Advances in Clinical Medicine
Vol.
13
No.
06
(
2023
), Article ID:
66733
,
9
pages
10.12677/ACM.2023.1361266
急性脑梗死患者介入术后预后相关因素的单中心回顾性研究
王旭,代林志,董江涛,赵冬*
石河子大学医学院第一附属医院神经外科,新疆 石河子
收稿日期:2023年5月7日;录用日期:2023年5月31日;发布日期:2023年6月8日

摘要
目的:探讨影响AIS患者机械取栓及补救性支架置入预后的相关因素。方法:选取本中心2019年至2022年所有进行机械取栓及补救性支架治疗的AIS患者,根据术后90天mRS评分将患者分为预后良好组(mRS评分0~2分)及预后不良组(mRS评分3~6分)。收集患者人口学特征、既往病史、入院时SII、术后24小时SII差值、肝肾功、OPT、入院时NIHSS评分、术后90天的mRS评分等临床资料;比较两组的资料有无统计学差异;使用多因素二元logistics回归分析影响AIS患者预后的独立危险因素;运用ROC曲线评估各独立危险因素对AIS患者预后的评估价值。结果:1) 入院NIHSS评分、OPT、取栓次数、LDH、SII差值是AIS患者介入术后预后的危险因素(OR > 1, P < 0.05);2) ROC曲线分析表明各独立危险因素联合预测预后不良的准确性比单用NIHSS效果更佳(P < 0.05)。结论:1) 入院NIHSS评分、发病至股动脉穿刺时间、取栓次数、乳酸脱氢酶、术后24小时SII差值是影响AIS患者介入术后预后的独立危险因素;2) 各独立危险因素联合预测预后具有更优的预测效能。
关键词
急性缺血性脑梗死,全身炎症指数,预后

A Single-Center Retrospective Study of Factors Associated with the Prognosis of Patients with Acute Ischemic Stroke after Interventional Therapy
Xu Wang, Linzhi Dai, Jiangtao Dong, Dong Zhao*
School of Neurosurgery, The First Affiliated Hospital of Shihezi University School of Medicine, Shihezi Xinjiang
Received: May 7th, 2023; accepted: May 31st, 2023; published: Jun. 8th, 2023

ABSTRACT
Objective: This study examines the factors associated with the prognosis of patients with AIS after interventional therapy. Methods: All AIS patients who underwent mechanical thrombectomy and remedial stenting in our center from 2019 to 2022 were selected, and patients were divided into good prognosis group (mRS score 0~2) and poor prognosis group (mRS score 3~6) according to their 90-day postoperative mRS score; patient data include demographic characteristics, past medical history, SII at admission, 24-hour postoperative SII. The clinical data including demographic characteristics, past medical history, SII at admission, SII at 24 hours postoperatively, difference, liver and kidney function, OPT, NIHSS score at admission, and mRS score at 90 days postoperatively were collected; whether there was a statistical difference between the data collected in the two groups was compared; the independent risk factors affecting the prognosis of AIS patients were analyzed by using multifactorial binary logistic regression; the value of each independent risk factor in assessing the prognosis of AIS patients was assessed by using ROC curves. Results: 1) Admission NIHSS score, OPT, number of mechanical bolus retrievals, LDH, and SII difference were risk factors affecting the prognosis of patients with AIS undergoing interventional therapy (OR > 1, P < 0.05); 2) ROC curve analysis showed that the combination of independent risk factors was better than NIHSS score alone in predicting the accuracy of poor prognosis in patients with AIS (P < 0.05). Conclusion: 1) Admission NIHSS score, time from onset to femoral artery puncture, number of mechanical bolus retrievals, lactate dehydrogenase, and 24-hour postoperative SII difference were independent risk factors affecting the prognosis of patients with AIS after intervention; 2) the combination of independent risk factors had superior predictive efficacy in predicting prognosis.
