韧带撕裂或完全断裂(见图2);
5) 改良Karlsson术。

Figure 1. (A) Talus inclination angle; (B) Distance of talus forward movement
图1. (A) 距骨倾斜角;(B) 距骨前移距离

Figure 2. (A) Tear of the anterior talofibular ligament; (B) Tear of calcaneal ligament
图2. (A) 距腓前韧带撕裂;(B) 跟腓韧带撕裂
2.1.2. 排除标准
1) 严重的踝关节骨折或合并有周围血管、神经及肌腱损伤;
2) 既往有踝关节周围手术史;
3) 功能性踝关节不稳;
4) 全身韧带松弛综合征;
5) 身体状态差,不能耐受手术者;
6) 临床资料不全者。
2.2. 一般资料
回顾性分析我院于2020年6月至2022年6月收治的踝关节外侧副韧带损伤的100例患者,根据纳入与排除标准,将75例患者纳入本研究。根据初次受伤至手术时间,将其分为慢性损伤组(病史 ≥ 3个月)与急性损伤组(病史 < 3个月)。慢性组共36例,其中男26例,女10例;平均年龄为34.7 ± 13.2岁(14~72)岁;左踝19例,右踝17例;单独ATFL损伤12例,ATFL合并CFL损伤21例,ATFL合并CFL及PTFL损伤3例。急性组共39例,其中男22例,女17例;平均年龄为33.1 ± 15.7岁(8~66)岁;左踝24例,右踝15例;单独ATFL损伤18例,ATFL合并CFL损伤20例,ATFL合并CFL及PTFL损伤1例。两组患者一般资料见表1和表2,两组比较差异无统计学意义,具有可比性。本研究通过医院伦理委员会批准备案,所有患者均知情同意。
Table 1. Comparison of general information between two groups of patients ( )
表1. 两组患者一般资料比较( )
Table 2. Proportion of damaged ligaments in two groups of patients (%)
表2. 两组患者受损韧带的比例(%)
2.3. 手术方法
患者腰硬联合麻醉成功后取侧卧位,常规消毒铺单。取外踝弧形切口,起自距骨头,长约10 cm,逐层切开皮肤,皮下组织及深筋膜,钝性分离并探查踝关节外侧各韧带(ATFL、CFL及PTFL),明确各韧带损伤情况,以及韧带撕裂的部位和数量,用4.5 mm × 14 mm带线锚钉(美国Arthrex聚醚醚酮骨锚钉系统)固定缝合修复撕裂的韧带于其外踝的解剖止点处,加强缝合踝关节下伸肌支持带,修复缝合关节囊及腓骨长、短肌腱鞘,检查韧带缝合牢固,行前抽屉试验及距骨倾斜试验阴性,踝关节正常屈伸无阻挡感。切口逐层缝合,予以加压包敷,踝关节背伸外翻位绷带固定。见图3。

Figure 3. (A) Surgical curved incision; (B) Cut subcutaneous tissue layer by layer to expose the external ankle ligament; (C) Tear of Calcaneal fibular ligament; (D) Tear of the Anterior talofibular ligament; (E) Insert a threaded anchor nail at the insertion point of the fibula of the Calcaneal fibular ligament; (F) Insert a threaded anchor nail at the insertion point of the fibula of the Anterior talofibular ligament; (G) Use a threaded anchor nail tail thread to tighten and suture the ruptured Anterior talofibular ligament and Calcaneus fibular ligament at the fibular insertion point; (H), (I) Suture the joint capsule and strengthen the suture of the extensor support band
