Asian Case Reports in Pediatrics
Vol.
09
No.
02
(
2021
), Article ID:
48118
,
9
pages
10.12677/ACRP.2021.92002
2例儿童急性淋巴细胞白血病合并肺孢子肺炎并文献复习
陈虹馨,叶富基,吴学东*
南方医科大学南方医院儿科,广东 广州
收稿日期:2021年12月11日;录用日期:2022年1月11日;发布日期:2022年1月21日

摘要
目的:探讨儿童急性淋巴细胞白血病(Acute lymphoblastic leukemia, ALL)合并肺孢子肺炎(Pneumocystis pneumonia, PCP)与艾滋病(Acquired immunodeficiency syndrome, AIDS)合并PCP在临床症状、影像学及治疗方面的不同。方法:回顾性分析我院2015年至今经病原学确诊为PCP的ALL患儿,与从CNKI数据库、万方资源数据库、PubMed数据库、Science Online数据库中以“艾滋病/AIDS”、“肺孢子肺炎/Pneumocystis pneumonia”为关键词检索AIDS合并PCP的相关文献,比较两类患者的临床症状、影像学表现及治疗。结果:我院2例确诊为ALL合并PCP,余疑似病例在经验性用药后均治愈。2例病例起病时均有发热伴干咳、气促,双肺可闻及少量湿啰音,血氧饱和度下降,使用无创辅助通气治疗可维持正常,乳酸脱氢酶(LDH)无明显上升,HRCT均呈斑片状密度增高影,1例出现实变影,另1例出现散在结节状致密影。2例均行纤维支气管镜肺泡灌洗,高通量检查确诊为PCP,予卡泊芬净、TMP-SMZ、糖皮质激素治疗后好转。结论:ALL合并PCP与AIDS合并PCP的临床症状、影像学表现及治疗基本一致,但ALL合并PCP起病时LDH无明显上升,肺部阳性体征较AIDS合并PCP更为常见。
关键词
儿童血液病,急性淋巴细胞白血病,肺孢子肺炎,复方磺胺甲噁唑

Two Cases of Childhood Acute Lymphoblastic Leukemia Combined with Pneumocystis Pneumonia and Literature Review
Hongxin Chen, Fuji Ye, Xuedong Wu*
Department of Pediatrics, Nanfang Hospital, Southern Medical University, Guangzhou Guangdong
Received: Dec. 11th, 2021; accepted: Jan. 11th, 2022; published: Jan. 21st, 2022

ABSTRACT
Objective: The objective is to explore the differences in clinical symptoms, imaging and treatment between childhood acute lymphoblastic leukemia (ALL) combined with Pneumocystis pneumonia (PCP) and AIDS combined with PCP. Methods: A retrospective analysis of childhood ALL diagnosed with PCP in our hospital from 2015 to the present, was compared with literature searched by “艾滋病/AIDS” and “卡氏肺孢子虫肺炎/Pneumocystis pneumonia” as keywords from CNKI database, Wanfang Resource database, PubMed database and Science Online database, to find out the differences in clinical symptoms, imaging manifestations and treatment of the two types of patients. Results: Two patients in our hospital were diagnosed with ALL combined with PCP, and the remaining suspected patients were cured after empirical treatment. Both patients had fever with dry cough and shortness of breath of onset, a few moist rales over lung fields and oxygen saturation decreased. Both could maintain the normal arterial oxygen with the help of non-invasive ventilation. Lactate dehydrogenase (LDH) didn’t increase significantly. Both HRCT showed patchy opacities, one case had consolidation, and the other had scattered nodules. Patients underwent fiberoptic bronchoscopies and bronchoalveolar lavage, high-throughput examination confirmed the diagnosis of PCP, and both improved after the treatment with caspofungin, TMP-SMZ, and glucocorticoids. Conclusion: The clinical symptoms, imaging manifestations and treatment of ALL combined with PCP and AIDS combined with PCP are similar, but LDH does not increase significantly at the onset of ALL combined with PCP, and positive lung signs are more common than AIDS combined with PCP.
