Hans Journal of Surgery
Vol.06 No.03(2017), Article ID:20973,10
pages
10.12677/HJS.2017.63004
A Meta-Analysis of Near-Long-Term Efficacy of Coronary Artery Bypass Grafting and Drug-Eluting Stent in Elderly Patients
Lingtong Shan1, Qi Wang2, Yujie Xiao1, Yi Pan1, Feng Wei1, Mingming Nan3, Jun Wang4*
1The First Clinical Medical College, Nanjing Medical University, Nanjing Jiangsu
2The College of Forensic Medicine and Medical Examiner, Jining Medical University, Jining Shandong
3The College of Nursing, Nanjing Medical University, Nanjing Jiangsu
4Department of Cardiothoracic Surgery, The First Affiliated Hospital of Nanjing Medical University, Nanjing Jiangsu

Received: May 20th, 2017; accepted: Jun. 12th, 2017; published: Jun. 15th, 2017

ABSTRACT
Objective: To evaluate the near-long-term efficacy of coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) in the elderly (age ≥ 75 years). Methods: We searched relevant literatures in MEDLINE (via pubmed), EMBASE, Cochrane Library from the time of building to 2017. Meanwhile, we collected conference records or gray literature from cardiovascular congresses to compare CABG and PCI for elderly patients. Meta analysis was performed using Review Manager 5.3 software. Results: A total of 12 articles were included in the meta-analysis, all of which were observational studies and randomized controlled studies (RCTs) were not retrieved. A total of 6877 patients were enrolled in this meta-analysis, of which 3460 (50.31%) were CABG. Meta- analysis showed that the long-term mortality rate (OR = 1.29, 95% CI (1.07, 1.57), P = 0.009) and the incidence rate of revascularization (OR = 