图3. (A) 手术弧形切口;(B) 逐层切开皮下组织,暴露外踝韧带;(C) 跟腓韧带撕裂;(D) 距腓前韧带撕裂;(E) 跟腓韧带腓骨止点处打入一枚带线锚钉;(F) 距腓前韧带腓骨止点处打入一枚带线锚钉;(G) 使用带线锚钉尾线分别紧缩缝合断裂的距腓前韧带及跟腓韧带于腓骨止点处;(H)、(I) 缝合关节囊并加强缝合伸肌下支持带
2.4. 术后康复
两组患者踝关节均背伸外翻位绷带固定,术后2 d拆除绷带。术后3周开始足趾屈伸活动踝关节背伸练习及股四头肌等长收缩。术后6周穿踝关节固定靴开始部分负重行走。术后7~8周达完全负重,并逐渐开始小腿三头肌肌力训练。术后2~3个月踝关节各方向活动度练习至正常,并开始正常行走和生活。术后3~4个月小腿三头肌肌力大部分恢复后可酌情开始慢跑等运动,加强小腿三头肌肌力训练,并增加踝关节背伸和内外翻抗阻练习,进行踝关节平衡训练。术后4~6个月恢复正常运动及专项训练。见图4、5。

Figure 4. The ankle range of motion of the 47-year-old male patient returned to normal during the final follow-up. (A) Landing on the sole of the foot; (B) Ankle varus; (C) Ankle valgus; (D) Ankle plantar flexion; (E) Ankle back extension
图4. 患者男47岁末次随访时脚踝活动度均恢复正常。(A) 全脚掌着地;(B) 脚踝内翻;(C) 脚踝外翻;(D) 脚踝跖屈;(E) 脚踝背伸
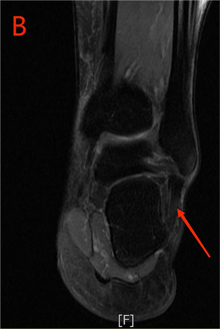
Figure 5. MR at last follow-up. (A) Anterior talofibular ligament; (B) Calcaneus fibular ligament
图5. 末次随访时MR。(A) 距腓前韧带;(B) 跟腓韧带
2.5. 评价指标
记录患者手术时间、术中出血量及重返日常生活时间、重返运动时间等围手术期资料,以及患者对该手术的满意度。记录术前和术后的AOFAS足踝评分、VAS疼痛评分及Karlsson踝关节功能评分。测量术前、术后的距骨倾斜角和距骨前移距离的变化。
2.6. 统计学方法
应用SPSS23.0统计软件进行统计学分析。计量资料以 表示,采取t检验或秩和检验;计数资料采取卡方检验。P < 0.05为差异有统计学意义。
3. 结果
3.1. 随访期间并发症情况及满意度调查
所有患者均获得12个月以上随访,随访期间均未发生感染、神经损伤、再扭伤、踝关节不稳及外侧僵硬等并发症。末次随访时,慢性组满意度为88.9%,急性组满意度为94.9%,差异无统计学意义(P > 0.05)。见表3。
Table 3. Satisfaction survey of two groups of patients at the last follow-up
表3. 两组患者末次随访时满意度调查
3.2. 手术相关指标比较
两组患者手术时间及术中出血量比较,差异无统计学意义(P > 0.05)。见表4。
Table 4. Comparison of surgical related indicators between two groups of patients ( )
表4. 两组患者手术相关指标比较( )
3.3. 踝关节功能及疼痛评分比较
术前,两组患者的AOFAS、VAS及Karlsson评分比较,差异无统计学意义(P > 0.05)。随时间推移,两组VAS评分均呈下降趋势,相应时间节点,与术前比较,差异有统计学意义(P < 0.05),两组相互比较,完全没有差异(P < 0.05),见表5。
Table 5. Comparison of VAS scores between two groups of patients ( )
表5. 两组患者VAS评分比较( )
*P < 0.05,与术前比较。
两组AOFAS及Karlsson评分均呈上升趋势,相应时间节点,与术前比较,差异有统计学意义(P < 0.05),两组相互比较,差异无统计学意义(P > 0.05),见表6、7。
Table 6. Comparison of AOFAS scores between two groups of patients ( )
表6. 两组患者AOFAS评分比较( )