Keywords:Childhood Hematology, Acute Lymphocytic Leukemia, Pneumocystis Pneumonia, Trimethoprim-Sulfametho-Xazole

Copyright © 2021 by author(s) and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/


1. 前言
肺孢子肺炎(PCP)是一种间质性浆细胞性肺炎,其病原体肺孢子菌是一种真菌且广泛存在于哺乳动物肺组织内 [1]。临床上PCP常见于使用大量免疫抑制剂、化疗药物及免疫缺陷病的患者中,尤其是艾滋病(AIDS)患者,PCP为该类患者的主要致死病因。目前临床上常用磺胺甲噁唑与甲氧苄啶的复合制剂,即复方磺胺甲噁唑(TMP-SMZ)治疗PCP。在急性淋巴细胞白血病(ALL)患儿化疗过程中,由于化疗药的细胞毒性作用,患儿长期处于骨髓抑制状态,此时亦容易出现肺孢子菌机会性感染。有文献报道,未予TMP-SMZ进行预防治疗的ALL患儿,PCP的患病率可达15%~20% [2],而在合并感染肺炎致死的ALL患儿中,病原体为肺孢子菌的占12%~28% [3]。因此在儿童ALL化疗方案中,均建议常规予TMP-SMZ进行预防。但仍有少数ALL患儿会感染PCP。在此报道2例经过肺泡灌洗液高通量检查后明确为肺孢子菌感染的ALL病例,同时复习相关文献,为该类疾病的临床诊断、相关治疗提供一定的参考。
2. 临床资料
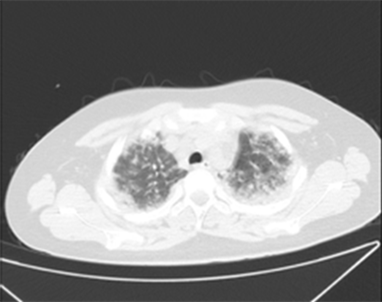
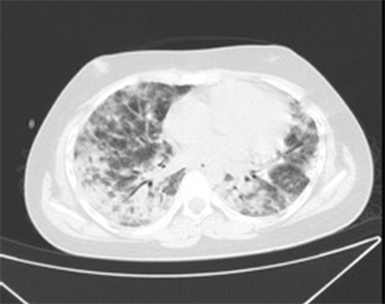
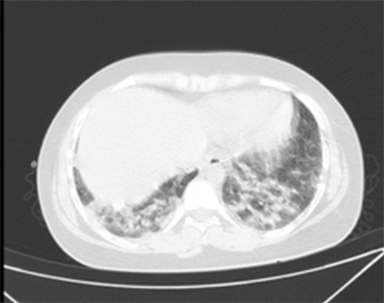
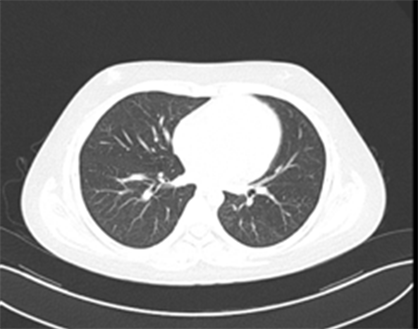
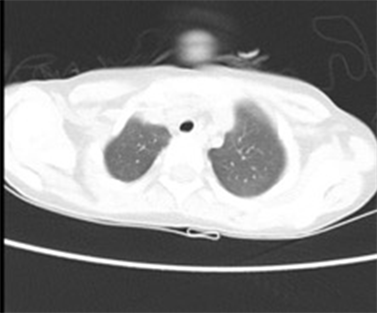
病例1:患儿,男,16岁,2018-11因发热就诊,血常规见两系减少,骨髓穿刺确诊为急性淋巴细胞白血病。2018-11开始予CCCG-ALL-2015方案治疗,治疗期间患儿自行减量服用TMP-SMZ,至2020-02患儿已进入中危晚期维持治疗。2020-05患儿出现发热2天,热峰39℃。胸片(如图1所示):双肺纹理增粗、增多,见散在分布斑片斑点状密度增高影,双下肺病灶部分呈片状高密度,内见“支气管充气征”,病灶以双侧肺门对称分布。胸部CT (如图2所示):双肺透亮度减低,内见弥漫多发斑片状及片状密度增高影,边界模糊,部分实变。住院期间患儿仍间断发热,伴间断单声干咳,呼吸33~64次/分,双肺可闻及散在湿啰音,LDH波动于237~326 U/L,血气分析:PaO2 48 mmHg,PaCO2 35 mmHg,BE 1.8 mmol/L,K+ 3 mmol/L,Na+ 137 mmol/L,LA 1.5 mmol/L,Hct 31%。予高通量辅助通气后血氧饱和度仅维持于92%~95%。经家属同意后进行气管插管术予有创呼吸机辅助通气,同时进行纤维支气管镜检查,肺泡灌洗液送检高通量,确诊为耶氏肺孢子菌、细环病毒感染。予卡泊芬净50 mg/m2 qd、复方磺胺甲噁唑0.96 g q6h、地塞米松5 mg bid抗感染治疗13天后患儿好转,复查胸部CT (如图3所示):1) 原双肺多发炎症较前已基本吸收,现双肺下叶后基底段少许慢性炎症;2) 右肺上叶尖段、前段结节,考虑炎性结节。

Figure 1. The chest radiograph before treatment of case 1
图1. 病例1治疗前胸片
 (a)
(a)
 (b)
(b)
 (c)
(c)
Figure 2. The chest CT before treatment
图2. 治疗前CT图像
 (a)
(a)
 (b)
(b)
 (c)
(c)
Figure 3. The chest CT after 13 days’ treatment
图3. 治疗13天后CT图像