5.88, 95% CI (4.68, 7.38), P < 0.00001) have significant difference between CABG group and PCI group. However, in-hospital mortality rate (OR = 0.78, 95% CI (0.56, 1.08), P = 0.14), the incidence rate of MACCE (OR = 1.01, 95% CI (0.88, 1.17), P = 0.87) and the incidence rate of MI (OR = 1.25, 95% CI (0.68, 2.30), P = 0.46) have not significant difference between CABG group and PCI group. Conclusions: Compared with PCI, CABG can reduce the long-term mortality rate and the incidence rate of TLR in elderly patients, but more and more randomized controlled trials are still needed for further verification.
Keywords:Coronary Artery bypass Grafting, Percutaneous Coronary Intervention, Elderly, Efficacy, Meta-Analysis
高龄患者冠状动脉旁路移植术与置入药物洗脱支架术后近远期疗效比较的Meta分析
单龄童1,王琪2,肖雨洁1,潘毅1,魏枫1,南明明3,王俊4*
1南京医科大学第一临床医学院,江苏 南京
2济宁医学院法医学与医学检验学院,山东 济宁
3南京医科大学护理学院,江苏 南京
4南京医科大学第一附属医院胸心外科,江苏 南京

收稿日期:2017年5月20日;录用日期:2017年6月12日;发布日期:2017年6月15日

摘 要
目的:系统评价高龄(年龄 ≥ 75岁)患者冠状动脉旁路移植术(coronary artery bypass grafting, CABG)与行经皮冠状动脉介入(percutaneous coronary intervention, PCI)下置入药物洗脱支架(drug eluting stent, DES)术后近远期疗效。方法:利用计算机检索MEDLINE(via pubmed,建库至2017年2月)、EMBASE (建库至2017年2月)、Cochrane Library (建库至2017年2月),并辅助以手动检索会议记录或灰色文献,收集研究高龄患者CABG与PCI下置入DES术后死亡率、主要不良心脑血管事件(main adverse cardiovascular and cerebrovascular events, MACCE)、心肌梗死(myocardial infarction, MI)以及靶病变再次血运重建(target lesion revascularization, TLR)发生率对比的英文文献资料。采用Review Manager 5.3软件进行meta分析。结果:共纳入12篇文献进入meta分析,均为观察性研究,未检索到随机对照研究(randomized controlled study, RCT)。本meta分析共纳入6877例患者,其中CABG组3460例(50.31%)。Meta分析结果表明:两组患者术后远期死亡率(OR = 1.29, 95%CI (1.07, 1.57), P = 0.009)以及TLR发生率(OR = 5.88, 95%CI (4.68,7.38), P < 0.00001)的差异具有统计学意义,院内死亡率(OR = 0.78, 95%CI (0.56,1.08), P = 0.14)、MACCE发生率(OR = 1.01, 95%CI (0.88, 1.17), P = 0.87)以及MI发生率(OR = 1.25, 95%CI (0.68, 2.30), P = 0.46)差异不具有统计学意义。结论:与PCI相比,CABG能明显减低高龄患者术后远期死亡率以及血运重建发生率,但仍有待于更多更大的随机对照试验以进一步验证。
