Advances in Clinical Medicine
Vol.
12
No.
10
(
2022
), Article ID:
57144
,
8
pages
10.12677/ACM.2022.12101389
氢气吸入疗法对二甲双胍疗效不佳的2型糖尿病患者的有效性和安全性
林桂花1,倪同上2
1中国人民解放军海军第九七一医院,山东 青岛
2青岛大学医学部中西医结合中心,山东 青岛
收稿日期:2022年9月24日;录用日期:2022年10月17日;发布日期:2022年10月26日

摘要
目的:探索氢气吸入疗法联合二甲双胍对二甲双胍单药控制不佳患者的治疗效果和安全性。方法:将110例2型糖尿病(T2DM)患者随机分为治疗组(n = 55)和对照组(n = 55),治疗组患者服用二甲双胍并且接受氢气吸入疗法,对照组患者使用二甲双胍和安慰剂气体,疗程12周,观察治疗前后两组患者的糖化血红蛋白(HbA1c)、空腹血糖(FPG)、餐后2 h血糖(2hPG)、一日七次的血糖自测、甘油三酯(TG)、总胆固醇(TC)、高密度脂蛋白胆固醇(HDL)、低密度脂蛋白胆固醇(LDL)、胰岛素抵抗指数(HOMA-IR)、胰岛b细胞功能指数(HOMA-b)和体重等指标变化,并且比较两组患者不良反应的发生率。结果:在基线状态下,两组患者的各项指标均无显著差异(P > 0.05),经过12周治疗后,治疗组患者的HbA1c、FPG、2hPG、TG、TC、HDL、LDL、HOMA-IR、HOMA-b和体重均显著得到改善(P < 0.05)。对照组患者FPG、2hPG、TC、HDL、HOMA-IR和体重显著升高,LDL显著降低(P < 0.05)。组间对比显示,接受氢气吸入疗法的患者更为显著地改善了HbA1c、FPG、2hPG、一日七次的血糖自测水平、TG、TC、LDL、HOMA-IR、HOMA-b和体重(全部P < 0.05),同时不良反应发生率也显著低于对照组(3.6% vs 32.7%, P = 0.009)。结论:氢气吸入疗法联合二甲双胍进行长达12周的治疗能够显著降低T2DM患者的血糖水平,改善脂质代谢,促使体重下降,调节胰岛素抵抗并恢复胰岛功能,同时减少治疗期间不良反应的发生频率,提高安全性。
关键词
2型糖尿病,糖化血红蛋白,血糖,二甲双胍,氢气吸入疗法

Efficacy and Safety of Hydrogen Inhalation Therapy in Type 2 Diabetes Mellitus Patients Inadequately Controlled by Metformin Alone
Guihua Lin1, Tongshang Ni2
1Hospital 971 of Chinese People’s Liberation Army Navy, Qingdao Shandong
2Center of Integrated Traditional Chinese and Western Medicine, Department of Medicine, Qingdao University, Qingdao Shandong
Received: Sep. 24th, 2022; accepted: Oct. 17th, 2022; published: Oct. 26th, 2022

ABSTRACT
Objective: To explore the efficacy and safety of hydrogen inhalation therapy combined with metformin in patients with inadequately controlled by metformin alone. Methods: 110 patients with type 2 diabetes mellitus (T2DM) were randomly divided into treatment group (n = 55) and control group (n = 55). The patients in the treatment group received metformin and hydrogen inhalation therapy, and the patients in the control group received metformin and placebo gas for 12 weeks. The changes of glycated hemoglobin (HbA1c), fasting blood glucose (FPG), 2-hour postprandial blood glucose (2hPG), self-monitoring of blood glucose seven times a day, triglyceride (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDL), low-density lipoprotein cholesterol (LDL), insulin resistance index (HOMA-IR), pancreatic islet β cell function index (HOMA-β), body weight and the incidence of adverse events in the two groups were compared. Results: At baseline, there was no significant difference between the two groups in all indicators (P > 0.05). After 12 weeks of treatment, HbA1c, FPG, 2hPG, TG, TC, HDL, LDL, HOMA-IR, HOMA-β and body weight of patients in the treatment group were significantly improved (P < 0.05). FPG, 2hPG, TC, HDL, HOMA-IR and body weight of patients in the control group were significantly increased, while LDL was significantly decreased (P < 0.05). Patients receiving hydrogen inhalation therapy significantly improved HbA1c, FPG, 2hPG, self-monitoring of blood glucose level seven times a day, TG, TC, LDL, HOMA-IR, HOMA-β and body weight (all P < 0.05), and the incidence of adverse reactions was also significantly lower than that of the control group (3.6% vs 32.7%, P = 0.009). Conclusion: Hydrogen inhalation therapy combined with metformin for 12 weeks can significantly reduce the blood glucose level, improve lipid metabolism, promote weight loss, regulate insulin resistance and restore islet function in T2DM patients, reduce the frequency of adverse reactions during treatment, and improve safety.