Keywords:Acute Ischemic Stroke, Systemic Immune Inflammation Index, Prognosis

Copyright © 2023 by author(s) and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/


1. 引言
急性缺血性脑卒中(acute ischemic stroke, AIS),又称急性脑梗死,是最常见的卒中类型。脑卒中现已成为我国居民致死、致残的第一大原因,占我国脑卒中的69.6%~70.8% [1] 。其中颅内大动脉急性闭塞在全部新发卒中患者中的占比约为80% [2] ,大血管闭塞导致的卒中病情重、预后差,给个人、家庭、社会带来严重的医疗负担。尽早开通闭塞血管,恢复血流灌注是有效治疗AIS的关键 [3] 。因此及时有效开通病变血管并准确评估AIS患者预后具有重要临床意义。目前很多研究表明免疫炎症反应机制在AIS发病过程中起着重要作用 [4] [5] [6] ,全身免疫炎症指数(systemic immune-inflammation index, SII)作为一中结合中性粒细胞、淋巴细胞及血小板的新型炎症标记物,已有研究证明SII是卒中相关性肺炎的独立危险因素 [7] ,但SII与AIS患者行机械取栓及补救性支架置入的预后相关性研究尚少。本研究旨在探讨影响介入术后AIS患者预后的相关因素、SII对于介入术后的AIS患者的预测价值,并通过联合指标预测以期在疾病发生早期判断卒中严重程度及预后不良的患者,为此患者的治疗提供一定的依据,以改善患者预后。
2. 研究对象与方法
2.1. 研究对象
本研究采用回顾性研究方法,纳入2019年6月至2022年5月入住石河子大学医学院第一附属医院神经外科且符合AIS诊断标准 [3] 的患者。所有受试者均签署知情同意书,本方案经我院伦理委员会批准(批号:KJX2021-117-01)。
2.2. 纳入及排除标准
纳入标准:1) 术前经头颅CT检查排除颅内出血,临床症状符合缺血性脑卒中;2) 年龄 ≥ 18岁;3) 本次发病前mRS评分0~2分;4) 脑卒中诊断标准符合《中国急性缺血性脑卒中诊治指南2018》;5) 临床资料完整;6) 患者(委托人)知情同意。
排除标准:1) 卒中由动脉夹层或血管炎引起;2) 合并其他严重疾病,包括肿瘤、免疫系统、肝肾功能不全、自身免疫系统疾病、血液系统疾病等病史;3) 卒中发病两周内服用免疫抑制类药物史;4) 发病前存在禁忌症或实验室检查提示不能使用造影剂、阿司匹林或者氯吡格雷;5) 严重的其他疾病,包括其他重要脏器功能衰竭、恶性肿瘤预计寿命小于3年;6) 临床资料不完整及回访丢失患者。
2.3. 资料收集
收集患者人口学特征及临床资料,人口学资料包括:性别、年龄、BMI (身体质量指数)、个人史(吸烟史、饮酒史);临床资料包括:既往史(高血压、糖尿病)、入院时NIHSS (National Institute of health stroke scale)评分、发病至股动脉穿刺时间(Onset to puncture time, OPT)、入院及术后24小时内静脉抽血检查、术后90天mRS评分。
根据血常规结果计算全身炎症指数(SII) (109/L),SII = P × N/L,其中P、N、L分别代表外周血小板、中性粒细胞、淋巴细胞计数;根据体重(kg)、身高(m),计算BMI = 体重/身高2。
术后出血转化:根据术后头颅CT或MRI影像明确颅内是否发生出血转化,根据海德堡出血分型 [8] 定义症状性颅内出血(symptomatic Intracranial Hemorrhage, sICH)。
2.4. 分组
使用改良Rankin量表(mRS)评估患者术后90天的神经功能预后,预后良好定义为mRS评分 ≤ 2分、预后不良为mRS评分 ≥ 3分 [9] 。
2.5. 统计学方法
数据采用SPSS 26.0进行处理,符合正态分布的计量资料用 表示,组间比较使用t检验;偏态分布的计量资料用中位数(四分位间距)表示,组间比较使用非参数秩和检验;计数资料用频数(%)表示,组间比较采用χ2检验;等级资料使用非参数秩和检验;相关性分析使用Spearman相关分析;对于危险因素的评估使用多因素二元Logistic进行分析;用ROC曲线评估各独立危险因素对AIS患者预后影响的预测价值。用MedCalc 20.0软件使用Delong检验各独立危险因素联合和单用NIHSS评分预测AIS患者预后的准确性差异。当P < 0.05时,表明差异具有统计学意义。