关键词 :冠状动脉旁路移植术,经皮冠状动脉介入,高龄,疗效,meta分析

Copyright © 2017 by authors and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


1. 引言
随着老年化进程的加速,冠状动脉粥样硬化性心脏病(coronary artery disease,CAD)已成为全球最突出的健康问题之一 [1] 。有资料表明,由CAD导致的死亡数在过去的20年里增加了40% [2] 。人口激增、高危险因素如吸烟,高胆固醇水平是导致死亡人数增长的部分原因 [3] [4] ,这些问题在亚洲人口中尤为突出 [5] [6] [7] [8] 。
上世纪五十年代,体外循环(cardiopulmonary bypass, CPB)技术开始应用于人类,其后随着CPB技术的发展,CPB被广泛用于冠状动脉旁路移植术(coronary artery bypass grafting,CABG) [9] 。此后开始出现非体外循环冠状动脉旁路移植技术(off-pump coronary artery bypass surgery, OPCAB),极为有效地减少了心肌缺血再灌注损伤,使得CABG更为安全有效 [10] 。在过去的几十年里,CABG已逐渐成为一种安全有效的标准术式。由于CABG手术创伤较大,老年患者特别是高龄患者难以耐受。PCI技术因其创伤小、院内死亡率低得以产生并迅速发展。该项技术开始时仅限于球囊成形术,随着社会的发展,现在PCI还拥有了包括斑块销蚀技术、支架植入术等在内的多项新技术 [11] 。药物洗脱支架的发明使得药物可自聚合物涂层中通过洗脱的方式有控制的释放,是介入心脏病学又一重大突破。PCI也逐渐与CABG、内科药物治疗一起成为目前治疗CAD的三大主要治疗手段。
本研究纳入了2017年2月1日之前样本量大于10且临床资料齐全的相关英文研究文献进行meta分析,试图比较高龄患者行CABG与PCI下置入DES术后近远期临床疗效的关系,以期能为治疗高龄CAD患者的临床工作做出指导。
2. 材料与方法
2.1. 材料
纳入标准:①在英文期刊杂志上发表的提供完整数据的临床研究;②研究CABG与PCI下置入DES治疗高龄(年龄 ≥ 75岁) CAD患者临床疗效的比较;③提供术后死亡率、MI、TLR以及MACCE发生率数据;排除标准:①研究样本量低于10;②发表的病例报道、综述、动物研究;③重复发表。若有一个研究组对同一队列患者的不同随访时期的研究,则选择最近发表的一篇。
临床结局:①院内死亡率:院内或术后30天内全因死亡;②心梗;③靶病变再次血运重建;④主要不良心脑血管事件:死亡、非致死性心肌梗死、再次血运重建以及脑卒中、脑出血等;⑤远期死亡率:随访结束时的死亡率。
本研究严格遵守PRISMA声明进行meta分析。
2.2. 方法
2.2.1. 检索策略
利用计算机检索MEDLINE(via pubmed,建库至2017年2月)、EMBASE(建库至2017年2月)、Cochrane Library (建库至2017年2月),并辅助以手动检索会议记录或灰色文献,纳入符合标准的英文研究文献资料。以检索词“coronary artery bypass grafting”、“percutaneous coronary intervention”和“drug eluting stent”在三大数据库中进行检索,其中MEDLINE (via pubmed)具体检索策略见表1。