*P < 0.05,与术前比较。
Table 7. Comparison of Karlsson scores between two groups of patients ( )
表7. 两组患者Karlsson评分比较( )
*P < 0.05,与术前比较。
3.4. 距骨倾斜角和距骨前移距离变化
术前,两组患者距骨倾斜角及距骨前移距离比较,差异无统计学意义(P > 0.05)。末次随访时,两组患者的距骨倾斜角及距骨前移距离均减小(见图6),与术前相比差异有统计学意义(P < 0.05),两组相互比较无统计学意义(P > 0.05)。见表8。
Table 8. Comparison of talus inclination angle and talus forward displacement distance between two groups of patients ( )
表8. 两组患者距骨倾斜角和距骨前移距离比较( )
*P < 0.05,与术前比较。

Figure 6. X-rays at the last follow-up. (A) Talus inclination angle; (B) Distance of talus forward movement
图6. 末次随访时X片。(A) 距骨倾斜角;(B) 距骨前移距离
3.5. 随访期间两组患者重返日常生活及运动情况
随访期间,两组患者的重返日常生活比例及重返运动比例比较,差异无统计学差异(P > 0.05)。见 表9。
Table 9. Comparison of the proportion of patients returning to daily life and exercise at different time points after surgery between two groups [number of cases (%)]
表9. 两组患者术后各时间点重返日常生活和重返运动比例比较[例数(%)]
4. 讨论
踝关节外侧副韧带急性损伤多是由运动扭伤导致踝关节平衡功能失调所致,其中踝关节过度内翻引起外侧副韧带不同程度的损伤,包括一条或多条韧带的部分撕裂或完全断裂 [9] ,从而导致局部组织液渗出和出血,由此可引发踝关节肿胀、跛行和疼痛等临床症状。若急性损伤早期未能及时得到正确处理,易出现反复扭伤,引起踝关节外侧副韧带慢性损伤而出现踝关节不稳,继发引起关节软骨的损伤退变,进一步发展为创伤性骨关节炎。踝关节外侧副韧带急性损伤因多为单一韧带部分损伤,故多采用保守治疗 [10] ,主要以石膏固定、制动为主,临床疗效较好,若石膏固定、制动时间较长,易对踝关节功能恢复造成影响。故在明确诊断踝关节韧带完全断裂或多条韧带撕裂,出现踝关节不稳且严重影响生活时,应积极采取手术治疗,可以最大程度的修复韧带,促进踝关节的稳定性增强,恢复患者的踝关节功能。当踝关节外侧副韧带急性损伤未能得到及时有效的治疗,不可避免的发展为慢性踝关节不稳定,导致踝关节韧带持续慢性损伤,有研究表明,其损伤时间越长,软骨损伤越重,还可能残留术后持续性疼痛 [11] ,同时韧带挛缩变短、疤痕粘连,不利于下一步治疗,故明确诊断后应尽早采取手术治疗,修复韧带,避免进一步发展为踝关节骨性关节炎。
比较两组患者的术中出血量及手术时间,未出现明显差异,且两组患者的出血量及手术时间均处于低位,这一结果表明,该手术方式不会因患者的病程长短和韧带的存在状态而出现术中情况的不同,进一步证实该手术方式的安全、可靠。在末次随访时,调查患者对该手术的满意度,慢性组为88.9%,急性组为94.9%,且两组均未出现不满意或疗效差的情况,说明两组患者对该手术的术后疗效均能达到自己的预期。同时急性组满意度稍高于慢性组,可能与慢性组患者病史过长,已经出现关节内病变或相关并发症有关。同时,应力位X片下距骨倾斜角及距骨前移距离的变化也是一个重要的评判指标 [12] [13] ,当行前抽屉试验时,距骨前移距离 > 9 mm或与健侧相比向前移动距离 > 5 mm;当行内翻应力试验时,距骨倾斜角 > 10˚或与健侧相比 > 3˚,则可诊断为踝外侧韧带损伤伴踝关节不稳定,这已被大多数学者所接受,但这一标准目前仍具有较大争议。也有学者认为慢性损伤患者由于疤痕粘连等因素,不易引出而出现阴性结果。在本研究中,两组患者术前麻醉状态下前抽屉试验及内翻应力试验均为(+),测量距骨倾斜角及距骨前移距离均达到诊断标准,末次随访时,两者的测量值与术前相比均明显减小。说明该术式对于急性与慢性患者,不仅从其主观感受无明显的临床疗效差异,而且从影像学等客观指标来看,两组患者同样没有任何差异。