3. 结果
本次研究收集440例,排除22人(资料不全10人,失访7人,不愿配合5人)共纳入418例,其中预后良好组246例,预后不良组172例,单纯取栓组278例,补救性支架置入组140例,男性290 (69.38%)人,女性128 (30.62%)人。
3.1. 单因素分析
经单因素分析可知,年龄、入院NIHSS、取栓次数、乳酸脱氢酶、同型半胱氨酸、术后24小时SII差值、出血转化、发病至股动脉穿刺时间、白蛋白、纤维蛋白原组间均存在统计学差异(P < 0.05),见表1。
Table 1. Clinical data analysis of good group and poor group
表1. 良好组与不良组临床资料分析
注:LDH为乳酸脱氢酶,单位:mmol/L;HCY为同型半胱氨酸,单位:mmol/L;BMI为身体质量指数;SII为全身免疫炎症指数,单位:109/L;OPT为发病至股动脉穿刺时间,单位:小时;*表示差异有统计学意义;n为例数;P < 0.05。
3.2. 多因素Logistic回归
使用多因素二元logistics回归分析建立模型,认为入院NIHSS、乳酸脱氢酶、取栓次数、发病至股动脉成功穿刺时间、术后24小时SII差值是影像AIS患者预后不良的独立危险因素(P < 0.05, OR值 > 1),见表2。
Table 2. Independent risk factors affecting prognosis
表2. 影响预后的独立危险因素
注:LDH为乳酸脱氢酶,单位:mmol/L;HCY为同型半胱氨酸,单位:mmol/L;SII为全身免疫炎症指数,单位:109/L;OPT为发病至股动脉穿刺时间,单位:小时;*表示差异有统计学意义;n为例数;P < 0.05。
3.3. ROC曲线分析
根据独立危险因素构建ROC曲线发现SII差值预测预后不良的AUC值为0.845 (P < 0.000),阈值为1076.34,预测敏感度为0.802,特异度为0.817;发病至股动脉穿刺时间预测预后不良的AUC值为0.851 (P < 0.000),阈值为10.00,预测敏感度为0.767,特异度为0.866;乳酸脱氢酶预测预后不良的AUC值为0.767 (P < 0.000),阈值为298.15,预测敏感度为0.773,特异度为0.715;入院NIHSS预测预后不良的AUC值为0.828 (P < 0.000),阈值为15.5,预测敏感度为0.826,特异度为0.748;取栓次数预测预后不良的AUC值为0.842 (P < 0.000),阈值为2.5,预测敏感度为0.791,特异度为0.809,见图1、表3。
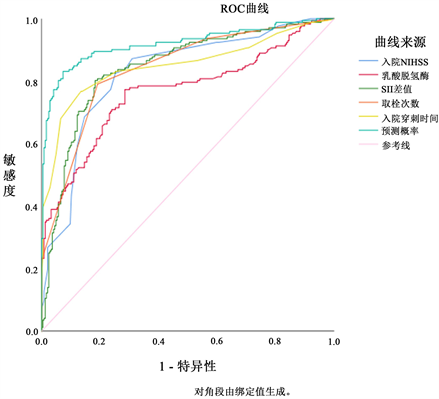
Figure 1. Predictive value of independent risk factors for poor prognosis in AIS patients
图1. 各独立危险因素对AIS患者预后不良的预测价值分析
Table 3. ROC curve analysis of prognostic factors in stent group
表3. 支架组预后影响因素的ROC曲线分析
注:LDH为乳酸脱氢酶,单位:mmol/L;SII为全身免疫炎症指数,单位:109/L;OPT为发病至股动脉穿刺时间,单位:小时;*表示差异有统计学意义;n为例数;P < 0.05。
3.4. 联合指标对预后的预测价值分析
将各独立危险因素联合,运用MedCalc 20.0软件,通过Delong检验分析,结果显示联合指标较单用NIHSS预测AIS患者90天神经功能预后效果更好(P < 0.05),见表4。
Table 4. Predictive value analysis of combined indicators in thrombectomy group
表4. 取栓组联合指标的预测价值分析