Keywords:Type 2 Diabetes Mellitus, Glycosylated Hemoglobin, Blood Glucose, Metformin, Hydrogen Inhalation Therapy

Copyright © 2022 by author(s) and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/


1. 引言
T2DM是一种复杂的进行性代谢疾病,对人类健康构成重大威胁,占所有糖尿病病例的91%以上。2015年,据估计有4.15亿成年人患有糖尿病,占全球成人人口的9.1%。中国是拥有全球糖尿病患者数量最多的国家,高达1.09亿 [1]。此外,随着生活方式的现代化和饮食习惯的改变,60%~70%的糖尿病患者也患有肥胖症,70%~80%患有高脂血症 [2] [3]。伴有肥胖和高脂血症的T2DM患者控制血糖水平较困难,心血管事件风险较高,死亡率较高 [4]。
T2DM的治疗旨在平衡抗高血糖的疗效、诱发低血糖的风险、体重增加的风险、耐受性和其他不良反应的关系 [5]。当糖尿病合并肥胖、高脂血症时,T2DM综合管理的算法是必不可少的 [6]。然而,相关研究表明除了有副作用外,合成药物也不能有效地控制某些患者的血糖水平 [7] [8]。此外,对于那些患有多种代谢疾病的患者,全面和有效的治疗方法严重缺乏 [9]。
氢气的抗氧化特性近年来已被逐渐发掘 [10] [11],并被广泛用于治疗缺血/再灌注 [12]、脓毒症 [13] 和急性肺损伤 [14] 等各种疾病。最近,氢气也被证明可以抑制糖尿病及其相关疾病 [15] [16] [17]。氢气吸入疗法作为一种能够有效降低血糖的方法,在中国被广泛应用于T2DM患者。然而目前尚未有探索氢气对T2DM患者治疗效果的相关研究出现,因此本研究旨在研究氢气吸入疗法联合二甲双胍对二甲双胍单药控制不佳患者的治疗效果和安全性。
2. 资料与方法
2.1. 一般资料
本研究选取了中国人民解放军海军第九七一医院内分泌科门诊在2019年1月1日至2021年1月1日初诊的T2DM患者110例,纳入患者均符合中国2型糖尿病防治指南诊断标准 [18]。入选标准:1) 被诊断为T2DM至少一年;2) 就诊时的年龄为18~70岁之间;3) 二甲双胍单药无法控制血糖水平。排除标准:1) 其他类型糖尿病,包括1型糖尿病等;2) 妊娠或最近有怀孕准备;3) 已知对氢气、二甲双胍过敏;4) 患有严重的胃、肠、心脏、肝、胰腺或肾脏疾病;5) 伴有精神疾患可能影响研究结果;6) 同时参与了其他相关研究。本研究中的患者均签署了知情同意书,本研究方案被青岛大学医学部伦理委员会批准。
2.2. 治疗方法
对所有入选的患者进行基础的糖尿病控制措施,包括常规饮食摄入的控制,制定了个体化运动指标并且普及糖尿病相关卫生保健知识。将患者随机分为治疗组(n = 55)和对照组(n = 55)。治疗组服用二甲双胍(中美上海施贵宝制药有限公司,国药准字H20023370),每日两次,一次一片,同时使用制氢机(海之圣有限公司)吸入氢气,以3000 ml/h的速率每日治疗3 h;对照组中的患者以相同的频次剂量服用与治疗组相同的药物,同时使用与治疗组制氢机有相同外形的机器泵入空气作为安慰剂气体,治疗时间亦为3 h/d。
所有的患者均随访12周,观察3个月后相应指标的变化情况。两组患者在基线水平时的年龄、性别、糖尿病病程、血压和肾小球滤过率均无统计学意义。见表1。
2.3. 观察指标
记录患者治疗前后的HbA1c、FPG、2hPG、TG、TC、HDL、LDL和体重,计算了胰岛素抵抗指数[HOMA-IR, HOMA-IR = (FBG × FINS)/22.5]、胰岛β细胞功能指数[HOMA-b, HOMA-β = 20 × FINS/(FBG − 3.5)]。每位患者均进行了一日七次的血糖自测,分别于三餐前后1 h和睡前共七个时间点进行。以上指标均使用日立7600自动生化分析仪进行测定。
同时,记录了患者在治疗的过程中发生的不良反应(如低血糖,胃肠道反应等),并且进行了组间比较。
2.4. 统计学分析
计量资料以均数±标准差表示,使用独立样本t检验比较同一指标的组间差异,配对样本t检验用于比较同一组患者治疗前后的变化。计数资料以例数(百分比)表示,使用卡方检验进行组间比较。所有的统计检验均为双尾检验,并认为P值<0.05具有统计学意义。使用SAS 9.2进行全部的数据分析。