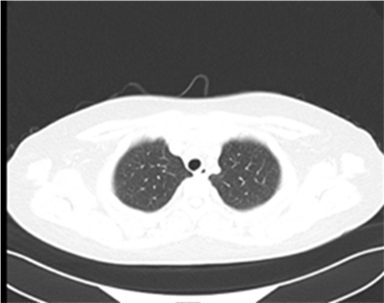
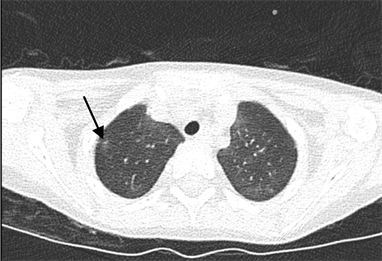
病例2:患儿,男,6岁,2020-06发现左侧颈部一蚕豆大小肿物及全身针尖样出血点,骨髓穿刺确诊为急性淋巴细胞白血病。2020-07开始予CCCG-ALL-2020方案治疗。因患儿存在G-6-PD缺乏症,使用磺胺药存在溶血风险,化疗期间未予TMP-SMZ服用。患儿CAT治疗结束5天后出现发热伴咳嗽,热峰38℃。胸部CT (如图4所示):双肺散在多发结节状、斑片状密度增高影,边缘模糊,以双下肺较明显;右肺下叶外基底段见一小结节状致密影。住院期间患儿出现干咳、气促,三凹征明显,听诊双肺呼吸音粗,右下肺可闻及少许湿性啰音,LDH波动于298~405 U/L,血氧饱和度一过性下降至88%,低流量给氧后呼吸频率仍波动于30~60次/min,后调整为高流量无创通气给氧。经家属同意后进行纤维支气管镜检查,肺泡灌洗液送检高通量,确诊为卡氏肺囊虫感染。予卡泊芬净50 mg/m2 qd、复方磺胺甲噁唑25 mg/kg q6h、甲泼尼龙1 mg/kg抗感染治疗,患儿未出现明显溶血情况。治疗5天后患儿好转,复查胸部CT (如图5所示):原双肺散在多发炎症较前吸收;右肺下叶外基底段小钙化灶。
 (a)
(a) (b)
(b)
Figure 4. The chest CT before treatment (the black arrow indicates nodular shadows of increased density)
图4. 治疗前CT图像(黑色箭头指示结节状密度增高影)
 (a)
(a) (b)
(b)
Figure 5. The chest CT after 8 days’ treatment
图5. 治疗8天后CT图像
3. 讨论及相关文献复习
PCP是由肺孢子虫引起的一种间质性肺炎,由于肺孢子虫在肺组织内扩散,致肺内细胞广泛受损、肺泡毛细血管通透性增加、乳酸脱氢酶(LDH)显著升高,而形成间质性浆细胞性肺炎。肺孢子虫在正常人群中为隐匿性感染,而在艾滋病患者中,尤其是当CD4+T淋巴细胞计数 < 50/uL时,PCP为最常见的机会性感染 [4]。同时PCP也是艾滋病患者最主要的死亡病因 [5],当肺孢子虫在肺泡内大量繁殖,引起肺毛细血管阻滞并降低肺泡表面活性物质含量时,患者最终出现呼吸衰竭而致死亡。艾滋病合并PCP以发热、进行性呼吸困难、干咳、发绀为主要临床表现,伴LDH升高,肺部阳性体征少,胸部X线多呈双肺弥漫性病变、弥漫性毛玻璃样改变 [6] [7] [8] [9]。胸部CT相较胸片更敏感,在AIDS合并PCP的胸部CT特点的相关文献分析中,肺部病变以中央部或肺门对称性分布常见,多为肺纹理增粗的间质性肺炎改变,少数可有肺部实变影、结节状影 [10],根据CT的表现还可将PCP细分为膜玻璃型、间质型(网织结节型)、肺气囊型和斑片–大片型这几种类型 [11]。确诊PCP的金标准以肺泡灌洗液、诱导痰、肺组织活检染色检出病原体为准,但总体检出率低,目前主要依靠临床诊断为主。对于诊断明确的AIDS患者,若CD4+T淋巴细胞计数 < 200/uL,可予TMP-SMZ预防性用药;合并PCP的患者,应该及早使用TMP-SMZ (100 mg/kg/d,分四次口服)对其进行治疗,并辅以吸氧、糖皮质激素等对症治疗 [7]。
在本文2例ALL合并PCP的病例中,患儿起病时均是呈发热伴干咳、气促,双肺可闻及少量湿啰音,血氧饱和度均出现下降,后使用高通量给氧维持正常氧分压。两例病例中,胸部CT都呈斑片状密度增高影,其中由于病例1的肺部炎症更为严重,CT呈实变影,治疗时间也较病例2长;而病例2则出现散在结节状致密影;这些均与PCP的发病表现基本一致。而两例病例中LDH均未出现明显上升,考虑到两例病例均存在ALL基础疾病及化疗相关副作用,且病例数较少,因此LDH是否能作为判断ALL病人合并PCP发生的指标需进一步研究。查阅文献发现,血清(1,3)-β-D葡聚糖(BDG)是一种存在于大多数真菌(包括念珠菌属、曲霉菌属、卡氏肺孢子菌)细胞壁的多糖成分,可作为敏感度较高的阴性排除指标 [12] [13],因此临床上还可考虑将BDG纳入以排查PCP感染。