注:*表示差异有统计学意义;P < 0.05。
4. 讨论
本研究回顾性分析2019年6至2022年5月入住石河子大学第一附属医院神经外科的急性脑梗死患者,通过统计学分析发现入院NIHSS、乳酸脱氢酶、取栓次数、发病至股动脉成功穿刺时间、术后24小时SII差值为影响AIS患者预后的独立危险因素。同时各独立危险因素联合与传统单用NIHSS评分预测AIS患者预后相比具有更优的预测效能。
本研究发现SII与AIS患者预后独立相关,它代表了体内部分炎症与免疫反应。此值最早被用于评估肺癌、胃癌、结直肠癌、乳腺癌等患者预后 [10] [11] [12] [13] ,研究表明免疫炎症反应参与了AIS的整个病理过程 [14] 。已有研究表明中性粒细胞、淋巴细胞水平与AIS患者病情严重程度有关 [15] [16] 。我们推测,AIS发生急性期,因脑组织缺血损伤,大量促炎性因子被释放,导致继发性神经炎症的产生,促炎因子迅速激活并介导大量炎症细胞(中性粒细胞、单核/巨噬细胞、不同亚型的T细胞和其他炎症细胞)向局部缺血区域浸润,同时释放毒性物质及炎症因子,加重神经功能损害。另一个原因可能是小胶质细胞及星型胶质细胞在AIS发生后的数小时内被激活产生大量细胞因子及趋化因子 [17] ,诱导炎症反应的发生。炎症反应及细胞因子可导致血脑屏障破坏,加重脑细胞水肿 [18] [19] 。同时,激活的神经胶质细胞与免疫细胞共同作用,介导其他病理反应及毒性物质的产生,包括氧化应激、兴奋毒性、基质金属蛋白酶(matrix metalloproteinases, MMPs)、花生四烯酸代谢物、丝裂原激活的蛋白激酶(mitogen-activated protein kinase, MAPK)等,进一步破坏血脑屏障 [20] ,加重脑组织损伤及神经元细胞凋亡 [21] 。
乳酸脱氢酶是一种存在于不同组织中的细胞质酶,它可作为炎症或其他病理条件引起的细胞破坏的指示物 [22] 。Anxin Wang等人发现高水平乳酸脱氢酶与AIS患者与短暂性脑缺血发作患者不良预后有关 [23] ;Dan Yan等人研究表明乳酸脱氢酶水平与ASI患者卒中相关肺炎的发病风险相关 [24] ;这也与本研究的分析结果一致,我们推测当脑细胞及神经元细胞因缺血出现损伤时,受损的细胞释放乳酸脱氢酶经细胞间隙扩散入脑脊液,再通过受损的血脑屏障进入血液循环,进而提升外周血中乳酸脱氢酶含量。同时,过量的乳酸脱氢酶可加快乳酸堆积,引起缺血脑组织酸中毒,加剧细胞水肿及再灌注损伤,造成血脑屏障破坏 [25] 。同时乳酸脱氢酶可通过增加干扰素-γ的乙酰化和转录来促进炎症反应的发生,加重细胞损伤 [26] 。
本研究发现入院NIHSS评分、发病至股动脉穿刺时间、取栓次数为影响AIS患者预后的独立危险因素。NIHSS评分作为评估AIS发病严重程度的重要指标 [27] ,因快速、易操作性、可信度高,目前已经得到了广泛临床应用 [28] 。AIS患者治疗关键是缩短发病至血流再灌注的时间,2015年5大RCT实验 [29] [30] [31] [32] [33] 均强调缩短发病至再灌注时间对改善AIS患者预后的重要性;Menon B K等人 [34] 的研究表明发病至再灌注时间与机械取栓后患者的良好预后有明显相关性;本中心既往研究 [35] 表明AIS患者就诊时间与预后存在显著相关性。研究表明随着取栓次数的增多,患者病变血管的再通率也在逐渐下降,伴随患者获得良好预后比例也呈下降趋势 [36] 。我们推测这可能与反复取栓操作造成血管内膜损伤增加有关,在实际操作中,为了达到血管快速再通的目的,手术操作医师通常会尝试多次取栓,并在机械取栓再通失败时尝试补救性支架置入治疗。王勇等 [37] 的研究结果显示,术中取栓次数 > 3次是术后发生出血转化的危险因素。NASA登记研究 [38] 的结果认为,即使闭塞血管成功再通,取栓次数 ≥ 3次仍然是AIS患者术后90天功能预后不良独立危险因素。
本次研究的不足在于:单中心回顾性研究;本研究虽采取手术前后患者SII差异进行比较,缺乏动态数据监测;未评估AIS患者超过3个月的神经功能评估;本研究中出血转化对预后影响无统计学差异,考虑可能由于出血转化患者纳入例数过少导致。
文章引用
王 旭,代林志,董江涛,赵 冬. 急性脑梗死患者介入术后预后相关因素的单中心回顾性研究
