Advances in Clinical Medicine
Vol.
08
No.
07
(
2018
), Article ID:
27004
,
6
pages
10.12677/ACM.2018.87107
Diagnostic Value of Ultrasound in Children with Pneumonia
Ling Zhao
Department of Imaging, Mianyang Maternity & Child Health Care Hospital, Mianyang Sichuan

Received: Aug. 27th, 2018; accepted: Sep. 21st, 2018; published: Sep. 28th, 2018

ABSTRACT
Objective: To study and analyze the value of ultrasound in treating child pneumonia. Materials and Methods: 198 cases that were clinically diagnosed as pneumonia and hospitalized in Pediatrics from January 2018 to May 2018 were included in the study. And the characteristics of lung ultrasonography were analyzed. The 198 cases got the lung X-ray examination at the same time within 6 hours after admission to compare the coincidence rate, the positive predictive value and specificity between the two. With changes in the conditions of the 198 children, the lung ultrasound was also timely reviewed. And the differences between the examination results and clinical manifestations were analyzed. Results: After comparing the results of lung ultrasonography and lung X-ray examination among the 198 children with child pneumonia, it is found that the coincidence rate and positive predictive value of ultrasonographic diagnosis in pneumonia were much higher than those of lung X-ray examination. Conclusion: Lung ultrasound has a high accuracy and sensitivity in the diagnosis of pneumonia in children, combined with a strong characteristic of reproducibility to timely observe and evaluate the inflammatory changes in children’s lungs, which helps further improve the treatment protocol and promotes the recovery of children. The effect is markedly effective.
Keywords:Ultrasonic, Children Pneumonia, Diagnosis
超声对儿童肺炎的诊断价值
赵玲
四川省绵阳市妇幼保健计划生育服务中心,影像科,四川 绵阳

收稿日期:2018年8月27日;录用日期:2018年9月21日;发布日期:2018年9月28日

摘 要
