World Journal of Cancer Research
Vol.
09
No.
01
(
2019
), Article ID:
28149
,
5
pages
10.12677/WJCR.2019.91001
A Case of Intracranial Epidermoid Cyst and Literature Review
Weihai Liu, Wen Su, Peng Wang, Jun Yang*
Yantai Affiliated Hospital of Binzhou Medical University, Yantai Shandong

Received: Nov. 29th, 2018; accepted: Dec. 17th, 2018; published: Dec. 24th, 2018

ABSTRACT
Objective: To investigate the clinical features, imaging diagnosis and treatment of Intracranial Epidermal Cysts. Methods: The clinical manifestations, imaging findings and treatment options of one case of intracranial epidermoid cyst were analyzed and related literatures were reviewed. Results: The patient underwent craniotomy and the pathological findings showed intracranial epidermoid cysts. Conclusion: EC is a clinically rare intracranial benign tumor with no characteristic clinical manifestations. CT shows low-density images with no change in enhancement. MRI examination of Flair images and DWI images is helpful for diagnosis. Surgical treatment is preferred for treatment options.
Keywords:Brain Tumor, Epidermoid Cyst, Treatment, Literature Review
颅内表皮样囊肿一例并文献复习
刘维海,苏文,王鹏,杨军*
滨州医学院烟台附属医院,山东 烟台

收稿日期:2018年11月29日;录用日期:2018年12月17日;发布日期:2018年12月24日

摘 要
目的:探讨颅内表皮样囊肿(Epidermoid Cysts)的临床特点、影像诊断、治疗方案。方法:对收治的1例颅内表皮样囊肿临床表现、影像表现及治疗方案进行分析,并复习相关文献。结果:患者行开颅肿瘤切除术,术后病理示颅内表皮样囊肿。结论:EC是临床上比较罕见的颅内良性肿瘤,无特征性临床表现,CT显示低密度影像,增强无变化,MRI检查Flair像和DWI像有助于确诊。治疗方案首选手术治疗。
关键词 :颅脑肿瘤,表皮样囊肿,治疗,文献复习

Copyright © 2019 by authors and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