3. 结果
3.1. 两组患者治疗前后血糖的变化
在接受治疗前,对照组和治疗组的HbA1c、FPG和2hPG水平并无显著差异(P > 0.05)。在治疗组中,HbA1c (9.04% ± 0.81% vs 8.26% ± 0.93%)、FPG (9.56 ± 0.74 mmol/L vs 8.66 ± 1.21 mmol/L)和2hPG (17.30 ± 3.66 mmol/L vs 15.40 ± 2.49 mmol/L)均显著降低(全部P < 0.05)。经过12周的治疗后,对照组中的HbA1c水平无显著改变(P > 0.05)但FPG (9.47 ± 0.83 mmol/L vs 9.98 ± 1.31 mmol/L)和2hPG (16.77 ± 2.97 mmol/L vs 17.47 ± 3.89 mmol/L)显著上升(P < 0.05)。组间对比显示,氢气吸入疗法在随访期更显著地降低了患者的HbA1c、FPG和2hPG水平(全部P < 0.001)。见表2。
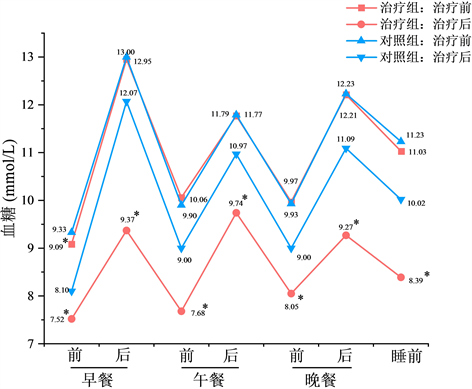
一日七次的血糖自测显示,在治疗前对照组患者的早餐前血糖水平显著高于治疗组(9.33 mmol/L vs 9.09 mmol/L, P < 0.05),两组患者在其他时间点的基线血糖水平均无显著差异(P > 0.05)。经过12周的治疗后,接受氢气吸入疗法患者在七个不同时间点的血糖检测水平均显著低于对照组(全部P < 0.05)。见图1。
3.2. 两组患者治疗前后血脂的改变
基线状态下,两组患者的四种血脂水平均无显著差异(P > 0.05)。经过3个月的治疗后,治疗组患者的TG (2.18 ± 0.55 mmol/L vs 1.99 ± 0.24 mmol/L)、TC (6.13 ± 0.97 mmol/L vs 5.52 ± 0.82 mmol/L)、HDL (1.18 ± 0.39 mmol/L vs 1.22 ± 0.40 mmol/L)、LDL (3.92 ± 0.72 mmol/L vs 3.45 ± 0.48 mmol/L)水平均得到了显著改善(全部P < 0.05)。对照组中,HDL (1.20 ± 0.40 mmol/L vs 1.25 ± 0.38 mmol/L)和LDL (3.99 ± 0.73 mmol/L vs 3.91 ± 0.89 mmol/L)均得到显著改善(全部P < 0.05),TG无显著改变(P > 0.05),而TC (5.93 ± 0.86 mmol/L vs 6.35 ± 0.80 mmol/L, P < 0.05)显著升高。相比于未接受氢气吸入疗法的患者,治疗组患者在12周后的TG、TC和LDL水平显著性的降低(全部P < 0.001),HDL无显著性差异(P > 0.05)。见表3、表4。
3.3. 两组患者治疗前后胰岛功能和体重的不同
治疗前,两组患者的体重、HOMA-β和HOMA-IR水平相似(全部P > 0.05),经过治疗后,氢气吸入疗法显著改善了治疗组患者的体重(85.43 ± 13.52 kg vs 84.13 ± 15.69 kg)、HOMA-β (31.02 ± 7.41 vs 32.39 ± 7.51)和HOMA-IR (3.71 ± 0.84 vs 3.63 ± 0.50) (全部P < 0.05)。在对照组中,患者HOMA-IR (3.61 ± 0.84 vs 3.86 ± 0.62)和体重(86.79 ± 14.27 kg vs 88.21 ± 16.75 kg)均显著升高(全部P < 0.05),HOMA-β无显著改变(P > 0.05)。相比于对照组,治疗组患者的体重、HOMA-β和HOMA-IR水平均有更为显著的改善(全部P < 0.05)。见表5。
3.4. 两组患者在治疗中发生不良反应的比较
治疗组共有2 (3.6%)例患者在治疗过程中出现了不良反应,分别为心悸和胃肠道反应。对照组的不
Table 1. Baseline demographic and clinical characteristics of the patients
表1. 基线状态下患者的人口学特征和临床指标
良反应发生率为32.7%,共出现18例不良反应,其中6 (10.9%)例为心悸,5 (9.1%)例为胃肠道反应,7 (12.7%)例低血糖患者。组间比较显示,接受氢气吸入疗法的患者出现不良反应显著少于对照组(P = 0.009)。见表6。
