Advances in Clinical Medicine
Vol.08 No.04(2018), Article ID:25269,4
pages
10.12677/ACM.2018.84063
A Case of Esophageal Cyst
Beibei Yuan, Huan Liu, Jia Liu, Guangrong Dai*
Department of Gastroenterology, Affiliated Hospital of Yan’an University, Yan’an Shaanxi

Received: May 13th, 2018; accepted: May 28th, 2018; published: Jun. 5th, 2018

ABSTRACT
The patient was male, 48 years old, with intermittent upper abdominal discomfort for six months. There was no abnormality in the examination. Outpatient endoscopy showed that the nature of esophageal mucosal uplift was to be determined; endoscopic ultrasonography reported that: esophageal mucosal origin originated in the mucosal layer to consider cystic disease. Endoscopic submucosal dissection (ESD) was performed after hospital admission. The postoperative pathological examination confirmed that it was esophageal cyst.
Keywords:Esophageal Cyst, Endoscopic Ultrasound, Submucosal Dissection
食管囊肿一例
袁贝贝,刘欢,刘佳,戴光荣*
延安大学附属医院消化内科,陕西 延安

收稿日期:2018年5月13日;录用日期:2018年5月28日;发布日期:2018年6月5日

摘 要
患者男,48岁,间断性上腹部不适半年,查体未见异常。门诊胃镜检查示:食管粘膜隆起性质待定;超声内镜报告示:食管粘膜隆起源于粘膜层多,考虑囊性病。入院后行内镜下食管粘膜下病变剥离术(ESD),术后病检报告证实为:食管囊肿。
关键词 :食管囊肿,超声内镜,粘膜下剥离术

Copyright © 2018 by authors and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


1. 前言
食管囊肿也称食管重复囊肿,属于罕见的先天性前肠囊肿;食管重复囊肿的发生率为1:8200。食管重复囊肿在成人中很少见,现将我院一例成人食管囊肿病例报道如下。
2. 病例报告
患者男,48岁。因间断性上腹部不适半年余入院。门诊行胃镜检查报告示(图1):距门齿35~38 cm约7点处可见一隆起,约3.0 × 2.0 × 1.2 cm,表面光滑粘膜色泽与周围粘膜相同,活检钳按压质软;诊断:食管粘膜隆起性质待定。内镜超声报告示(图2):隆起物起源于粘膜下层,呈无回声,内部回声均匀,边缘清晰,最大截面积约12.6 × 9.8 mm;诊断:食管粘膜隆起源于粘膜下层多考虑囊性病。拟行内镜下食管粘膜下病变剥离术(ESD)治疗,术后固定标本送检,病理报告示(图3):(食管囊性病变)食管囊肿。
3. 讨论
食管囊肿也称食管重复囊肿,属于罕见的先天性前肠囊肿。在胚胎发育期间,胚胎第四至第八周期间原始前肠的背侧空泡化失败而形成的食管异常肿块,重复囊肿可发生在消化道从口腔到肛门的任何地方,食管重复囊肿在儿童中多发,男性发病率高于女性,在消化道中是第二常见的重复囊肿,在回肠段最常见,约占20%,在食管部分占10%~15% [1] 。食管重复囊肿的发生率为1:8200 [2] 。囊肿在食管下段占60%,上段占23%,中段占17%,好发于食管下段 [3] 。食管重复囊肿在成人中很少见,因为80%的囊肿在儿童时期被诊断出来并切除,小于7%的在青春期之前仍没有症状。无症状的食管囊肿在成年人中很难诊断,甚至由于症状的非特异性常被误认为其他常见的食管疾病 [4] [5] 。最常见的临床表现是上腹部不适、吞咽困难及胸骨后疼痛 [6] 。目前病例报告中,有人认为吞咽困难、胸骨后疼痛的快速发展是由囊肿快速增长所致 [4] [5] 。本例患者主要表现为上腹部不适症状。组织病理学检查是食管重复囊肿的金标准,其病理学诊断标准如下 [7] :1) 囊肿在食管内或附着于食管壁,与消化道上皮细胞相连,2) 囊肿表面有两层肌肉组织覆盖,3) 囊肿可呈球形或管状,内壁为鳞状上皮组织或与胚胎食管同样的上皮组织,即圆