目的:研究分析超声在儿童肺炎的诊断价值。资料与方法:将2018年1月至2018年5月本院儿科住院的198例临床诊断肺炎病例纳入研究对象,分析研究其肺脏超声检查的征象特点,在此198例患儿入院后6小时内同时行肺部X线检查,对比两者的符合率、阳性预测值及特异度。并对198例患儿病情变化时及时复查肺脏超声,分析检查结果与临床表现差异值。结果:198例儿童肺炎肺脏超声检查结果及肺部X线结果比较中肺脏超声诊断符合率及阳性预测值均高于肺部X线检查。结论:肺脏超声对儿童肺炎的诊断方面具有高的准确性和敏感性,加之具有重复性强特点随时对小儿肺部炎症变化适时观察评估,以此帮助临床进一步改善治疗方案,促进患儿恢复,疗效显效。
关键词 :超声,儿童肺炎,诊断

Copyright © 2018 by author and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


1. 引言
近年来,儿科门诊及急诊的就诊量增加,以儿童肺炎患儿的增加尤为显著。近年来国外文献报道,病理情况下超声伪像可以反映肺组织和胸膜变化,可以应用于肺炎诊断 [1] 。目前肺炎的动态监测靠临床,缺乏一种安全、及时、可靠、床旁的影像学检查,针对此种情况,肺脏超声对儿童肺炎检查的应用对临床和患儿及家属都有很大的帮助。一直以来,小儿肺脏超声未引起重视,该领域相对腹部超声等比较滞后,特别是基层医院更加突出,通过本文研究分析超声在儿童肺炎的诊断价值及分析其影像表现,总结其优点,促进尚未开展小儿肺部超声检查项目的医院尽快开展此项新技术。
2. 资料与方法
2.1. 一般资料
收集2018年1月至2018年5月本院198例在我院初诊的儿童肺炎患者为研究对象。纳入标准:临床表现伴有发热,部分患儿伴有咳嗽。肺部X线检查具有典型的异常表现;血常规提示白细胞异常升高或降低;患儿家属对本次研究签署知情同意书。排除标准:排除因其它原因而引发的发热,咳嗽患儿。198例患者男103例,女95例,年龄2岁至13岁。本研究通过医院伦理委员会批准。
2.2. 仪器与方法
肺脏超声:使用迈瑞DC-N6及三星H60型彩色多普勒超声诊断仪,选用线阵探头,探头频率7.5~12 MHZ。超声检查方法为:安静状态,患儿仰卧,侧卧,俯卧或坐位。以腋前,后线为界,将肺脏分为前侧后三个区。探头与肋骨垂直或平行,分别对肺脏的每个区域进行扫查。
DR检查:所有陪同家属签署放射科X线检查知情同意书。使用ZKDR诊断仪,选取儿童体型拍摄胸部正位。
2.3. 观察指标
对比肺部X线与肺脏超声两种检查方法诊断儿童肺炎与临床诊断的结果的诊断符合率,以临床诊断为金标准,计算肺部X线与肺脏超声诊断儿童肺炎的特异度,阳性预测值。
2.4. 诊断标准
① 目前,肺实变、支气管充气征是肺炎最重要的超声征象,由Weinberg等 [2] 首次提出,同时参照《新生儿肺脏疾病超声诊断指南》 [3] 中的肺炎诊断标准。② 肺炎DR诊断标准参照徐赛英等《实用儿科放射诊断学》中的标准。③ 临床肺炎诊断标准参照第七版诸福棠实用儿科学。肺部X线与肺脏超声两种检查方法诊断儿童肺炎与临床诊断的结果的诊断符合率,以临床诊断为金标准,计算肺部X线与肺脏超声诊断儿童肺炎的特异度,阳性预测值。
2.5. 统计学方法
SPSS 20.0软件处理数据,计数资料以率的形式表示,经c2检验分析,P < 0.05表示差异有统计学意义。
3. 结果
本组198例患儿,所有患儿均在入院后6小时内进行肺脏超声及肺部X线检查,将两者检查结果进行对比及随访临床诊治结果,P < 0.05,差异有统计学意义,见表1。结果显示198例儿童肺炎肺脏超声检查结果及肺部X线检查结果比较中肺脏超声诊断符合率及阳性预测值均高于肺部X线检查。
本组病例肺部超声图像特征为:① 肺实变伴支气管充气征,实变区的边缘不规则或呈锯齿状。常见动态支气管充气征。② 胸膜线异常,A线消失,胸腔积液。
本组病例肺部X线图像特征为:① 双肺纹理增多、増粗、模糊。② 肺野内斑点状、片状密度增高影。
4. 讨论
小儿肺炎作为儿童首位致死原因,早期诊断及有效治疗尤为重要 [4] [5] 。本组病例中患儿因发热入院,如图1肺部X线示患儿左肺中下野可见大片状致密影,而在相同部位患儿肺脏超声如图2可见L6区查见实变区说明肺脏超声对儿童肺炎具有诊断价值。实际上,肺脏超声不仅仅可以对儿童肺炎做诊断,同时可以做儿童肺炎治疗的跟踪和随访,了解病人治疗改变,对于一周前一患儿发热咳嗽做了如肺部X线(图1)和肺脏超声(图2)的检查,经过一段时间治疗后,患儿发热减退,血象趋近于正常,我们再次做了肺部X线(图3)和肺脏超声(图4)复查查对比,图3示肺部表现,与上次肺部X线相比,炎性病灶大部分吸收。图4示左下肺肺间质综合征改变(较上次检查明显好转)。肺部X线与肺脏超声都说明了治疗是有效的,而且有报道肺脏超声能够降低幼儿在X线下的暴露 [6] [7] 。所以肺脏超声对于儿童肺炎是可以跟着