Taylor Eddens等人报道了1例儿童21-三体综合征合并ALL的患儿,在全程口服TMP-SMZ预防的情况下,依然感染了严重的PCP,且分子诊断并未发现有关TMP-SMZ的耐药突变 [14]。该病例说明在免疫力低下且需要呼吸支持治疗的患者中,需要考虑到肺孢子感染的可能。本文两例病例均及时进行支气管镜检,送检肺泡灌洗液高通量后确诊为PCP,予卡泊芬净、TMP-SMZ、糖皮质激素治疗后迅速出现好转,因此临床上怀疑ALL患者合并PCP感染时,应及早行病原学检查,同时调整药物,可达到预期治疗效果。另有研究证实,即使在ALL化疗的维持期停止用TMP-SMZ预防性治疗,患儿感染PCP的风险仍会增加,高危组甚至可有70%的感染风险 [15]。同时有研究发现TMP-SMZ不仅可有效预防PCP,还可能具有抗白血病作用 [16]。因此推荐,对所有ALL患儿,在整个化疗阶段至化疗结束后6周至6个月,都需要预防性口服TMP-SMZ,以减少PCP的感染风险 [17] [18]。对TMP-SMZ不耐受、TMP-SMZ导致骨髓抑制及其他副反应的患者,如本文的病例2,化疗初期可尝试予小剂量TMP-SMZ预防性治疗,同时监测患儿尿常规、肝功等指标,待患儿耐受后再逐渐加量,还可考虑选择喷他脒、氨苯砜和阿托伐醌静脉注射和雾化 [19] [20] [21] [22],以减少化疗过程中PCP的感染风险。对于TMP-SMZ的预防剂量,世卫组织及我国艾滋病诊疗指南上均建议AIDS病人每天服用进行预防(TMP 0.16 g和SMZ 0.8 g,bid)。而对于儿童ALL患者,国外推荐每日或每周3 d服用预防剂量(TMP/SMZ 150/750 mg/m2/d) [18]。国外学者研究发现每周2d服用预防剂量,与每日或每周3 d服用预防剂量相比,可达到同样的预防PCP感染效果 [23]。甚至有研究发现,每周1 d服用大剂量的TMP-SMZ (TMP/SMZ 300/2500 mg/m2/d)和每周2/3 d服用TMP-SMZ一样有效 [24]。我国相关指南建议儿童ALL每周连续3 d口服预防剂量(24 mg/kg/d,分2次)。有研究发现,外周血淋巴细胞 < 1.2*109/L时,予每周3 d口服TMP-SMZ (25 mg/kg/d,分2次)预防,直至淋巴细胞上升至 > 1.2*109/L后1周停用,与每周3 d服用预防剂量具有同等的预防治疗效果,且患儿依从性更强 [25]。因此对于服药依从性较差的ALL患儿,也可考虑以外周血淋巴细胞计数作为预防性治疗指征。
致谢
该病例报道已获得患方的知情同意,感谢患方提供的宝贵临床资料。
文章引用
陈虹馨,叶富基,吴学东. 2例儿童急性淋巴细胞白血病合并肺孢子肺炎并文献复习
Two Cases of Childhood Acute Lymphoblastic Leukemia Combined with Pneumocystis Pneumonia and Literature Review[J]. 亚洲儿科病例研究, 2021, 09(02): 9-17. https://doi.org/10.12677/ACRP.2021.92002
参考文献
- 1. Edman, J.C., Kovacs, J.A., Masur, H., et al. (1988) Ribosomal RNA Sequence Shows Pneumocystis carinii to Be a Member of the Fungi. Nature, 334, 519-522. https://doi.org/10.1038/334519a0
- 2. Shankar, S.M. and Nania, J.J. (2007) Management of Pneumocystis jiroveci Pneumonia in Children Receiving Chemotherapy. Pediatric Drugs, 9, 301-309. https://doi.org/10.2165/00148581-200709050-00003