1. 引言
颅内表皮样囊肿(Epidermoid Cysts)是一种罕见的先天性良性肿瘤。发病率占全脑肿瘤的0.5%~1.8% [1]。本病多发与20~40岁年龄段,男女之间发病率无明显差异,临床中本病多见于桥小脑脚、鞍旁,也可见于四脑室、侧脑室、颅骨板障内以及脊柱。近年来,随着显微神经外科以及神经内镜技术的发展,本病的手术疗效及患者术后的生活质量有了明显的提高。现本文报道一例颅内巨大表皮样囊肿复发病例。
2. 临床资料
患者,男,54岁,因“头晕伴行走不稳5年,加重1年”就诊于滨州医学院烟台附属医院神经外科。患者轻度言语不流利,无头痛,无恶心、呕吐,无饮水呛咳,无肢体抽搐。既往20年前因小脑表皮样囊肿型开颅肿瘤切除术。吸烟40年,每日20支,未戒烟。轻度饮酒史。否认高血压、糖尿病、冠心病及周围血管病史。
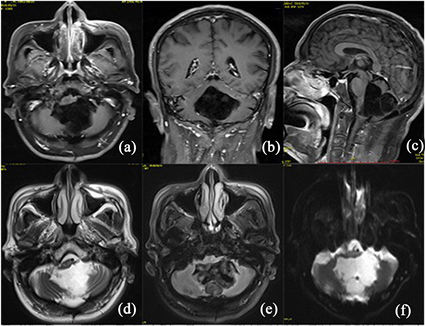
Figure 1. Axial position. (a) Coronal position. (b) Sagittal position. (c) T1WI shows that the tumor is located in the cerebellar palsy and the fourth ventricle, showing a low-density signal, with irregular medium signal shadows visible, and the brain stem is obvious. Deformed under pressure. (d) Shows that the tumor shows a high signal in the axial T2WI image, and the signal intensity in the tumor cavity is not uniform. (e) The axial position T2Flair resembles a high-low mixed-density signal in which the tumor appears to be flocculated. (f) DWI image shows a high signal of mixed density in the tumor area
图1. 轴位(a)、冠状位(b)、矢状位(c)T1WI示肿瘤位于小脑蚓、四脑室,呈现低密度信号,内可见不规则中等信号影,脑干明显受压变形。(d) 轴位T2WI像可见肿瘤表现为高信号,瘤腔内信号强度不均匀。(e) 轴位T2Flair像肿瘤表现为絮状不均匀的高低混合密度信号。(f) DWI像可见瘤区呈现混杂密度的高信号
查体:生命体征平稳,体温:36.5℃,心率:72次/分,呼吸:18次/分,血压:120/70 mmHg。神志清,精神一般,自然睁眼,对答切题,遵嘱动作。双侧瞳孔等大等圆,直径约3 mm,对光反射及调节均正常。颈后可见陈旧性手术瘢痕,四肢肌力V级,肌张力正常。神经系统查体未见明显阳性体征。实验室检查示乙肝大三阳:HBsAg: >250 ng/ml,HBeAg: 1066.24 PEI/ml,HBcAb: 8.71 PEI/ml。心电图、胸片未见明显异常。颅脑MRI平扫 + 增强(图1):小脑蚓、四脑室为中心见大小约4.8 × 5.7 cm混杂长T1长T2异常信号,小脑蚓后部病灶内见小片状短T1信号,DWI呈混杂高信号,注入对比机未见明显强化,病灶向临近间隙延伸,局部结构受压。诊断:小脑表皮样囊肿。
患者于入院后第6天在全身麻醉下行后颅凹肿瘤切除术,全身麻醉成功后,患者右侧侧俯卧位,头钉固定于头架上,取枕下后正中原切口,切口长约9 cm,依次切开头皮、皮下组织、帽状腱膜,高频电刀切开枕部肌肉及其筋膜、骨膜,可见原枕部骨窗约3 cm,人工脑膜部分覆盖,部分小脑半球裸露。术中见:病灶位于小脑半球,肿物约5 × 5 × 5 cm大小,与小脑及脑干关系紧密,脑干受压变薄。瘤腔内见银白色蜡样脑组织,质软(图2)。肿瘤钳夹除肿瘤组织,刮匙刮除边缘区肿瘤组织,取部分肿瘤组织送检,近全切除肿瘤。手术顺利,术后给予脱水、抗感染、营养神经、抗癫痫治疗。术后病理示表皮样囊肿(图3)。术后1 d复查颅脑CT示颅内肿瘤次全切除(图4)。
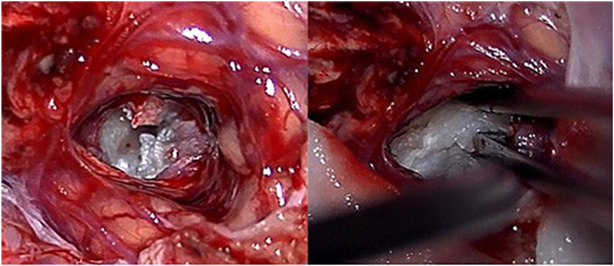
Figure 2. Silver-white, waxy tumor tissue in the tumor cavity
图2. 瘤腔内银白色、蜡样肿瘤组织

Figure 3. Cerebellum (cyst), covered with stratified squamous epithelium, containing a large amount of keratin, consistent with squamous epithelial cysts
图3. 小脑(囊肿),囊壁被覆复层鳞状上皮,内含大量角质物,符合鳞状上皮囊肿