Figure 1. Ordinary gastroscopy report: (The nature of esophageal mucosal uplift is to be determined)
图1. 普通胃镜报告:(食管粘膜隆起性质待定)

Figure 2. Endoscopic Ultrasound Report: Arrows indicate that the bulge originates in the submucosa Consider cystic disease
图2. 内镜超声报告:箭头指示隆起物源于粘膜下层多考虑囊性病
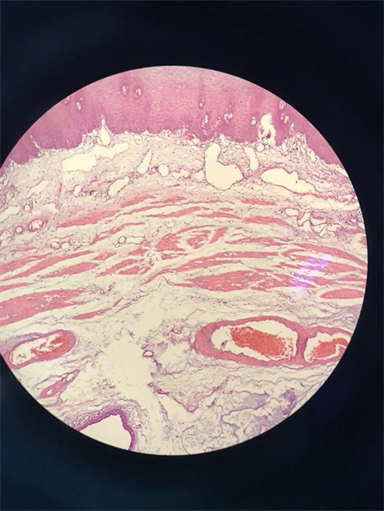
Figure 3. Pathology report (100× magnification): (Esophageal cystic lesion) Esophageal cyst
图3. 病理报告(放大100倍)示:(食管囊性病变)食管囊肿
柱状上皮、胃粘膜上皮、假复层柱状上皮或纤毛上皮组织。在本病例中,组织学检查显示囊肿起源于食管,其壁由上皮细胞排列,由两层平滑肌层组成,符合上述诊断标准。
消化道隆起性形态学病变,普通消化内镜对其有较好的诊断价值,但对于肿瘤、囊肿以及消化道管壁外的脏器或肿瘤压迫引起的隆起性病变诊断较为困难。内镜超声检查(EUS)技术,可排除体表超声检查遇到的干扰,通过调整超声的频率能够清晰地将食管管壁从黏膜到外层显示为高–低–高–低–高回声的5层结构,分别为黏膜界面层、黏膜肌层、黏膜下层、固有肌层和外膜层 [8] 。它可以定义胃肠道内壁和外壁关系,并对区分囊性和实性肿块病变很敏感,食管重复囊肿常常表现为肿瘤内部无回声或低回声囊肿改变 [9] [10] 。尽管EUS对消化道隆起性病变的检查有较高诊断价值,但其仅仅是一种影像学诊断,若能够配合内镜超声引导,对病变组织活检或细针穿刺细胞学检查,将会很大程度上提高其诊断准确性 [11] 。本病例EUS报告为无回声囊肿,大小为12.6 × 9.8 mm。
虽然食管重复囊肿是良性的,癌变非常罕见,但外文文献中已有报道肿瘤性变性 [12] [13] 。由于食管重复囊肿存在出血、感染及转变为恶性肿瘤的并发症,因此早期诊断,发现病灶,即使患者没有症状,手术切除是最常见的治疗方式 [4] [5] 。Abu-Zaid等人先曾报道一例食管复发囊肿,经手术切除治疗,但目前这种情况的治疗已从开胸手术治疗转向内镜治疗 [14] 。本患者采用内镜下食管粘膜下剥离术,对患者创伤小,将囊肿完整切除,恢复快,并发症少,可以将消化道生理功能以及解剖结构很好的保留,并且可以达到和外科手术治疗相同的效果。
文章引用
袁贝贝,刘 欢,刘 佳,戴光荣. 食管囊肿一例
A Case of Esophageal Cyst[J]. 临床医学进展, 2018, 08(04): 377-380. https://doi.org/10.12677/ACM.2018.84063
参考文献
- 1. Kawashima, S., Segawa, O., Kimura, et al. (2016) A Case of Cervical Esophageal Duplication Cyst in a Newborn Infant. Surgical Case Reports, 2, 2-3.
https://doi.org/10.1186/s40792-016-0157-2 - 2. Arbona, J.L., Fazzi, J.G. and Mayoral, J. (1984) Congenital Esophageal Cysts: Case Report and Review of Literature. American Journal of Gastroenterology, 79, 177-182.
- 3. Sodhi, K.S., Saxena, A.K., Rao, K.L., Singh, M. and Suri, S. (2005) Esophageal Duplication Cyst: An Unusual Cause of Respiratory Distress in Infants. Pediatric Emergency Care, 21, 854-856.
https://doi.org/10.1097/01.pec.0000190236.50728.0d - 4. Bagheri, R., Asnaashari, A.M. and Afghani, R. (2015) Esophageal Duplication Cyst. Asian Cardiovascular and Thoracic Annals, 23, 332-334.