Table 2. Comparison of blood glucose before and after treatment between both groups
表2. 两组治疗前后血糖比较
注:在同一组中与治疗前比较,*P < 0.05。
Table 3. Comparison of TG and TC before and after treatment between both groups
表3. 两组治疗前后TG和TC的比较
注:在同一组中与治疗前比较,*P < 0.05。
Table 4. Comparison of HDL and LDL before and after treatment between both groups
表4. 两组治疗前后HDL和LDL的比较
注:在同一组中与治疗前比较,*P < 0.05。
Table 5. Comparison of pancreatic islet function and body weight before and after treatment between the two groups
表5. 两组治疗前后胰岛功能和体重的比较
注:在同一组中与治疗前比较,*P < 0.05。
Table 6. Adverse events occurred during the treatment in both groups
表6. 两组患者在治疗过程中出现的不良反应
 注:与对照组比较,*P < 0.05。
注:与对照组比较,*P < 0.05。
Figure 1. Changes in self-monitoring of blood glucose at different time point before and after treatment in both groups
图1. 两组患者治疗前后不同时间点血糖自测的变化
4. 讨论
与对照组相比,氢气吸入疗法能够更为显著地降低患者的HbA1c、FPG、2hPG和一日七次血糖自测水平。Lebaron等 [19] 亦证明,60名代谢综合征患者饮用富氢水24周能够显著改善HbA1c和FPG,而氢分子降低FPG的效果也在多个糖尿病动物模型中被反复证明 [20] [21] [22]。然而,Kajiyama等 [23] 研究结果显示,36名饮用富氢水的T2DM患者未显示出显著的HbA1c改善的效果,这可能与样本量较小有关。
由于T2DM患者常存在高血糖、胰岛素抵抗和高胰岛素血症,这些因素会导致脂质代谢异常 [24] [25]。本研究中,治疗组患者的TG、TC、LDL水平有更为显著的降低,这与先前的多项动物实验结果相符合 [17] [20] [21] [22]。虽然两组患者的HDL均显著升高,二者之间的差异并不显著,多项对代谢综合征患者的氢分子治疗研究在HDL是否有显著改善的问题上同样有着相互矛盾的结果 [19] [26] [27]。
在治疗组中,HOMA-b和HOMA-IR水平在12周的治疗后被显著改善了,这表明氢气疗法能够有效调节T2DM患者的胰岛素抵抗和胰岛细胞功能,这也同样在先前的糖尿病患者和动物模型中被多次证实 [21] [22] [23] [28]。
治疗组在研究过程中的不良反应发生率仅为3.6%,显著低于未吸入氢气的患者。对照组的患者在12周的研究期内有32.7%的患者出现了包括低血糖,胃肠道反应和心悸在内的不良反应,这说明联合氢气吸入疗法治疗T2DM患者能够显著提高安全性。
氢的治疗机制是由于选择性地处理人体内能够破坏细胞成分,导致细胞坏死和凋亡,而没有针对性的解毒途径的OH· [10] [29]。血糖的改善可能是氢分子通过激活磷脂酰肌醇-3-OH激酶、蛋白激酶C和腺苷酸活化蛋白激酶来实现的 [15]。肝脏组织中脂质的异位沉积是胰岛素抵抗的一个不可忽视的原因,氢分子可以抑制这一过程,这可能是胰岛素抵抗改善效应的一个原因 [20] [30]。不可否认的是,氢分子对糖尿病患者的诸多治疗作用背后的分子机制仍然需要进一步的研究。
当然,本研究也有一定的局限性,本研究时间相对较短,同时样本量较小,并且未能探究氢气吸入疗法的最佳治疗时间、次数和浓度等。因此未来的研究应当注重研究大量患者的长期氢气吸入治疗的效果和安全性,探索不同的氢气吸入方案带来的效果差异性。
