Asian Case Reports in Vascular Medicine
Vol.
07
No.
04
(
2019
), Article ID:
34753
,
7
pages
10.12677/ACRVM.2019.74010
Left Ventricular Noncompaction Cardiomyopathy Combined with Severe Mitral Insufficiency: A Case Report and Literature Review
Long Gui*, Min Lin#, Wenpeng Dong
Department of Cardiac Macrovascular Surgery, the First Affiliated Hospital of Anhui Medical University, Hefei Anhui

Received: Mar. 5th, 2020; accepted: Mar. 19th, 2020; published: Mar. 26th, 2020

ABSTRACT
Objective: To explore the diagnosis and treatment of left ventricular noncompaction cardiomyopathy (LVNC) combined with heart valve disease, and to improve the clinical understanding of this disease. Methods: To summarize the clinical data of 1 case of adult diagnosed with left ventricular noncompaction cardiomyopathy combined with severe mitral insufficiency in our hospital, and literature of domestic and foreign reports were reviewed. Results: The patient was admitted for 6 years with heart palpitate and asthma after activities before in hospital, severe mitral insufficiency with LVNC was diagnosed since the preoperative echocardiography and cardiac MRI were performed, and mitral valve replacement was performed under the general anesthesia and cardiopulmonary bypass, postoperative recovery was good and cardiac function was significantly improved compared with that before hospitalization. Conclusion: LVNC combined with severe heart valve disease is uncommon, and surgery is an effective method to treat LVNC combined with intracardiac malformation, which is beneficial for patients with early recovery of cardiac function.
Keywords:Left Ventricular Noncompaction Cardiomyopathy, Cardiomyopathy, Mitral Valve Insufficiency

左心室心肌致密化不全合并二尖瓣重度 关闭不全1例报道并文献复习
桂龙*,林敏#,董文鹏
安徽医科大学第一附属医院心脏大血管外科,安徽 合肥

收稿日期:2020年3月5日;录用日期:2020年3月19日;发布日期:2020年3月26日

摘 要