Table 1. Comparetion of the results of lung ultrasonography and lung X-ray examination among the 198 children with child pneumonia
表1. 198例儿童肺炎超声检查结果及肺部X线结果比较(%)
 注:双肺纹理增多,增粗,以左肺中下野为主,结构乱,左肺中野见大片状致密影,边界不清,内密度欠均匀,左侧部分心缘显示欠清,两侧肋膈角锐利。
注:双肺纹理增多,增粗,以左肺中下野为主,结构乱,左肺中野见大片状致密影,边界不清,内密度欠均匀,左侧部分心缘显示欠清,两侧肋膈角锐利。
Figure 1. X-ray characteristics of lung before treatment
图1. 治疗前肺部X线表现
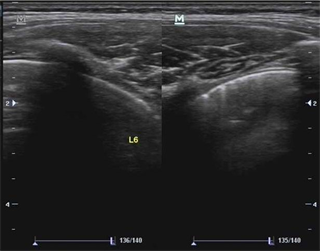
 注:左后下肺靠近膈肌处查见实变区,范围约0.6 × 0.6 cm,内可见支气管充气征,前方胸膜线增粗模糊,后方可见散在B线,A线较模糊。
注:左后下肺靠近膈肌处查见实变区,范围约0.6 × 0.6 cm,内可见支气管充气征,前方胸膜线增粗模糊,后方可见散在B线,A线较模糊。
Figure 2. Ultrasound characteristics of lung before treatment
图2. 治疗前肺部超声表现
 注:双肺纹理增多,增粗,以左肺中下野为主,结构乱,心影大小未见明显异常,两侧肋膈角锐利。
注:双肺纹理增多,增粗,以左肺中下野为主,结构乱,心影大小未见明显异常,两侧肋膈角锐利。
Figure 3. X-ray characteristics of lung after treatment
图3. 治疗后肺部X线表现
 注:左下肺胸膜稍增粗,欠光滑,见稀疏B线,未见实变区,可见肺滑动征。
注:左下肺胸膜稍增粗,欠光滑,见稀疏B线,未见实变区,可见肺滑动征。
Figure 4. Ultrasound characteristics of lung after treatment
图4. 治疗后肺部超声表现
病人的病情有直观反映的,肺脏超声在治疗反应以及随访方面作为一个可以重复无损的工具,可以非常有效帮助我们进行临床干预及指导。
肺脏超声也更容易发现隐匿性病变 [8] [9] [10] [11] ,尤其是在肺炎早期。本此小儿肺炎中部分肺部X片未见明显异常或仅表现为双肺纹理增多,增粗改变,而肺脏超声可表现为肺部小的实变区,使得小儿肺炎的阳性表现更加直观及客观。
同时对于有些肺炎患者炎症阳性表现在肺部X线中有时会因为纵隔、心脏、脊柱遮挡了,而肺脏超声由于准二维、三维支撑基础条件避开了遮挡而表现出肺部炎症征象。因此肺脏超声比肺部X线可以更敏感,更精确地发现肺部炎症的表现,这与许多学者证实超声检查对小儿肺炎诊断的敏感度均高于胸部X线检查 [12] [13] [14] 相符。
由于本文缺乏大样本儿童肺炎并发症的数据对照及其它肺部疾病的病例,具有一定局限性,有待今后进一步研究。
另外肺脏超声是一项新技术,目前并未广泛应用 [13] ,基层医院儿科超声开展应用经验少,相关专业技术人员相对不足,因此需要推广肺部超声诊断新技术及规范操作。而且对于肺部超声很容易漏诊小的实变区域,所以在临床工作中要谨慎仔细,强调系统性扫查,扫查分区应有部分重叠,而且不要漏掉背部扫查,扫查区域应有部分重叠,避免漏诊。也需要在实际工作中不断总结经验及时更新知识,与临床沟通交流,最大程度避免错诊。总之肺脏超声不仅是诊断也是监测随访儿童肺炎的首选检查方法且具有很大的应用价值。
文章引用
赵 玲. 超声对儿童肺炎的诊断价值
Diagnostic Value of Ultrasound in Children with Pneumonia[J]. 临床医学进展, 2018, 08(07): 638-643. https://doi.org/10.12677/ACM.2018.87107
参考文献
- 1. 赵倩茹, 马红彪, 付大鹏. 肺超声评估儿童肺炎的研究进展[J]. 临床儿科杂志, 2016, 34(2): 154-157.