A Single-Center Retrospective Study of Factors Associated with the Prognosis of Patients with Acute Ischemic Stroke after In-terventional Therapy[J]. 临床医学进展, 2023, 13(06): 9044-9052. https://doi.org/10.12677/ACM.2023.1361266
参考文献
- 1. 佚名. 中国心血管健康与疾病报告(2019)节选二: 脑血管病[J]. 心脑血管病防治, 2020, 20(6): 544-552.
- 2. 中华医学会神经病学分会, 中华医学会神经病学分会脑血管病学组, 中华医学会神经病学分会神经血管介入协作组. 中国急性缺血性卒中早期血管内介入诊疗指南2022 [J]. 中华神经科杂志, 2022, 55(6): 565-580.
- 3. 中华医学会神经病学分会, 中华医学会神经病学分会脑血管病学组. 中国急性缺血性脑卒中诊治指南2018 [J]. 中华神经科杂志, 2018, 51(9): 666-682.
- 4. Agard, T.A., Hass, R., Cavrak, M.E., et al. (2023) Neutrophil Lymphocyte Ratio (NLR) and Systemic Immune Inflammatory Index (SII) for the Differential Diagnosis of CT-Negative Mild Acute Is-chemic Stroke and Transient Ischemic Attack. International Journal of Neuroscience. https://doi.org/10.1080/00207454.2023.2171877
- 5. Huang, L.M. (2023) Increased Systemic Im-mune-Inflammation Index Predicts Disease Severity and Functional Outcome in Acute Ischemic Stroke Patients. The Neurologist, 28, 32-38. https://doi.org/10.1097/NRL.0000000000000464
- 6. Lin, K.-B., Fan, F.-H., Cai, M.-Q., et al. (2022) Systemic Immune Inflammation Index and System Inflammation Response Index Are Potential Biomarkers of Atrial Fibrillation among the Patients Presenting with Ischemic Stroke. European Journal of Medical Research, 27, Article No. 106. https://doi.org/10.1186/s40001-022-00733-9
- 7. 渠成, 张尊胜. 全身免疫炎症指数对急性缺血性脑卒中患者发生卒中相关性肺炎的预测价值[J]. 徐州医学院学报, 2021, 41(7): 528-533.
- 8. von Kummer, R., Broderick, J.P., Campbell, B.C., et al. (2015) The Heidelberg Bleeding Classification: Classification of Bleeding Events after Ischemic Stroke and Reperfusion Therapy. Stroke, 46, 2981-2986. https://doi.org/10.1161/STROKEAHA.115.010049
- 9. 武霄, 宋海庆, 孙蔚, 等. 入院血压对行血管内治疗的急性缺血性卒中患者神经功能预后的影响研究[J]. 中国脑血管病杂志, 2022, 19(11): 733-740.