- 3. 林媛媛, 梁昌达, 范晓菊, 等. 小儿白血病化疗后并发卡氏肺囊虫肺炎3例[J]. 江西医药, 2013, 48(8): 724-726.
- 4. Phair, J., Muñoz, A., Detels, R., et al. (1990) The Risk of Pneumocystis carinii Pneumonia among Men Infected with Human Immunodeficiency Virus Type 1. Multicenter AIDS Cohort Study Group. New England Journal of Medicine, 322, 161-165. https://doi.org/10.1056/NEJM199001183220304
- 5. Markowitz, G.S., Concepcion, L., Factor, S.M., et al. (1996) Autopsy Patterns of Disease among Subgroups of an Inner-City Bronx AIDS Population. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology, 13, 48-54. https://doi.org/10.1097/00042560-199609000-00008
- 6. 郭秀莲. 128例艾滋病合并卡氏肺孢子虫肺炎的临床特点[J]. 大家健康(学术版), 2016, 10(9): 186.
- 7. 姚正钢, 邓秋月. 58例艾滋病合并卡氏肺孢子虫肺炎的临床特点[J]. 临床肺科杂志, 2012, 17(9): 1692-1693.
- 8. 彭平, 唐小平, 胡中伟, 等. 艾滋病合并卡氏肺孢子虫肺炎107例[J]. 实用医学杂志, 2011, 27(4): 637-639.
- 9. Delorenzo, L.J., Huang, C.T., Maguire, G.P., et al. (1987) Roentgenographic Patterns of Pneumocystis carinii Pneumonia in 104 Patients with AIDS. Chest, 91, 323-327. https://doi.org/10.1378/chest.91.3.323
- 10. 岳炫彤, 邬颖华, 王涛, 等. 艾滋病合并卡氏肺孢子虫肺炎与其合并肺结核的CT诊断[J]. 中国临床医学影像杂志, 2018, 29(10): 696-698+703.
- 11. 史恒瑞, 赵建民, 江铭. 艾滋病合并卡氏肺孢子虫肺炎分型影像学特点及鉴别诊断[J]. 临床医学, 2013, 33(9): 62-64.
- 12. Morjaria, S., Frame, J., Franco-Garcia, A., et al. (2018) Clinical Performance of (1,3) Beta-D Glucan for the Diagnosis of Pneumocystis Pneumonia (PCP) in Cancer Patients Tested With PCP Polymerase Chain Reaction. Clinical Infectious Diseases, 69, 1303-1309. https://doi.org/10.1093/cid/ciy1072
- 13. Atalay, M.A., Koc, A.N., Kaynar, L.G., et al. (2014) Useful-ness of (1→3)β-D Glucan in Early Diagnosing Pneumocystis jirovecii Pneumonia: A Case Report. Le Infezioni in Me-dicina, 22, 57-61.