目的:探讨左心室心肌致密化不全(LVNC)合并心脏瓣膜疾病的诊断及治疗,提高临床对本病的认识水平。方法:总结我院收治的1例成人左心室心肌致密化不全合并二尖瓣重度关闭不全的临床资料,并结合国内外文献进行回顾复习。结果:患者系活动后心悸气喘6年入院,术前行超声心动图及心脏MRI等检查,诊断为LVNC伴二尖瓣重度关闭不全,并在全麻体外循环下二尖瓣置换术,术后恢复良好,心功能较入院前明显改善。结论:LVNC合并严重心脏瓣膜疾病临床较为少见,外科手术治疗是治疗LVNC合并心内畸形的有效方法,有利患者早期心功能的恢复。
关键词 :左心室心肌致密化不全,心肌病,二尖瓣关闭不全

Copyright © 2019 by author(s) and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/


1. 引言
左心室心肌致密化不全(left ventricular noncompaction cardiomyopathy, LVNC)系原发性遗传性心肌病一种,临床较为少见,又称“海绵状”心肌、“蜂窝状”心肌、左心室小梁过度化。目前其病因尚不明确,患者常出现心力衰竭、心律失常和血栓栓塞等症状 [1],而长期二尖瓣关闭不全使得左心容量负荷增加,增高的舒张末压引起离心性肥厚和左心室扩张,室壁应力增加,严重影响左心室心肌收缩功能,常需外科手术治疗。现将一例LVNC患者合并二尖瓣关闭不全患者的临床资料进行回顾分析,并行相关文献复习。
2. 病历资料
患者,男性,30岁,主诉“活动后心悸、气喘6年”入住安徽医科大学第一附属医院心血管外科,患者6年前开始出现活动后心悸气喘,休息后缓解,后症状反复,逐渐加重,遂至我院门诊,拟“心脏瓣膜病”收住入院,患者无咳嗽咳痰咯血,无胸痛及放射痛,既往无高血压、血栓栓塞、心律失常等疾病,无特殊不良嗜好,无外伤手术史。查体:体温:36.2℃,脉搏:85次/分,呼吸:21次/分,血压:113/75 mm Hg。胸廓对称,双肺呼吸音粗,未闻及明显干湿性啰音,HR:95 bpm,房颤律,心尖区见局限性抬举样搏动,可闻及3/6级收缩期吹风样杂音,双下肢稍水肿。入院后血、尿、粪便常规、生化、凝血、免疫、心肌酶谱、肌钙蛋白未见明显异常,心血管正侧位示:心脏横径增大,以左心室及左心房增大为主,肺血增多。心电图示:心房颤动,完全性右束支传导阻滞,左心室高电压,T波变化。超声心动图示(图1,图2):二尖瓣瓣叶增厚,前叶冗长,关闭时部分脱入左房(相当于A2位置),Doppler测及重度二尖瓣返流,三尖瓣形态活动正常,轻度三尖瓣返流,房间隔中段测及一细束穿隔血流(约0.2 cm),据CWDoppler三尖瓣返流估测右室压力为41 mm Hg,LA:6.13 cm,LVD:8.22 cm,EF:0.51 (Simpson法)。冠状动脉造影未见明显冠脉管腔狭窄。心脏核磁共振(CMR)显示(见图3):左房中度增大,卵圆孔未闭,二尖瓣重度关闭不全,三尖瓣轻度关闭不全,左室重度增大,左室各节段心肌运动弥漫性减弱,左室心尖部前壁、侧壁、下壁,心中部前壁、侧壁、下壁心肌部均匀增厚,增厚心肌处心内膜下肌小梁粗乱呈海绵状,深陷的小梁隐窝与左心室腔相通,心尖部舒张末期内层较厚的非致密化心肌(NC)最厚达21.1 mm,外层薄的致密化心肌(C)最厚达5.2 mm,NC/C = 4.1 > 2.3,心输出量(CO):8.09 L/min,心指数(CI):4.63 L/min/m2,舒张期容积(EDV):293.08 ml,收缩期容积(ESD):174.13 ml,每搏输出量(SV):118.95 ml,舒张末心肌质量(LVMED):279.95 g,射血分数:41%,诊断:1) 心脏瓣膜病:二尖瓣前叶脱垂伴重度关闭不全、三尖瓣轻度关闭不全;2) 卵圆孔未闭;3) 左心室心肌致密化不全;4) 心房颤动;5) 心功能III级(NYHA分级)。术前予以强心、利尿、改善心肌重构、营养支持等对症治疗后,症状有所好转,遂于全麻浅低温体外循环下行二尖瓣机械瓣置换 + 三尖瓣成形 + 卵圆孔未闭缝扎 + 左心耳结扎术。术中经右房–房间隔径路,探查见二尖瓣瓣叶冗长,腱索发育细小,注水试验见大量返流,切除二尖瓣前瓣叶,保留后瓣叶及瓣下结构,并置换29 mm机械瓣,手术顺利,心脏自动复跳,术中心肌阻断84分钟,体外循环时间:122分钟,停机后经食道超声(TEE)见置换瓣膜形态活动正常,未见明显返流,术后早期顺利拔出气管插管脱离呼吸机,出院后回访至今,活动耐量良好,未诉心悸、气喘、胸闷等特殊不适。