根据相关研究报道,踝关节外侧副韧带损伤的急性期与慢性期的具体定义存在一定争议,既有通过病史长短又有通过影像学资料等多种方式来定义急性期与慢性期。因此本研究采用时间跨度进行分组,将病史 < 3个月的患者归为急性期组,而将病史 ≥ 3个月的患者归为慢性期 [14] [15] [16] 。同时,根据本研究结果发现,踝关节外侧三条韧带的损伤比例及各自功能均有所差异。在慢性组中,单独ATFL损伤为33.3%,ATFL合并CFL损伤为58.3%,ATFL、CFL及PTFL同时损伤为8.3%;在急性组中,单独ATFL损伤为46.2%,ATFL合并CFL损伤为51.3%,ATFL、CFL及PTFL同时损伤为2.6%。无论在慢性组还是在急性组,ATFL均有损伤、断裂,说明ATFL对维持踝关节功能及稳定性最重要 [3] [17] [18] 。合并有CFL撕裂或松弛(功能丧失)在慢性组与急性组占比相当且较高,术中探查修复CFL对踝关节的稳定性也至关重要。而合并PTFL的患者较少,术中探查均为部分损伤、松弛,未见撕裂,功能未丧失,故急慢性组均未行带线锚钉修复固定,若伴有踝关节骨折、脱位合并严重的外侧副韧带断裂的患者则需手术解剖修复PTFL。
本研究采用改良Karlsson术修复距腓前韧带或跟腓韧带,加强缝合伸肌下支持带,未破坏踝关节的生物力学及局部解剖结构。术后两组患者的AOFAS及Karlsson评分均高于术前,且呈逐步上升的趋势,同时踝关节功能恢复快且并发症少,表明该手术方式对于急性踝关节外侧副韧带的损伤、撕裂和慢性踝关节外侧副韧带的持续损伤、关节不稳都有不错的临床效果。进一步比较两组患者术后的AOFAS、VAS及Karlsson评分,不难发现两组患者的恢复情况没有明显差距,均能满足患者日常生活及运动的需要。该研究的手术方式旨在帮助患者恢复日常生活和运动,不影响生活水平,故比较了各时间节点两组患者的重返日常生活和重返运动的比例,可以发现在术后3个月时,两组患者重返日常生活的人数均为50%左右,而重返运动的患者极少,同样在6个月时,几乎所有患者均能正常生活,而两组重新返回日常运动的人数均在50%以下,手术后1年时,两组患者均能正常生活及回到受伤前的运动水平。这一结果表明,不管对于急性损伤的新鲜韧带还是慢性持续损伤而挛缩变短的陈旧性韧带,改良Karlsson术式均能够帮助患者重新回到受伤前的生活状态和运动水平,且两组患者的恢复时间没有显著性差异,进一步表明,该术式不会因患者的病程长短和韧带的存在状态而出现术后疗效的不同,同时在没有发生踝关节创伤性关节炎之前,对急慢性踝关节外侧副韧带的损伤、关节不稳均有满意的临床疗效。
根据本研究结果及相关资料,急性损伤的新鲜韧带和慢性持续性损伤的陈旧性韧带,通过手术解剖修复治疗,两者的术后疗效没有本质区别。故笔者认为对于运动要求较高的青壮年患者或运动员,当明确诊断为急性踝关节外侧副韧带损伤、关节不稳时,在康复锻炼、短期制动等保守治疗失败或疗效不理想的情况下,尤其MR显示ATFL完全断裂或伴有CFL部分或完全撕裂,麻醉下踝关节前抽屉试验或内翻应力试验(+),主张积极手术修复受损韧带,目的是加强踝关节稳定性,尽早恢复运动 [19] 。同时急性期治疗可避免进一步发展为慢性踝关节不稳定而出现更多的并发症,也有利于韧带撕裂后的早期修复,韧带缝合牢固、精准、确切。而对于稳定性较低的中老年患者,应首选保守治疗和康复锻炼,在不影响日常生活的情况下,暂不考虑手术治疗 [20] [21] 。同时,当患者已经明确诊断为慢性踝关节不稳定时,考虑患者病史较长,可能会出现踝关节滑膜炎、软骨损伤、骨赘形成和骨关节炎等关节内病变,影响手术效果,故应尽早手术干预,避免对患者日常生活造成严重影响。
本研究病例较少,随访时间较短,远期疗效未进一步跟踪研究,同时未将青壮年与中老年分开纳入研究,可能会出现选择偏倚,影响研究结果。故以后将增加样本量,延长随访时间,进一步细致分组,进行前瞻性随机研究,将该研究更加深入继续进行下去。同时踝关节软骨对踝关节的运动和稳定性起着重要作用,未来需进一步研究软骨损伤对术后疗效的影响。
5. 结论
改良Karlsson术治疗踝关节外侧副韧带急性损伤与慢性持续性损伤,手术操作简便,安全可靠,均能取得满意的临床疗效,且两者术后疗效对比,无明显差异。
文章引用
匡 鑫,孟 晔. 改良Karlsson术治疗踝外侧副韧带急性与慢性损伤的疗效对比