- 10. Huang, L., Liu, S., Lei, Y., et al. (2016) Systemic Immune-Inflammation Index, Thymidine Phosphorylase and Survival of Localized Gastric Cancer Patients after Curative Resection. Oncotarget, 7, 44185-44193. https://doi.org/10.18632/oncotarget.9923
- 11. Tomita, M., Ayabe, T., Maeda, R. and Nakamura, K. (2018) Sys-temic Immune-Inflammation Index Predicts Survival of Patients after Curative Resection for Non-Small Cell Lung Cancer. In Vivo, 32, 663-667. https://doi.org/10.21873/invivo.11291
- 12. Chen, Q., Wu, H., Guo, X., et al. (2020) The Change of Systemic Im-mune-Inflammation Index Independently Predicts Survival of Colorectal Cancer Patients after Curative Resection. Medi-ators of Inflammation, 2020, Article ID: 4105809. https://doi.org/10.1155/2020/4105809
- 13. Li, W., Ma, G., Deng, Y., et al. (2021) Systemic Immune-Inflammation Index Is a Prognostic Factor for Breast Cancer Patients after Curative Resection. Frontiers in Oncology, 11, Article 570208. https://doi.org/10.3389/fonc.2021.570208
- 14. Pluta, R., Januszewski, S. and Czuczwar, S.J. (2021) Neuroinflammation in Post-Ischemic Neurodegeneration of the Brain: Friend, Foe, or Both? International Journal of Molecular Sciences, 22, Article No. 4405. https://doi.org/10.3390/ijms22094405
- 15. Li, S.-J., Cao, S.-S., Huang, P.-S., et al. 2022) Post-Operative Neutro-phil-to-Lymphocyte Ratio and Outcome after Thrombectomy in Acute Ischemic Stroke. Frontiers in Neurology, 13, Arti-cle 990209. https://doi.org/10.3389/fneur.2022.990209
- 16. Li, W., Hou, M., Ding, Z., et al. (2021) Prognostic Value of Neu-trophil-to-Lymphocyte Ratio in Stroke: A Systematic Review and Meta-Analysis. Frontiers in Neurology, 12, Article 686983. https://doi.org/10.3389/fneur.2021.686983
- 17. Jin, R., Yang, G. and Li, G. (2010) Inflammatory Mecha-nisms in Ischemic Stroke: Role of Inflammatory Cells. Journal of Leukocyte Biology, 87, 779-789. https://doi.org/10.1189/jlb.1109766
- 18. Ceulemans, A.-G., Zgavc, T., Kooijman, R., et al. (2010) The Dual Role of the Neuroinflammatory Response after Ischemic Stroke: Modulatory Effects of Hypothermia. Journal of Neuroin-flammation, 7, Article No. 74. https://doi.org/10.1186/1742-2094-7-74
- 19. Kim, J.Y., Park, J., Chang, J.Y., Kim, S.-H. and Lee, J.E. (2016) In-flammation after Ischemic Stroke: The Role of Leukocytes and Glial Cells. Experimental Neurobiology, 25, 241-251. https://doi.org/10.5607/en.2016.25.5.241
- 20. Dyatlova, A.S., Novikova, N.S., Yushkov, B.G., et al. (2022) The Blood-Brain Barrier in Neuroimmune Interactions and Pathological Processes. Herald of the Russian Academy of Sci-ences, 92, 590-599. https://doi.org/10.1134/S1019331622050100
- 21. 卢敏, 郑威楠. 水通道蛋白AQP-4与脑水肿[J]. 农垦医学, 2012, 34(3): 254-258.