总之,本研究证明了氢气吸入疗法联合二甲双胍进行长达12周的治疗能够显著降低T2DM患者的血糖水平,改善脂质代谢,促使体重下降,调节胰岛素抵抗并恢复胰岛功能,同时减少治疗期间不良反应的发生频率,提高安全性。
基金项目
本文章来源于青岛大学课题:《氢气对常见慢病的健康影响研究及档案管理》,基金编码:RH2200001592。
文章引用
林桂花,倪同上. 氢气吸入疗法对二甲双胍疗效不佳的2型糖尿病患者的有效性和安全性
Efficacy and Safety of Hydrogen Inhalation Therapy in Type 2 Diabetes Mellitus Patients Inadequately Controlled by Metformin Alone[J]. 临床医学进展, 2022, 12(10): 9605-9612. https://doi.org/10.12677/ACM.2022.12101389
参考文献
- 1. Ogurtsova, K., da Rocha Fernandes, J.D., Huang, Y., et al. (2017) IDF Diabetes Atlas: Global Estimates for the Preva-lence of Diabetes for 2015 and 2040. Diabetes Research and Clinical Practice, 128, 40-50. https://doi.org/10.1016/j.diabres.2017.03.024
- 2. Selvin, E., Parrinello, C.M., Sacks, D.B., et al. (2014) Trends in Prevalence and Control of Diabetes in the United States, 1988-1994 and 1999-2010. Annals of Internal Medicine, 160, 517-525. https://doi.org/10.7326/M13-2411
- 3. Preis, S.R., Pencina, M.J., Hwang, S.-J., et al. (2009) Trends in Cardiovascular Disease Risk Factors in Individuals with and without Diabetes Mellitus in the Framingham Heart Study. Circulation, 120, 212-220. https://doi.org/10.1161/CIRCULATIONAHA.108.846519
- 4. Benjamin, E.J., Blaha, M.J., Chiuve, S.E., et al. (2017) Heart Disease and Stroke Statistics—2017 Update: A Report from the American Heart Association. Circulation, 135, E146-E603. https://doi.org/10.1161/CIR.0000000000000485
- 5. Yu, X.T., Xu, L.P., Zhou, Q., et al. (2018) The Efficacy and Safety of the Chinese Herbal Formula, Jttz, for the Treatment of Type 2 Diabetes with Obesity and Hy-perlipidemia: A Multicenter Randomized, Positive-Controlled, Open-Label Clinical Trial. International Journal of Endo-crinology, 2018, Article ID: 9519231. https://doi.org/10.1155/2018/9519231