https://doi.org/10.1177/0218492314530977 - 5. Castelijns, P.S., Woensdregt, K., Hoevenaars, B., et al. (2014) Intraabdominal Esophageal Duplication Cyst: A Case Report and Review of the Literature. World Journal of Gastro-intestinal Surgery, 6, 112-116.
https://doi.org/10.4240/wjgs.v6.i6.112 - 6. Obasi, P.C., Hebra, A. and Varela, J.C. (2011) Excision of Esophageal Duplication Cysts with Robotic-Assisted Thoracoscopic Surgery. JSLS, 5, 244-247.
https://doi.org/10.4293/108680811X13071180406961 - 7. Moulton, M.S.J., Moir, C., Matsumoto, J. and Thompson, D.M. (2005) Esophageal Duplication Cyst: A Rare Cause of Biphasic Stridor and Feeding Difficulty. In-ternational Journal of Pediatric Otorhinolaryngology, 69, 1129-1133.
https://doi.org/10.1016/j.ijporl.2005.03.008 - 8. 李清峰. 纵轴超声内镜指导内镜微创治疗多层次食管黏膜下肿瘤的价值研究[D]: [硕士学位论文]. 广州: 南方医科大学, 2014: 2-3.
- 9. Soares, R., Gasparaitis, A., Waxman, I., Chennat, J. and Patti, M. (2011) Esophageal Duplication Cyst. Diseases of the Esophagus, 24, E21-E22.
https://doi.org/10.1111/j.1442-2050.2010.01103.x - 10. Wiechowska-Kozłowska, A., Wunsch, E., Majewski, M. and Milkiewicz, P. (2012) Esophageal Duplication Cysts: Endosonographic Findings in Asymptomatic Patients. World Journal of Gastroenterology, 18, 1270-1272.
https://doi.org/10.3748/wjg.v18.i11.1270 - 11. Caletti, G., Zani, L., Bolondi, L., et al. (1989) Endoscopic Ultra-sonography in Diagnosis of Gastric Submucosal Tumor. Gastrointestinal Endoscopy, 35, 413-418.
https://doi.org/10.1016/S0016-5107(89)72846-7 - 12. Lecompte, J.F., Breaud, J., Pop, D., Venissac, N. and Mouroux, J. (2012) Pancreatic Adenocarcinoma Arising Fromesophageal Duplication. Annals of Thoracic Surgery, 93, 2047-2048.
https://doi.org/10.1016/j.athoracsur.2011.11.023 - 13. Liu, J.F., Liu, G. and Xu, B. (2012) Acute Respiratory Distress Caused by Esophageal Duplication Canceration in an Adult. General Thoracic and Cardiovascular Surgery, 60, 316-320.
https://doi.org/10.1007/s11748-010-0731-7 - 14. Somani, P. and Sharma, M. (2016) Endoscopic Ultrasound of Esophageal Duplication Cyst. Indian J Gastroenterol., 35, 497-498.
NOTES
*通讯作者