- 22. Drent, M., Cobben, N., Henderson, R.F., Wouters, E.F. and van Dieijen-Visser, M. (1996) Usefulness of Lactate Dehydrogenase and Its Isoenzymes as Indicators of Lung Damage or Inflammation. European Respiratory Journal, 9, 1736-1742. https://doi.org/10.1183/09031936.96.09081736
- 23. Wang, A., Tian, X., Zuo, Y., et al. (2021) High Lactate De-hydrogenase Was Associated with Adverse Outcomes in Patients with Acute Ischemic Stroke or Transient Ischemic At-tack. Annals of Palliative Medicine, 10, 10185-10195. https://doi.org/10.21037/apm-21-2195
- 24. Yan, D., Huang, Q., Dai, C., Ren, W. and Chen, S. (2021) Lactic De-hydrogenase to Albumin Ratio Is Associated with the Risk of Stroke-Associated Pneumonia in Patients with Acute Is-chemic Stroke. Frontiers in Nutrition, 8, Article 743216. https://doi.org/10.3389/fnut.2021.743216
- 25. Bakay, R.A.E. and Ward Jr., A.A. (1983) Enzymatic Changes in Serum and Cerebrospinal Fluid in Neurological Injury. Journal of Neurosurgery, 58, 27-37. https://doi.org/10.3171/jns.1983.58.1.0027
- 26. Certo, M., Tsai, C.-H., Pucino, V., Ho, P.-C. and Mauro, C. (2021) Lactate Modulation of Immune Responses in Inflammatory Versus Tumour Microenvi-ronments. Nature Reviews Immunology, 21, 151-161. https://doi.org/10.1038/s41577-020-0406-2
- 27. Ding, G.-Y., Xu, J.-H., He, J.-H. and Nie, Z.-Y. (2022) Clinical Scoring Model Based on Age, NIHSS, and Stroke-History Predicts Outcome 3 Months after Acute Ischemic Stroke. Frontiers in Neurology, 13, Article 935150. https://doi.org/10.3389/fneur.2022.935150
- 28. Goyal, M., Menon, B.K., Zwam, W., et al. (2016) Endovascular Thrombectomy after Large-Vessel Ischaemic Stroke: A Meta-Analysis of Individual Patient Data from Five Randomised Trials. Lancet, 387, 1723-1731. https://doi.org/10.1016/S0140-6736(16)00163-X
- 29. Berkhemer, O.A., Fransen, P.S., Beumerd, D., et al. (2015) A Randomized Trial of Intraarterial Treatment for Acute Ischemic Stroke. New England Journal of Medicine, 372, 11-20. https://doi.org/10.1056/NEJMoa1411587
- 30. Campbell, B.C.V., Mitchell, P.J., Kleinig, T.J., et al. (2015) Endo-vascular Therapy for Ischemic Stroke with Perfusion-Imaging Selection. New England Journal of Medicine, 372, 1009-1018. https://doi.org/10.1056/NEJMoa1414792
- 31. Goyal, M., Demchuk, A.M., Menon, B.K., et al. (2015) Randomized Assessment of Rapid Endovascular Treatment of Ischemic Stroke. New England Journal of Medicine, 372, 1019-1030. https://doi.org/10.1056/NEJMoa1414905
- 32. Saver, J.L., Goyal, M., Bonafe, A., et al. (2015) Stent-Retriever Thrombectomy after Intravenous t-PA vs. t-PA Alone in Stroke. New England Journal of Medicine, 372, 2285-2295. https://doi.org/10.1056/NEJMoa1415061
- 33. Jovin, T.G., Chamorro, A., Cobo, E., et al. (2015) Thrombectomy within 8 Hours after Symptom Onset in Ischemic Stroke. New England Journal of Medicine, 372, 2296-2306. https://doi.org/10.1056/NEJMoa1503780
- 34. Goyal, M., Menon, B.K., Coutts, S.B., Hill, M.D. and Demchuk, A.M. (2011) Effect of Baseline CT Scan Appearance and Time to Recanalization on Clinical Outcomes in Endovascular Thrombectomy of Acute Ischemic Strokes. Stroke, 42, 93-97. https://doi.org/10.1161/STROKEAHA.110.594481
- 35. 王霞, 朱美意. 新疆石河子地区急性脑卒中患者就诊时间及预后分析[J]. 农垦医学, 2014, 36(4): 300-305.
- 36. García-Tornel, Á., Requena, M., Rubiera, M., et al. (2019) When to Stop. Stroke, 50, 1781-1788. https://doi.org/10.1161/STROKEAHA.119.025088
- 37. 王勇, 陈胜利, 李赛男, 等. 急性缺血性卒中血管内治疗后出血转化的预测因素研究进展[J]. 当代医学, 2021, 27(18): 191-194.
- 38. Linfante, I., Starosciak, A.K., Walker, G.R., et al. (2016) Predictors of Poor Outcome despite Recanalization: A Multiple Regression Analysis of the NASA Registry. Journal of Neurointerventional Surgery, 8, 224-229. https://doi.org/10.1136/neurintsurg-2014-011525
NOTES
*通讯作者。