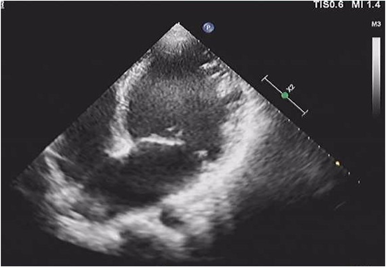
Figure 1. Anterior mitral valve prolapse with incomplete closure in systolic stage
图1. 超声见收缩期二尖瓣前叶脱垂伴关闭不全
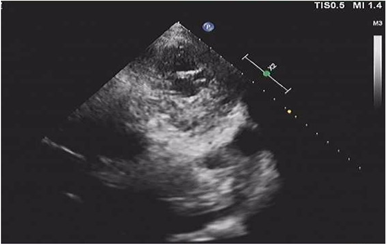
Figure 2. Sonography showed myocardial tissue with different thickness, and the blood flow was interlinked with the cardiac cavity in the deep-set recess
图2. 超声见薄厚不等的心肌组织,深陷的隐窝内有血流与心腔相通

Figure 3. The cardiac MRI showed abnormally increased trabeculae in the cardiac cavity, and the myocardium in the non-dense layer presented a “honeycomb” appearance
图3. 心脏核磁共振见心腔内异常增多的肌小梁,非致密层心肌呈“蜂窝样”
3. 讨论
3.1. 病理生理及遗传学
1926年Grant [2] 首次发现并将其描述为特异的心肌疾病,此后对于LVNC的研究及探索一直持续,多数学者认为在胚胎发育期,其心肌由相互交织的海绵状心肌纤维组成,肌小梁呈网格样,小梁间隙形成隐窝,心腔通过隐窝供给相应区域的心肌血液,此时为非致密心肌,胚胎发育第5周起,心室肌逐渐从外膜到内膜,从基底部到心尖部开始致密化,隐窝被压缩成毛细血管,逐步形成冠状动脉微循环 [3] [4],上述过程中若出现致密化过程受阻,则影响心肌细胞螺旋生长及收缩功能障碍 [5]。
目前LVNC的病因尚不明确,多数学者认为与胚胎发育期间心肌致密化过程暂停有关,但缺乏明确的证据,这一过程的发生可能由遗传性基因变异引起,LVNC遗传通常是X连锁隐性遗传或常染色体显性遗传,而常染色体隐性遗传和线粒体(母体)遗传极为少见 [6] [7],Ichida [8] 等报告,在44%的遗传性LVNC患者中,70%的患者有常染色体显性遗传,30%有X连锁遗传。现有超过40种基因突变及染色体异常与LVNC相关联,如G4.5(TAZ)、LIM域结合蛋白3、LMNA、MYBPC3、TTN [9],此外,一些与先天性心脏病相关的LVNC基因突变也逐渐被发现,如DTNA突变与LNVC合并左心发育不良综合征相关,NKX2-5突变与儿童LVNC合并房间隔缺损相关,MYH7突变与LVNC合并三尖瓣下移畸形(Ebstein畸形)相关等 [10] [11]。
3.2. 临床表现
LVNC的临床表现是高度可变的,可以发生在任何年龄段,从无症状到终末期心力衰竭,其典型的临床三联征为:心力衰竭、心律失常及血栓栓塞。对于有症状的LVNC,心力衰竭是患者就诊的主要原因,本例报道患者系反复活动后心悸、气喘6年,久治不愈前来就诊,其异常的多隆突的肌小梁的血供与心肌供血不相配,虽然冠状动脉正常,但由于心内膜下低灌注,导致左室心肌收缩乏力,和(或)致密化不全累积二尖瓣乳头肌,使得二尖瓣瓣叶发生脱垂造成关闭不全 [12] [13]。在LVNC患者中,室上性心律失常、室性心律失常和慢速性心律失常频繁发生,其中许多是危及生命的,特别是对于严重左心室功能障碍、既往有持续性室性心动过速或纤颤病史、不明原因的复发性晕厥或有心脏猝死家族史的患者更为多见 [14] [15],本例报道的患者术前12导联心电图示:心房颤动、完全性右束支传导阻滞、左心室高电压,追问病史,未发生过恶性心律失常,Weiford [13] 报道在患有LVNC的患者中,出现心电异常的成人高达88%~94%,而儿童约88%。心脏栓塞可表现为卒中、短暂性缺血发作、肠系膜梗死、心肌梗死、肾梗死或周围性栓塞,在严重收缩功能障碍的情况下,血栓可起源于心室腔、小梁间间隙、房颤患者的心房,或通过室间隔缺损或房间隔缺损起源于右心室或右心房,LVNC患者中成人约13%~24%的出现栓塞症状,而儿童约0%~38% [13] [16] [17]。此外,LVNC合并其他心脏畸形或结构性异常可出现如胸痛、紫绀、呼吸困难、生长缓慢等临床症状。
3.3. 诊断及鉴别诊断