2.2.2. 数据提取与研究质量评价
由两名调查者(单龄童,肖雨洁)依据检索策略独立进行文献检索并提取文献中数据资料录入EXCEL表格,如两名调查者发生分歧则与第三名调查者讨论决定。(文献检索与纳入流程图见图1)提取资料包括三个部分:①研究文献的基本资料(研究者、发表年份、国籍、样本量) ②研究对象基线资料(年龄、性别)③临床结局。利用Newcastle-Ottawa量表对纳入的观察性临床研究进行质量评价:病例组和对照组的选择(0~4星),可比性(0~2星),结局(0~3星) (表2)。
2.2.3. 统计学方法
按照Cochrane手册的指南,进行数据提取与计算。通过卡方检验和I2检验进行异质性检验,按

Figure 1. Flow chart
图1. 流程图
Table 1. Retrieve policy of MEDLINE (via pubmed)
表1. MEDLINE(via pubmed)检索策略
Table 2. The Newcastle-Ottawa scale of the study included
表2. 纳入研究的Newcastle-Ottawa量表评价
Cochrane手册认为,P > 0.1和I2 < 50%时,异质性可以接受,并采用固定效应模型计算比值比(OR)和95%可信区间(CI),显著性水平设定为0.05,绘制森林图展示合并数据后对比的结果。反之,异质性较大时,采用随机效应模型。纳入研究数量大于10时,利用漏斗图直观检测发表偏倚。本研究所有统计分析均由Review Manager 5.3软件完成。
3. 结果
3.1. 纳入文献一般资料
本研究总计纳入了12项研究 [12] - [23] ,共纳入6877例患者。其中3460例(50.31%)接受了CABG治疗,3427例(49.69%)接受了PCI下置入DES治疗。纳入的12项研究均为观察性研究,其中9项研究报道了患者术后院内死亡率,8项研究报道了患者随访期间MACCE发生率,9项研究报道了患者心肌梗死情况,10项研究报道了患者靶病变再次血运重建情况,9项研究报道了患者随访结束时的死亡情况(表3)。
3.2. meta分析结果
对报道了患者术后院内死亡率的9项研究进行院内死亡率荟萃分析显示PCI相比于CABG能降低高龄CAD患者院内死亡率(OR = 0.78, 95%CI (0.56,1.08), P = 0.14),但两者间差异没有统计学意义。各研究间无明显异质性(P = 0.15, I2 = 33%) (图2)。
对报道了患者随访期间MACCE发生率的8项研究进行荟萃分析显示PCI相比于CABG对高龄CAD患者随访期间MACCE发生率的降低并没有显示出优势(OR = 1.01, 95%CI (0.88,1.17), P = 0.87),且差异无统计学意义。各研究间无明显异质性(P = 0.54,I2 = 0%) (图3)。
对报道了患者心肌梗死情况的9项研究进行荟萃分析显示PCI相比于CABG增加了高龄CAD患者心肌梗死发生率(OR = 1.25, 95%CI (0.68,2.30), P = 0.46),但差异有统计学意义。各研究间存在异质性(P = 0.0001, I2 = 74%) (图4)。
对报道了患者靶病变再次血运重建情况的10项研究进行荟萃分析显示CABG相比于PCI能显著的降低CAD患者术后靶病变再次血运重建发生率(OR = 5.88, 95% CI (4.68,7.38), P < 0.00001),且差异有统计学意义。各研究间无明显异质性(P = 0.12,I2 = 36%) (图5)。
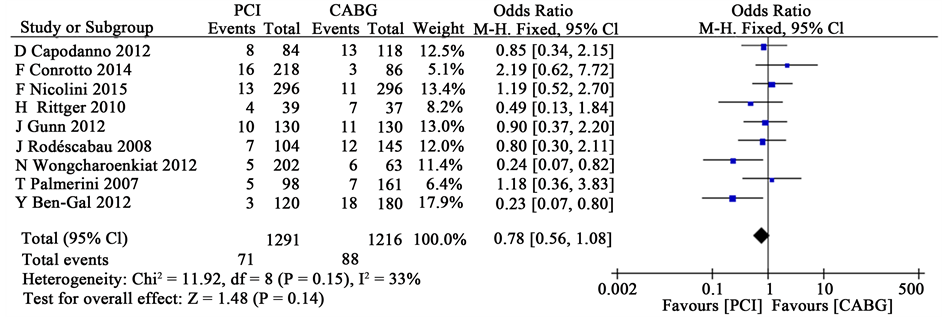