Comparison of the Therapeutic Effects of Modified Karlsson Procedure on Acute and Chronic Injuries of the Lateral Collateral Ligament of the Ankle[J]. 临床医学进展, 2023, 13(12): 20442-20455. https://doi.org/10.12677/ACM.2023.13122878
参考文献
- 1. Porter, D.A. and Kamman, K.A. (2018) Chronic Lateral Ankle Instability: Open Surgical Management. Foot and Ankle Clinics, 23, 539-554. https://doi.org/10.1016/j.fcl.2018.07.002
- 2. Dias, S., Lewis, T.L., Alkhalfan, Y., et al. (2022) Current Concepts in the Surgical Management of Chronic Ankle Lateral Ligament Instability. Journal of Ortho-paedics, 33, 87-94. https://doi.org/10.1016/j.jor.2022.07.006
- 3. Cordier, G., Nunes, G.A., Vega, J., et al. (2021) Connecting Fibers between ATFL’s Inferior Fascicle and CFL Transmit Tension between both Ligaments. Knee Surgery, Sports Traumatology, Arthroscopy: Official Journal of the ESSKA, 29, 2511-2516. https://doi.org/10.1007/s00167-021-06496-w
- 4. Herzog, M.M., Kerr, Z.Y., Marshall, S.W., et al. (2019) Epide-miology of Ankle Sprains and Chronic Ankle Instability. Journal of Athletic Training, 54, 603-610. https://doi.org/10.4085/1062-6050-447-17
- 5. Vuurberg, G., Altink, N., Rajai, M., et al. (2019) Weight, BMI and Stability Are Risk Factors Associated with Lateral Ankle Sprains and Chronic Ankle Instability: A Meta-Analysis. Journal of ISAKOS: Joint Disorders & Orthopaedic Sports Medicine, 4, 313-327. https://doi.org/10.1136/jisakos-2019-000305
- 6. Cottom, J.M., Graney, C.T. and Sisovsky, C. (2020) Evaluation of BMI with an All inside Arthroscopic Broström Procedure for Chronic Lateral Ankle Instability: An Analysis of 113 Patients. The Journal of Foot and Ankle Surgery, 59, 1008-1012. https://doi.org/10.1053/j.jfas.2019.10.016
- 7. 焦晨, 胡跃林, 郭秦炜, 等. 距跟外侧韧带替代法治疗跟腓韧带缺失的慢性踝关节外侧不稳[J]. 中国运动医学杂志, 2016, 35(3): 211-214.
- 8. 孙健, 蔡郑东, 朱裕昌, 等. 改良Karlsson术治疗踝关节外侧副韧带损伤伴慢性踝关节不稳症疗效分析[J]. 中国运动医学杂志, 2014, 33(6): 510-513+551.