- 14. Eddens, T., Song, E., Ardura, M.I., et al. (2016) A Protracted Course of Pneumocystis Pneumo-nia in the Setting of an Immunosuppressed Child with GMS-Negative Bronchoalveolar Lavage. Medical Mycology Case Reports, 11, 48-52. https://doi.org/10.1016/j.mmcr.2016.04.004
- 15. Poulsen, A., Demeny, A.K., Bang Plum, C., et al. (2001) Pneu-mocystis carinii Pneumonia during Maintenance Treatment of Childhood Acute Lymphoblastic Leukemia. Medical and Pediatric Oncology, 37, 20-23. https://doi.org/10.1002/mpo.1157
- 16. Levinsen, M., Shabaneh, D., Bohnstedt, C., et al. (2012) Pneumocystis ji-roveci Pneumonia Prophylaxis during Maintenance Therapy Influences Methotrexate/6-Mercaptopurine Dosing but Not Event-Free Survival for Childhood Acute Lymphoblastic Leukemia. European Journal of Haematology, 88, 78-86. https://doi.org/10.1111/j.1600-0609.2011.01695.x
- 17. Kim, H.A., Jang, H.M., Kim, Y.K., et al. (2018) Charac-teristic Features of Pneumocystis Pneumonia in Pediatric Acute Lymphoblastic Leukemia. Clinical Pediatric Hematolo-gy-Oncology, 25, 154-161. https://doi.org/10.15264/cpho.2018.25.2.154
- 18. Maertens, J., Cesaro, S., Maschmeyer, G., et al. (2016) ECIL Guidelines for Preventing Pneumocystis jirovecii Pneumonia in Patients with Haematological Malignancies and Stem Cell Transplant Recipients. Journal of Antimicrobial Chemotherapy, 71, 2397-2404. https://doi.org/10.1093/jac/dkw157
- 19. Mantadakis, E. (2020) Pneumocystis jirovecii Pneumonia in Children with Hematological Malignancies: Diagnosis and Approaches to Management. Journal of Fungi, 6, Article No. 331. https://doi.org/10.3390/jof6040331
- 20. Kruizinga, M.D., Bresters, D., Smiers, F.J., et al. (2017) The Use of In-travenous Pentamidine for the Prophylaxis of Pneumocystis Pneumonia in Pediatric Patients. Pediatric Blood & Cancer, 64, e26453. https://doi.org/10.1002/pbc.26453
- 21. Madden, R.M., Pui, C.H., Hughes, W.T., et al. (2007) Prophylaxis of Pneumocystis carinii Pneumonia with Atovaquone in Children with Leukemia. Cancer, 109, 1654-1658. https://doi.org/10.1002/cncr.22562
- 22. Nazir, H.F., Elshinawy, M., Alrawas, A., et al. (2017) Efficacy and Safety of Dapsone versus Trimethoprim/Sulfamethoxazol for Pneumocystis Jiroveci Prophylaxis in Children with Acute Lym-phoblastic Leukemia with a Background of Ethnic Neutropenia. Journal of Pediatric Hematology/Oncology, 39, 203-208. https://doi.org/10.1097/MPH.0000000000000804
- 23. Agrawal, A.K., Chang, P.P. and Feusner, J. (2011) Twice Weekly Pneumocystis jiroveci Pneumonia Prophylaxis with Trimethoprim-Sulfamethoxazole in Pediatric Patients with Acute Lymphoblastic Leukemia. Journal of Pediatric Hematology/Oncology, 33, e1-e4. https://doi.org/10.1097/MPH.0b013e3181fd6fca
- 24. Caselli, D., Petris, M.G., Rondelli, R., et al. (2014) Sin-gle-Day Trimethoprim/Sulfamethoxazole Prophylaxis for Pneumocystis Pneumonia in Children with Cancer. The Journal of Pediatrics, 164, 389-392.E1. https://doi.org/10.1016/j.jpeds.2013.10.021
- 25. 赖长城, 李艳红, 曾宪铭, 等. 儿童急性淋巴细胞白血病合并肺孢子菌肺炎预防治疗[J]. 江西医药, 2018, 53(2): 110-112+115.
NOTES
*通讯作者。