Figure 2. A meta-analysis of in-hospital mortality rate in both groups
图2. 两组患者院内死亡率荟萃分析
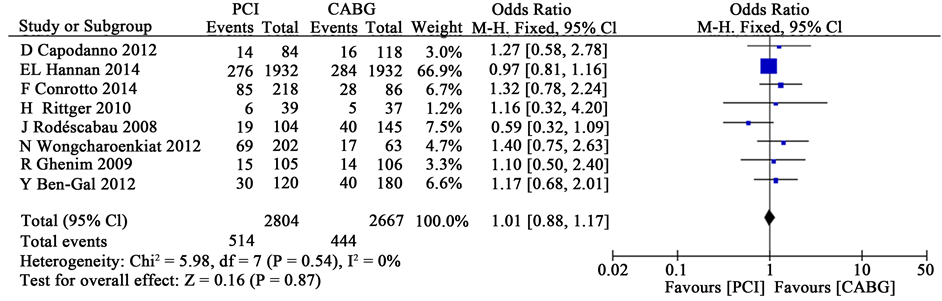
Figure 3. A meta-analysis of the incidence rate of MACCE in both groups
图3. 两组患者术后MACCE发生率荟萃分析
Table 3. The baseline data of the study included
表3. 纳入文献的基线资料
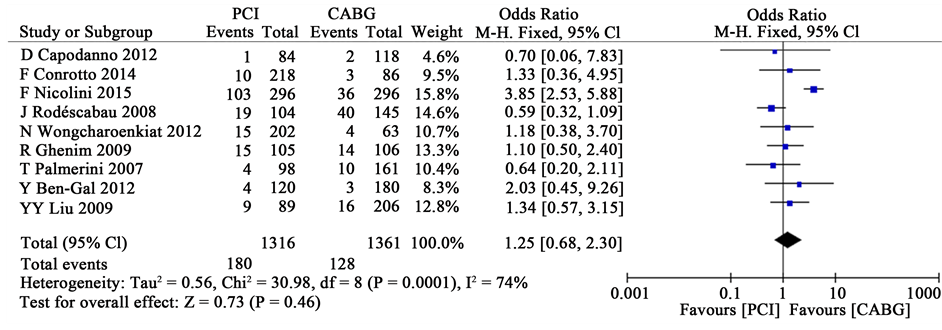
Figure 4. A meta-analysis of the incidence rate of MI in both groups
图4. 两组患者术后MI发生率荟萃分析
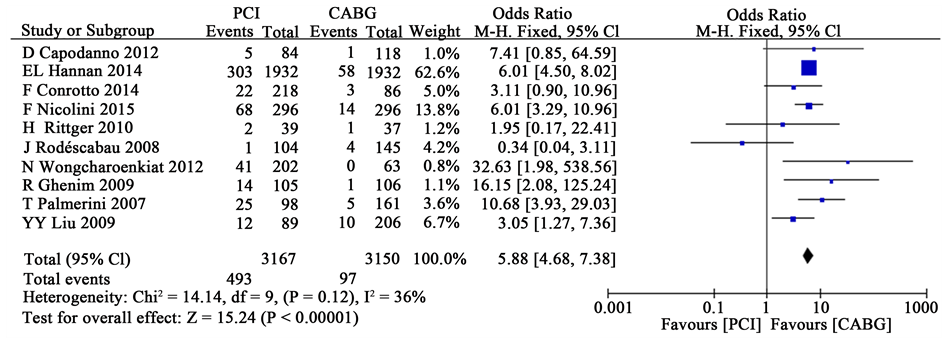
Figure 5. A meta-analysis of the incidence rate of TLR in both groups
图5. 两组患者术后靶病变再次血运重建发生率荟萃分析
对报道了患者远期死亡率的9项研究进行荟萃分析显示CABG相比于PCI能显著的降低CAD患者远期死亡率(OR = 1.29, 95%CI (1.07,1.57), P = 0.009),且差异有统计学意义。各研究间无明显异质性(P = 0.40, I2 = 4%) (图6)。
3.3. 敏感性分析与发表偏倚
剔除其中一项研究重新分析以进行敏感性分析,本研究剔除任一研究均未对结果产生较大影响,不能改变总体统计学结果。通过软件制作漏斗图以检测是否存在发表偏倚,本研究中以靶病变再次血运重建发生率作为临床结局制作的漏斗图显示有一项研究落在95%可信区间外(1/10, 10%),提示可能存在异质性与发表偏倚(图7)。
4. 讨论
CAD是冠状动脉粥样硬化引起官腔狭窄、阻塞,导致心肌缺血、缺氧的心脏病,严重危害着人类健康 [24] 。据既往研究报道,冠心病导致的死亡居全球全因病死率前列,特别是在人口老年化严重的西方发达国家,有近80%的老年患者死亡CAD [25] 。在我国,目前约有2.9亿心血管疾病患者,死亡率高居各类疾病之首,形势十分严峻 [26] 。

Figure 6. A meta-analysis of long-term mortality rate in both groups
图6. 两组患者术后远期死亡率荟萃分析
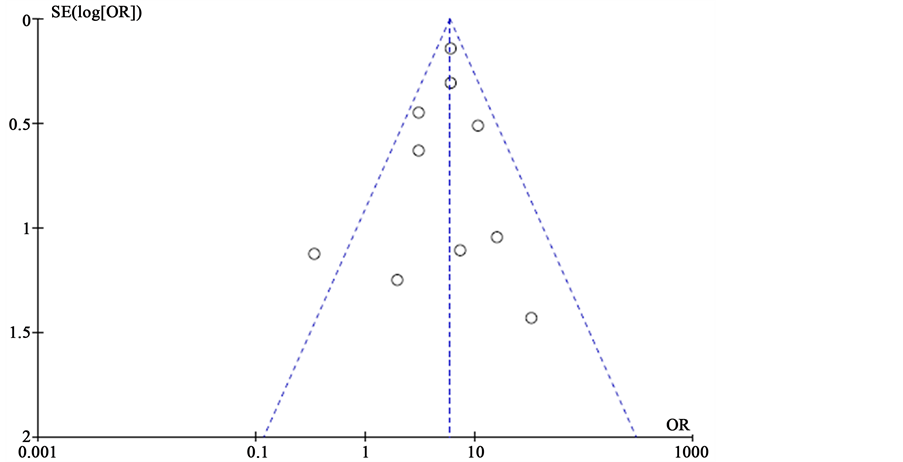
Figure 7. Funnel map
图7. 漏斗图
内科药物治疗、CABG与PCI是三种主要的治疗CAD的手段。药物治疗原则是缓解症状、纠正缺血、预防心脑血管不良事件进而改善患者生活质量,近来药物治疗多作为CABG与PCI的辅助治疗 [27] 。
CABG与PCI已被广泛应用于临床,其临床疗效已得到肯定。既往已有meta分析 [28] [29] 聚焦于CAD患者CABG与DES的近远期临床疗效对比,认为PCI能有效降低CAD患者术后院内死亡率,但在术后靶病变再次血运重建方面与CABG的比较仍有待讨论。
既往的系统综述与荟萃分析很少关注于高龄患者群体 [28] [29] ,本文纳入了2017年2月1日之前样本量大于10且临床资料齐全的相关英文研究文献进行meta分析,试图比较高龄患者行CABG与PCI下置入DES术后近远期临床疗效的关系,以期能为治疗高龄CAD患者的临床工作做出指导。本研究分析表明:CABG能明显减低高龄患者术后远期死亡率以及血运重建发生率,PCI下置入DES在减低院内死亡率、MI发生率、MACCE发生率、TLR发生率方面对比CABG具有的优势不具有统计学意义。因此我们认为PCI对于高龄虽然在近期安全性方面具有优势,但其远期疗效不如CABG。