经胸或经食道超声心动图仍属于首选的诊断方法和遗传信息筛查方法,它能够特异性显示LVNC心肌结构特点,心脏核磁共振(CRI)以其较高的敏感性(86%)及特异性(99%) [18] 逐步广泛应用。此外,如左心室声学造影技术、增强CT、心室造影等也能为诊断提供依据。
3.3.1. 超声心动图
对于LVNC的超声诊断,目前至少有3种不同的诊断标准,其中Jenni于1990年推荐的孤立性左室心肌致密化不全(即无合并心内畸形,如房间隔缺损、室间隔缺损、肺动脉狭窄、Ebstein畸形、左室发育不良综合征等)超声诊断最为被临床接受并广泛应用,经过不断的完善,其诊断标准如下 [19]:1) 没有合并其他的心脏畸形;2) 典型的双层心肌结构,外层致密化心肌较薄,内层非致密化心肌较厚,由深心内膜间隙的小梁网状结构组成,内层非致密心肌与外层致密化心肌厚度比为>2;3) 主要的异常节段位置(即非致密心肌)见于心尖部(>80%)、下壁和侧壁;4) 彩色多普勒探测深隐窝之间有与心腔相通的血流灌注,而不与冠状动脉循环相通。其对于心内畸形的检查也有着不可替代的作用。
3.3.2. 心脏核磁共振(CRI)
CRI软组织空间分辨力比较高,且能够多方位成像,现阶段CRI诊断LVNC的具体标准至今并未统一。目前引用最多的是Petersen [20] 等提出的诊断标准,他们将7例左心室不致密化患者的磁共振图像与健康对照组以及高血压或肥厚性心肌病等疾病患者的磁共振图像进行了比较,在电影序列上可见异常增多的肌小梁,小梁之间的陷窝与左心室之间相通,并在心肌17节段模型中探索了舒张期非致密心肌与致密心肌的比值(NC/C),发现NC/C > 2.3能够准确区分病理非致密心肌。本例患者心尖部舒张末期内层较厚的非致密化心肌(NC)最厚达21.1 mm,外层薄的致密化心肌(C)最厚达5.2 mm,NC/C = 4.1 > 2.3。
LVNC的临床症状多变,临床鉴别具有一定的困难,主要与扩张性心肌病、肥厚性心肌病、缺血性心肌病等相互鉴别,根据其肌小梁的结构、有无隐窝结构及典型的双层心肌结构、心肌的厚薄、心室壁的活动度等,需要结合病史、临床症状及必要的辅助检查来判断。
3.4. 治疗
LVNC伴有心力衰竭患者的治疗同心力衰竭相同,利尿剂、血管紧张素转化酶抑制剂、血管紧张素受体拮抗剂、适当的β受体阻滞剂等,对于缓解患者急性心衰症状,改善心肌舒缩功能、延缓心室重构有着明显的效果 [21]。Stollberger [22] 等对62名心室致密化不全患者与另外62名非心室致密化不全但症状相似的患者进行对照研究发现,心室致密化不全组体循环栓塞发生率为10%,而对照组为15%,心室致密不全并非栓塞的独立危险因素,但伴有心房颤动、左心扩大、心功能不全等高风险因素,和(或)已有栓塞证据的患者,抗凝治疗显得尤为重要。而对于部分合并严重的心律失常的患者,为避免心源性猝死,除必要的抗心律失常药物治疗外,可植入体内自动除颤器(ICD),但LVNC患者预防性植入指针并未纳入临床治疗指南,需根据临床实际情况综合判断。
LVNC合并心内畸形的患者,手术介入干预对于患者心功能的维护凸显重要,方法包括微创封堵、腔镜手术及传统开胸手术等,本例患者合并有二尖瓣脱垂伴重度关闭不全,其左室扩张明显,其前叶冗长、关闭时脱入左房,相当于A2位置,按经典的Carpentier分型属于IIIB型,我们术前为明确其病因,排除是否因心肌缺血而出现的瓣膜关闭不全,行冠状动脉造影检查,结果阴性,查询相关文献,二尖瓣脱垂伴关闭不全亦常发生于有症状的LVNC患者中,有着一定的病理生理基础,心尖部是LVNC最常累积部位,也是乳头肌的生理附着部位,乳头肌的发育不良导致功能障碍,心肌纤维组织、胶原纤维组织增生明显,纤维组织变粗变长,进而影响二尖瓣瓣叶及腱索的活动 [23],术中注水试验见返流明显,A2处瓣叶脱垂明显,其相应的腱索发育纤细。因该患者青年男性,二尖瓣关闭不全病因不明,且巨大左室伴左心功能减退,二尖瓣显露困难,及家属对于成形效果不佳需再次手术的顾虑,遂行机械瓣膜置换术,术中小心操作,以免过度牵拉导致与乳头肌相连的左室壁出现撕裂损伤,并尽可能保存瓣下结构维持二尖瓣自身形态,国内也报道 [24] 一例风湿性心脏病二尖瓣病变行二尖瓣置换术,术后因左室延迟性破裂 (Ⅲ型)预后不佳,考虑为合并LVNC,但术前未能明确诊断。
总之,LVNC自发现以来逐渐被临床所关注,其并发症及严重性越来越引起重视,对于有症状的LVNC合并瓣膜病变的患者,详细的术前诊疗是必须的,积极的内科治疗及必要的外科手术干预对于其心功能的维持有着重要的意义。