- 2. Weinberg, B., Diakoumakis, E.E., Kass, E.G., et al. (1986) The Air Bronchogram, Sonographic Demonstration. AJR. American Journal of Roentgenology, 147, 593-595. https://doi.org/10.2214/ajr.147.3.593
- 3. 刘敬, 冯星, 等. 新生儿肺脏疾病超声诊断指南[J]. 中华实用儿科临床杂志, 2018, 33(14): 1057-1064.
- 4. Eaposito, S., Papa, S.S., Borzani, I., et al. (2014) Performance of Lung Ultrasonography in Children with Community-Acquired Pncumonia. Italian Journal of Pediatrics, 40, 37. https://doi.org/10.1186/1824-7288-40-37
- 5. Principi, N., Esposito, S. (2011) Management of Severe Commu-nity-Acquired Pncumonia of Children in Developing and Developed Countries. Thorax, 66, 815-822. https://doi.org/10.1136/thx.2010.142604
- 6. Reissig, A., Gramegna, A. and Aliberti, S. (2012) The Role of Lung Ultrasound in the Diagnosis and Follow-Up of Community-Acquired Pncumonia. European Journal of Internal Medicine, 23, 391-397. https://doi.org/10.1016/j.ejim.2012.01.003
- 7. Volpicelli, G., Elbarbaby, M., Blaivas, M., et al. (2012) Interna-tional Evidence-Based Recommendations for Point-Of-Care Lung Ultrasound. Intensive Care Medicine, 38, 577-591. https://doi.org/10.1007/s00134-012-2513-4
- 8. Lichtenstein, D., Goldstein, I., Mourgeon, E., et al. (2004) Comparative Diagnostic Performances of Ausultation, Chest Radiography, and Lung Ultrasonography in Acute Res-piratory Distress Syndrome. Anesthesiology, 100, 9-15. https://doi.org/10.1097/00000542-200401000-00006
- 9. 刘敬, 刘颖, 王华伟, 等. 肺脏超声对新生儿肺不张的诊断价值[J]. 中华儿科杂志, 2013, 51(9): 644-648.
- 10. Liu, J., Chen, S.W., Liu, F., et al. (2014) BPD, tot BPD, Oriatrogenic BPD: Findings of Lung Ultrasound Examinations. Medicine, 93, 133. https://doi.org/10.1097/MD.0000000000000133
- 11. Liu, J., Wang, Y., Fu, W., et al. (2014) Diagnosis of Neo-natal Transienttachypnea and Its Differentiation from Respiratory Distress Syndromeusing Lung Ultrasound. Medicine, 93, 197. https://doi.org/10.1097/MD.0000000000000197
- 12. Caiulo, V.A., Gargani, L., Caiulo, S., et al. (2013) Lung Ultrasound Characteristies of Community-Acquired Pncumonia in Hospitalized Children. Pediatric Pulmonology, 48, 280-287. https://doi.org/10.1002/ppul.22585
- 13. Parlamento, S., Copetti, R. and Di Bartolomeo, S. (2009) Evaluation of Lung Ultrasound for the Diagnosis of Pneumonia in the ED. American Journal of Emergency Medicine, 27, 379-384. https://doi.org/10.1016/j.ajem.2008.03.009
- 14. Reissig, A. and Kroegel, C. (2007) Sonographic Diagnosis and Follow-Up of Pncumonia: A Prospective Study. Respiration, 74, 537-547. https://doi.org/10.1159/000100427