本研究中纳入的研究资料均为观察性研究,未检索到随机对照试验研究。各研究间的研究设计、患者基线资料、研究终点、随访时长等方面存在着差异,这也是meta分析方法的局限性。异质性分析也发现在本研究中可能存在着发表偏倚。这些因素可能会对本研究的结论产生一定影响。
CABG尽管在高龄患者术后院内死亡率等方面表现劣于PCI下置入DES,但其能够有效降低远期死亡率、靶病变再次血运重建发生率。该结论仍然需要更大规模的临床随机对照试验来进一步证明。
致谢
感谢南京医科大学附属淮安市第一人民医院教学办程劲松老师、司北老师以及陈梅老师在本文写作中提供的帮助与指导。
文章引用
单龄童,王琪,肖雨洁,潘毅,魏枫,南明明,王俊. 高龄患者冠状动脉旁路移植术与置入药物洗脱支架术后近远期疗效比较的Meta分析
A Meta-Analysis of Near-Long-Term Efficacy of Coronary Artery Bypass Grafting and Drug-Eluting Stent in Elderly Patients[J]. 外科, 2017, 06(03): 21-30. http://dx.doi.org/10.12677/HJS.2017.63004
参考文献 (References)
- 1. Bengal, Y., Finkelstein, A., Banai, S., et al. (2012) Surgical Myocardial Re-vascularization versus Percutaneous Coronary Intervention with Drug-Eluting Stents in Octogenarian Patients. Heart Surgery Forum, 15, 204-209. https://doi.org/10.1532/HSF98.20111190
- 2. Gunn, J., Kuttila, K., Vasques, F., et al. (2012) Comparison of Results of Coro-nary Artery Bypass Grafting versus Percutaneous Coronary Intervention in Octogenarians. American Journal of Cardiology, 110, 1125-1129.
- 3. Rodéscabau, J., Deblois, J., Bertrand, O.F., et al. (2008) Nonrandomized Comparison of Coronary Artery Bypass Surgery and Percutaneous Coronary Intervention for the Treatment of Unprotected Left Main Coronary Artery Disease in Octogenari-ans. Circulation, 118, 2374-2381. https://doi.org/10.1161/CIRCULATIONAHA.107.727099
- 4. Nicolini, F., Contini, G.A., Fortuna, D., et al. (2015) Coronary Artery Surgery versus Percutaneous Coronary Intervention in Octogenarians: Long-Term Results. The Annals of Thoracic Surgery, 99, 567-574.