Figure 4. Reexamination of the brain CT for 1 day after surgery shows subtotal resection of the tumor
图4. 术后1天复查颅脑CT示肿瘤次全切除
3. 讨论
表皮样囊肿(Epidermoid Cysts)起源于异位表皮细胞。其外形可为分叶状或菜花状,表面覆以菲薄的包膜,境界清楚,外观呈珍珠样,带有白色光泽,质软,囊内充满松软、蜡状或片状透明角质物。被称为“最美丽的肿瘤” [2]。分为先天性和继发性两种,前者起源于颅内残余的上皮母细胞。是在胚胎3~5周神经管闭合期,继发性脑细胞形成时,来源于神经嵴的外胚层上皮组织细胞异位残留所致,并通过不断的上皮细胞脱落,产生角蛋白和胆固醇积聚于瘤内,使肿瘤不断缓慢增长 [3]。后者多因外伤、手术或腰椎穿刺等操作将皮肤组织异位带入所致 [4]。该病年龄分布甚广,可发生与任何年龄,最多见于50~60岁,高峰年龄可在40岁 [5]。小脑桥脑角、鞍旁、鞍上池为其好发部位 [6]。表皮样囊肿临床上无特征性症状,具体因肿瘤生长部位不同而异。肿瘤生长缓慢,但对周围组织的破坏性较强,也有炎症作用,常表现为无菌性脑膜炎反复发作。虽然表皮样囊肿属良性病变,但也存在恶变可能 [7]。恶性变以鳞状细胞癌最为常见,可见于原发性恶性变 [8] ,也可见于术后残留组织恶性变 [9]。
表皮样囊肿结合病史及CT、MRI检查一般诊断并不困难,CT囊肿显示为低密度影像。MRI检查中表皮样囊肿在T1WI上显示低信号,T2WI为高信号 [10]。有文献表明FLAIR序列在显示表皮样囊肿方面要优于T1、T2序列 [11]。DWI序列呈显著高信号,在与颅内其他囊性病变的鉴别上具有重要参考价值 [12]。
表皮样囊肿的治疗目前首选手术切除,由于表皮样囊肿具有“见缝就钻”的特性 [13] ,因此术中应注意防止肿瘤碎屑随脑脊液扩散,仔细清除囊肿内容物后,对无粘连的囊壁部分,尽可能广泛切除,用生理盐水反复冲洗,也有作者主张用含地塞米松的生理盐水冲洗 [14]。除传统的开颅肿瘤切除术外,神经内镜技术在治疗颅内表皮样囊肿中的应用越来越广泛 [15]。无菌性脑膜炎为本病最常见的术后并发症。表皮样囊肿属良性肿瘤,术后预后一般较好,若肿瘤能大部分切除,一般恢复良好,复发亦较晚。
在本例病例中,患者病变位于四脑室,但巨大的肿瘤实体并未堵塞中脑导水管引起脑积水,患者仅仅表现为小脑受压引起的步态不稳,考虑与肿瘤呈分叶状有关,脑脊液从肿瘤间隙流通,并未引起阻塞症状。根据患者MR影像定位,选取枕下正中入路,此处距离肿瘤位置最近,以利于肿瘤的暴露及切除。患者肿瘤压迫脑干十分严重,从影像学观察脑干最薄处仅为1 cm左右,术中并未强求全切肿瘤,且在处理靠近脑干部分的肿瘤时并未强行牵拉肿瘤组织,以免术后脑干塌陷引起呼吸循环衰竭。术中采用含有地塞米松的生理盐水反复冲洗瘤腔,避免残余囊肿内容物对脑组织的刺激,术后放置引流以利于术腔内残余碎屑的流出。
综上所述,颅内表皮样囊肿是一种良性肿瘤,起病缓慢,多以继发性临床表现为主。核磁共振特别是DWI像对本病的诊断具有重要意义。主要治疗方式首选手术切除病灶,在不影响重要血管、神经的前提下,应尽可能的全切肿瘤。肿瘤的术后并发症以术后迟发性出血、无菌性脑炎多见,减少术后并发症的发生对提高患者术后的生活质量具有重要意义。
文章引用
刘维海,苏 文,王 鹏,杨 军. 颅内表皮样囊肿一例并文献复习
A Case of Intracranial Epidermoid Cyst and Literature Review[J]. 世界肿瘤研究, 2019, 09(01): 1-5. https://doi.org/10.12677/WJCR.2019.91001
参考文献
- 1. Wang, Z. (2009) Wang Zhongcheng Neurosurgery. Hubei Science and Technology Publishing, Wuhan, 715.
- 2. Cruveilhier, J. (1829) Anatomie pathologique du corps humain. Bailliere, Paris.
- 3. Cobbs, C.S., Pitts, L.H. and Wilson, C.B. (1997) Epidermoid and Dermoid Cysts of the Posterior Fossa. Clinical Neurosurgery, 44, 511-528.
- 4. Per, H., Kumandaş, S., Gümüs, H., et al. (2007) Iatrogenic Epidermoid Tumor: Late Complication of Lumbar Puncture. Journal of Child Neurology, 22, 332-336.
https://doi.org/10.1177/0883073807300531 - 5. Sabin, H.I., Bordi, L.T. and Symon, L. (1987) Epidermoid Cysts and Cholesterol Granulomas Centered on the Posterior Fossa: Twenty Years of Diagnosis and Management. Neurosurgery, 21, 798-805.