- 9. Slater, K. (2018) Acute Lateral Ankle Instability. Foot and Ankle Clinics, 23, 523-537. https://doi.org/10.1016/j.fcl.2018.07.001
- 10. Rezaninova, J., Hrazdira, L., Moc Kralova, D., et al. (2018) Ad-vanced Conservative Treatment of Complete Acute Rupture of the Lateral Ankle Ligaments: Verifying by Stabilometry. Foot and Ankle Surgery, 24, 65-70. https://doi.org/10.1016/j.fas.2016.12.001
- 11. Golditz, T., Steib, S., Pfeifer, K., et al. (2014) Functional Ankle In-stability as a Risk Factor for Osteoarthritis: Using T2-Mapping to Analyze Early Cartilage Degeneration in the Ankle Joint of Young Athletes. Osteoarthritis and Cartilage, 22, 1377-1385. https://doi.org/10.1016/j.joca.2014.04.029
- 12. Purevsuren, T., Batbaatar, M., Khuyagbaatar, B., et al. (2018) Comparative Evaluation between Anatomic and Nonanatomic Lateral Ligament Reconstruction Techniques in the Ankle Joint: A Computational Study. Journal of Biomechanical Engineering, 140, Article ID: 061009. https://doi.org/10.1115/1.4039576
- 13. Gomes, J.L.E., Soares, A.F., Bastiani, C.E., et al. (2018) Anterolateral Talar Palpation: A Complementary Test for Ankle Instability. Foot and Ankle Surgery, 24, 486-489. https://doi.org/10.1016/j.fas.2017.05.006
- 14. 谢兴, 胡跃林, 焦晨, 等. 55例踝关节外侧副韧带损伤合并外踝撕脱骨折的手术治疗分析[J]. 中华骨与关节外科杂志, 2015, 8(1): 66-70.
- 15. 陈明亮, 周耀君, 谷成毅, 等. 开放与关节镜下改良Brostr(o)m术式治疗慢性踝关节外侧副韧带损伤的对比研究[J]. 中国运动医学杂志, 2020, 39(2): 104-110.
- 16. Noda, Y., Horibe, S., Hiramatsu, K., et al. (2021) Quick and Simple Test to Evaluate Severity of Acute Lateral Ankle Sprain. Asia-Pacific Journal of Sports Medicine, Arthroscopy, Rehabilitation and Technology, 25, 30-34. https://doi.org/10.1016/j.asmart.2021.05.003
- 17. Brown, C.N., Rosen, A.B. and Ko, J. (2015) Ankle Ligament Laxity and Stiffness in Chronic Ankle Instability. Foot & Ankle International, 36, 565-572. https://doi.org/10.1177/1071100714561057
- 18. Kim, J.S., Kim, M.S., Kim, D.K., et al. (2023) Magnetic Reso-nance Imaging Characteristics of a Lateral Ligament Injury in Acute Ankle Sprains among Athletes. Orthopaedic Journal of Sports Medicine, 11. https://doi.org/10.1177/23259671231207688
- 19. 冉讯, 陈志伟, 崔俊成, 等. 带线锚钉修复治疗合并腓骨尖撕脱骨折的距腓前韧带损伤后踝关节不稳的临床疗效观察[J]. 足踝外科电子杂志, 2021, 8(2): 10-14+9+6.
- 20. Lin, C.I., Houtenbos, S., Lu, Y.H., et al. (2021) The Epidemiology of Chronic Ankle Instability with Perceived Ankle Instability—A Systematic Review. Journal of Foot and Ankle Research, 14, Article No. 41. https://doi.org/10.1186/s13047-021-00480-w
- 21. Delahunt, E. and Remus, A. (2019) Risk Factors for Lateral Ankle Sprains and Chronic Ankle Instability. Journal of Athletic Training, 54, 611-616. https://doi.org/10.4085/1062-6050-44-18
NOTES
*第一作者。
#通讯作者。