- 5. Hannan, E.L., Zhong, Y., Berger, P.B., et al. (2014) Comparison of Intermedi-ate-Term Outcomes of Coronary Artery Bypass Grafting versus Drug-Eluting Stents for Patients ≥ 75 Years of Age. American Journal of Cardiology, 113, 803-812. https://doi.org/10.1016/j.amjcard.2013.11.035
- 6. Capodanno, D., Caggegi, A., Capranzano, P., et al. (2012) Comparative One-Year Effectiveness of Percutaneous Coronary Intervention versus Coronary Artery Bypass Grafting in 2012 Patients < 75 versus ≥ 75 Years with Unprotected Left Main Disease (from the CUSTOMIZE Registry). American Journal of Cardiology, 110, 1452-1458. https://doi.org/10.1016/j.amjcard.2012.07.005
- 7. Kundi, H., Kiziltunc, E., Cetin, M., et al. (2016) Association of Monocyte/HDL-C Ratio with SYNTAX Scores in Patients with Stable Coronary Artery Disease. Herz, 41, 1-7. https://doi.org/10.1007/s00059-015-4393-1
- 8. Rittger, H., Rieber, J., Kögler, K., et al. (2011) Clinical Outcome and Quality of Life after Interventional Treatment of Left Main Disease with Drug-Eluting-Stents in Comparison to CABG in Elderly and Younger Patients. Clinical Research in Cardiology, 100, 439-446.
- 9. Rabeh, G.M.D., Jérôme, R.M.D., Amir, M.T.M., et al. (2009) One-Year Follow-Up of Nonrandomized Comparison between Coronary Artery Bypass Grafting Surgery and Drug-Eluting Stent for the Treatment of Unprotected Left Main Coronary Artery Disease in Elderly Patients (Aged ≥ 75 Years). Journal of Interventional Cardiology, 22, 520-526. https://doi.org/10.1111/j.1540-8183.2009.00503.x
- 10. Liu, Y.Y., Zhou, Y.J., Wang, Z.J., et al. (2009) Comparison between Drug Eluting Stent and Coronary Artery Bypass Grafting Surgery for the Treatment of Unprotected Left Main Coronary Artery Disease in Elderly Patients. Zhong Hua Xin Xue Guan Bing Za Zhi, 24, 769-772.
- 11. Palmerini, T., Barlocco, F., Santarelli, A., et al. (2007) A comparison between Coronary Artery Bypass Grafting Surgery and Drug Eluting Stent for the Treatment of Unprotected Left Main Coronary Artery Disease in Elderly Patients. Oxford University Press, Oxford.
- 12. Wongcharoenkiat, N., Tresukosol, D., Lak-sanabunsong, P. and Udompunturak, S. (2012) A Comparison of Outcomes between Percutaneous Coronary Intervention versus Cor-onary Artery Bypass Surgery in Octogenarian Patients. Journal of the Medical Association of Thailand, 95, 154-168.
- 13. Naghavi, M., Wang, H., Lozano, R. and Davis, A. (2013) GBD Mortality and Causes of Death Collaborators. Global, Regional, and National Levels of Age-Sex Specific All-Cause and Cause-Specific Mortality for 240 Causes of Death, 1990-2013: A Systematic Analysis for the Global Burden of Disease Study 2013. The Lancet, 385, 117-171.
- 14. Mahmoud, A.N., Elgendy, I.Y., Mentias, A., et al. (2017) Percutaneous Coronary Intervention or Coronary Artery Bypass Grafting for Unpro-tected Left Main Coronary Artery Disease.
- 15. Hanna, I.R. and Wenger, N.K. (2005) Secondary Prevention of Coronary Heart Dis-ease in Elderly Patients. American Family Physician, 71, 2289-2296.
- 16. 陈伟伟. 中国心血管病报告2015. 中华医学信息导报. 2016(12): 11-12.