文章引用
桂 龙,林 敏,董文鹏. 左心室心肌致密化不全合并二尖瓣重度关闭不全1例报道并文献复习
Left Ventricular Noncompaction Cardiomyopathy Combined with Severe Mitral Insufficiency: A Case Report and Literature Review[J]. 亚洲心脑血管病例研究, 2019, 07(04): 57-63. https://doi.org/10.12677/ACRVM.2019.74010
参考文献
- 1. Chin, T.K., Perloff, J.K., Williams, R.G., et al. (1990) Isolated Noncompaction of Left Ventricular Myocardium. A Study of Eight Cases. Circulation, 82, 507-513. https://doi.org/10.1161/01.CIR.82.2.507
- 2. Grant, R.T. (1926) An Unusual Anomaly of the Coronary Vessels in the Malformed Heart of a Child. Heart, 13, 273-283.
- 3. Li, S., Yin, L.X., Li, C.M., et al. (2006) Eehoeardiographic Diagnosis of Noncompaction of Ventricular Myocardium and Its Clinical Potential. Chinese Journal of Ultrasound in Medicine, 22, 508-511.
- 4. Henderson, D.J. and Anderson, R.H. (2009) The Development and Structure of the Ventricles in the Human Heart. Pediatric Cardiology, 30, 588-596. https://doi.org/10.1007/s00246-009-9390-9
- 5. Bennett, C.E. and Freudenberger, R. (2016) The Current Approach to Diagnosis and Management of Left Ventricular Noncompaction Cardiomyopathy: Review of the Literature. Cardiology Research and Practice, 2016, Article ID: 5172308. https://doi.org/10.1155/2016/5172308
- 6. Towbin, J.A. (2010) Left Ventricular Noncompaction: A New Form of Heart Failure. Heart Failure Clinics, 6, 453-469. https://doi.org/10.1016/j.hfc.2010.06.005
- 7. Towbin, J.A., Lorts, A. and Jefferies, J.L. (2015) Left Ventricular Non-Compaction Cardiomyopathy. The Lancet, 386, 813-825. https://doi.org/10.1016/S0140-6736(14)61282-4
- 8. Ichida, F., Hamamichi, Y., Miyawaki, T., et al. (1999) Clinical Features of Isolated Noncompaction of the Ventricular Myocardium: Long-Term Clinical Course, Hemodynamic Properties, and Genetic Background. Journal of the American College of Cardiology, 34, 233-240.