https://doi.org/10.1227/00006123-198712000-00004 - 6. Nagasawa, D., Yew, A., Safaee, M., et al. (2011) Clinical Characteristics and Diagnostic Imaging of Epidermoid Tumors. Journal of Clinical Neuroscience, 18, 1158-1162.
https://doi.org/10.1016/j.jocn.2011.02.008 - 7. Vellutini, E.A.S., De Oliveira, M.F., Ribeiro, A.P.C., et al. (2014) Ma-lignant Transformation of Intracranial Epidermoid Cyst. British Journal of Neurosurgery, 28, 507-509.
https://doi.org/10.3109/02688697.2013.869552 - 8. Kim, M.-S. and Kim, O.-L. (2008) Primary Intracranial Squamous Cell Carcinoma in the Brain Stem with a Cerebellopontine Angle Epidermoid Cyst. Journal of Korean Neurosurgical Society, 44, 401-404.
https://doi.org/10.3340/jkns.2008.44.6.401 - 9. Nakao, Y., Nonaka, S., Yamamoto, T., et al. (2010) Malignant Trans-formation 20 Years after Partial Removal of Intracranial Epidermoid Cyst. Neurologia Medico-Chirurgica, 50, 236-239.
https://doi.org/10.2176/nmc.50.236 - 10. Osborn, A.G. and Preece, M.T. (2006) Intracranial Cysts: Radiolog-ic-Pathologic Correlation and Imaging Approach. Radiology, 239, 650-664.
https://doi.org/10.1148/radiol.2393050823 - 11. Hakyemez, B., Aksoy, U., Yildiz, H., et al. (2005) Intracranial Epi-dermoid Cysts: Diffusion-Weighted, FLAIR and Conventional MR Findings. European Journal of Radiology, 54, 214-220.
https://doi.org/10.1016/j.ejrad.2004.06.018 - 12. Kara Bozkurt, D., Gok, M., Erdem, A., et al. (2015) Diagnostic Im-portance of Flair and Diffusion Weighted Magnetic Resonance Imaging of the Atypic Intracranial Epidermoid Cysts. Journal of Academic Research in Medicine, 5, 134-138.
https://doi.org/10.5152/jarem.2015.686 - 13. Czernicki, T., Kunert, P., Nowak, A., et al. (2016) Epidermoid Cysts of the Cerebellopontine Angle: Clinical Features and Treatment Outcomes. Neu-rologia i Neurochirurgia Polska, 50, 75-82.
https://doi.org/10.1016/j.pjnns.2015.11.008 - 14. Schiefer, T.K. and Link, M.J. (2008) Epidermoids of the Cerebellopontine Angle: A 20-Year Experience. Surgical Neurology, 70, 584-590.
https://doi.org/10.1016/j.surneu.2007.12.021 - 15. Singh, I., Rohilla, S., Kumar, P., et al. (2018) Combined Microsur-gical and Endoscopic Technique for Removal of Extensive Intracranial Epidermoids. Surgical Neurology International, 9, 36.
NOTES
*通讯作者。