- 17. Shen, W., Aguilar, R., Montero, A.R., et al. (2017) Acute Kidney Injury and in Hospital Mortality after Coro-nary Artery Bypass Graft versus Percutaneous Coronary Intervention: A Nationwide Study. American Journal of Nephrology, 45, 217-230. https://doi.org/10.1159/000455906
- 18. Fanari, Z., Weiss, S.A., Zhang, W., Sonnad, S.S. and Weintraub, W.S. (2015) Comparison of Percutaneous Coronary Intervention with Drug Eluting Stents versus Coronary Artery Bypass Grafting in Patients with Multivessel Coronary Artery Disease: Meta-Analysis of Six Randomized Controlled Trials. Cardiovascular Revascularization Medi-cine Including Molecular Interventions, 16, 70-77. https://doi.org/10.1016/j.carrev.2015.01.002
- 19. Moran, A.E., Forouzanfar, M.H., Roth, G.A., et al. (2014) The Global Burden of Is-chemic Heart Disease in 1990 and 2010 the Global Burden of Disease 2010 Study. Circulation, 129, 1493-1501. https://doi.org/10.1161/CIRCULATIONAHA.113.004046
- 20. Ng, M., Fleming, T., Robinson, M., et al. (2014) Global, Re-gional, and National Prevalence of Overweight and Obesity in Children and Adults during 1980-2013: A Systematic Analysis for the Global Burden of Disease Study 2013. The Lancet, 384, 766-781. https://doi.org/10.1016/S0140-6736(14)60460-8
- 21. Joanne, F., Huo, Y., Ji, L., et al. (2013) Unique and Varied Contributions of Traditional CVD Risk Factors: A Systematic Literature Review of CAD Risk Factors in China. Clinical Medicine Insights: Cardiology, 7, 59-86.
- 22. Hata, J. and Kiyohara, Y. (2013) Epidemiology of Stroke and Coronary Artery Disease in Asia. Circulation Journal Official Journal of the Japanese Circulation Society, 77, 1923-1930. https://doi.org/10.1253/circj.CJ-13-0786
- 23. Park, G.M., Yun, S.C., Cho, Y.R., et al. (2015) Prevalence of Coronary Athero-sclerosis in an Asian Population: Findings from Coronary Computed Tomographic Angiography. The International Journal of Cardi-ovascular Imaging, 31, 659-668. https://doi.org/10.1007/s10554-015-0587-0
- 24. Yang, G., Wang, Y., Zeng, Y., et al. (2013) Rapid Health Transition in China, 1990-2010: Findings from the Global Burden of Disease Study 2010. The Lancet, 381, 1987-2015. https://doi.org/10.1016/S0140-6736(13)61097-1
- 25. Herlitz, J., Haglid, M., Albertsson, P., et al. (2015) Short-and Long-Term Prognosis after Coronary Artery Bypass Grafting in Relation to Smoking Habits. Cardiology, 88, 492-497.
- 26. Lawton, J.S. (2002) Off-Pump Coronary Artery Bypass Grafting. The Lancet, 360, 327-330. https://doi.org/10.1016/S0140-6736(02)09557-0
- 27. Lassen, J.F., Holm, N.R., Banning, A., et al. (2016) Percutaneous Coro-nary Intervention for Coronary Bifurcation Disease: 11th Consensus Document from the European Bifurcation Club. European Society of Cardiology, 12, 38-46. https://doi.org/10.4244/eijv12i1a7
- 28. Conrotto, F., Scacciatella, P., D'Ascenzo, F., et al. (2014) Long-Term Outcomes of Per-cutaneous Coronary Interventions or Coronary Artery Bypass Grafting for Left Main Coronary Artery Disease in Octogenarians (from a Drug- Eluting Stent for Left Main Artery Registry Substudy). American Journal of Cardiology, 113, 2007-2012. https://doi.org/10.1016/j.amjcard.2014.03.044
- 29. Herbison, P. and Wong, C.K. (2015) Has the Difference in Mortality between Percutaneous Coronary Intervention and Coronary Artery Bypass Grafting in People with Heart Disease and Diabetes Changed over the Years? A Systematic Review and Meta-Regression. BMJ Open, 5, Article ID: 010055. https://doi.org/10.1136/bmjopen-2015-010055
NOTES
*通讯作者。