- 9. Belanger, A.R., Miller, M.A., Donthireddi, U.R., et al. (2008) New Classification Scheme of Left Ventricular Noncompaction and Correlation with Ventricular Performance. American Journal of Cardiology, 102, 92-96. https://doi.org/10.1016/j.amjcard.2008.02.107
- 10. Ouyang, P., Saarel, E., Bai, Y., et al. (2011) A de Novo Mutation in NKX2.5 Associated with Atrial Septal Defects, Ventricular Noncompaction, Syncope and Sudden Death. Clinica Chimica Acta, 412, 170-175. https://doi.org/10.1016/j.cca.2010.09.035
- 11. Postma, A.V., van Engelen, K., van de Meerakker, J., et al. (2011) Mutations in the Sarcomere Gene MYH7 in Ebstein Anomaly. Circulation: Cardiovascular Genetics, 4, 43-50. https://doi.org/10.1161/CIRCGENETICS.110.957985
- 12. 王超, 杨炳昂, 林凌, 等. 超声心动图对心肌致密化不全的诊断价值[J]. 现代预防医学, 2011, 8(6): 1162-1165.
- 13. Weiford, B.C., Subbarao, V.D. and Mulhern, K.M. (2004) Noncompaction of the Ventricular Myocardium. Circulation, 109, 2965-2971. https://doi.org/10.1161/01.CIR.0000132478.60674.D0
- 14. Chen, H., Zhang, W., Li, D., et al. (2009) Analysis of Ventricular Hypertrabeculation and Noncompaction Using Genetically Engineered Mouse Models. Pediatric Cardiology, 30, 626-634. https://doi.org/10.1007/s00246-009-9406-5
- 15. Stähli, B.E., Gebhard, C., Biaggi, P., et al. (2013) Left Ventricular Non-Compaction: Prevalence in Congenital Heart Disease. International Journal of Cardiology, 167, 2477-2481. https://doi.org/10.1016/j.ijcard.2012.05.095
- 16. Oechslin, E.N., Attenhofer Jost, C.H., Rojas, J.R., et al. (2000) Long-Term Follow-Up of 34 Adults with Isolated Left Ventricular Noncompaction: A Distinct Cardiomyopathy with Poor Prognosis. Journal of the American College of Cardiology, 36, 493-500. https://doi.org/10.1016/S0735-1097(00)00755-5
- 17. Stöllberger, C., Blazek, G., Dobias, C., et al. (2011) Frequency of Stroke and Embolism in Left Ventricular Hypertrabeculation/Noncompaction. American Journal of Cardiology, 108, 1021-1023. https://doi.org/10.1016/j.amjcard.2011.05.039
- 18. Steffen, E.P., Joseph, B.S., Frank, W., et al. (2005) Left Ventricular Non-Compaction Insight from Cardiovascular Magnetic Resonance Imaging. Journal of the American College of Cardiology, 46, 101-105.
- 19. Jenni, R., Echslin, E.N. and van der Loo, B. (2007) Isolated Ventricular Non-Compaction of the Myocardjum in Adults. Heart, 93, 11-15. https://doi.org/10.1136/hrt.2005.082271
- 20. Petersen, S.E., Selvanayagam, J.B., Wiesmann, F., et al. (2005) Left Ventricular Noncompaction: Insights from Cardiovascular Magnetic Resonance Imaging. Journal of the American College of Cardiology, 46, 101-105.
- 21. 李欣洋, 任卫东. 左心室心肌致密化不全研究进展[J]. 中国医学影像技术, 2018, 34(11): 1716-1719.
- 22. Stöllberger, C. and Finsterer, J. (2005) Left Ventricular Hypertrabeculation/Noncompaction and Stroke or Embolism. Cardiology, 103, 68-72. https://doi.org/10.1159/000082050
- 23. 任永凤, 王洲, 丁严, 等. 心肌致密化不全并房室瓣脱垂1例[J]. 中国医学影像技术, 2008(S1): 83.
- 24. 齐胤尊, 马云鹏. 风湿性心脏病并心肌致密化不全行二尖瓣置换术后发生左室破裂死亡临床报告[J]. 临床误诊误治, 2016, 29(6): 59-62.
NOTES
*第一作者。
#通讯作者。