- 6. Garber, A.J., Abrahamson, M.J., Barzilay, J.I., et al. (2017) Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm—2017 Executive Summary. Endocrine Practice, 23, 207-238. https://doi.org/10.4158/EP161682.CS
- 7. Ji, L.-N., Lu, J.-M., Guo, X.-H., et al. (2013) Glycemic Control among Patients in China with Type 2 Diabetes Mellitus Receiving Oral Drugs or Injectables. BMC Public Health, 13, Article No. 602. https://doi.org/10.1186/1471-2458-13-602
- 8. Dodd, A.H., Colby, M.S., Boye, K.S., et al. (2009) Treatment Ap-proach and HbA1c Control among US Adults with Type 2 Diabetes: NHANES 1999-2004. Current Medical Research and Opinion, 25, 1605-1613. https://doi.org/10.1185/03007990902973300
- 9. Alberti, K.G.M.M., Zimmet, P. and Shaw, J. (2006) Metabolic Syndrome—A New World-Wide Definition. A Consensus Statement from the International Diabetes Federation. Diabet-ic Medicine, 23, 469-480. https://doi.org/10.1111/j.1464-5491.2006.01858.x
- 10. Ohsawa, I., Ishikawa, M., Takahashi, K., et al. (2007) Hy-drogen Acts as a Therapeutic Antioxidant by Selectively Reducing Cytotoxic Oxygen Radicals. Nature Medicine, 13, 688-694. https://doi.org/10.1038/nm1577
- 11. Wood, K.C. and Gladwin, M.T. (2007) The Hydrogen Highway to Reperfusion Therapy. Nature Medicine, 13, 673-674. https://doi.org/10.1038/nm0607-673
- 12. Buchholz, B.M., Kaczorowski, D.J., Sugimoto, R., et al. (2008) Hydrogen Inhalation Ameliorates Oxidative Stress in Transplantation In-duced Intestinal Graft Injury. American Journal of Transplantation, 8, 2015-2024. https://doi.org/10.1111/j.1600-6143.2008.02359.x
- 13. Xie, K., Yu, Y., Pei, Y., et al. (2010) Protective Effects of Hydrogen Gas on Murine Polymicrobial Sepsis via Reducing Oxidative Stress and Hmgb1 Release. Shock, 34, 90-97. https://doi.org/10.1097/SHK.0b013e3181cdc4ae
- 14. Xie, K., Yu, Y., Huang, Y., et al. (2012) Molecular Hydro-gen Ameliorates Lipopolysaccharide-Induced Acute Lung Injury in Mice through Reducing Inflammation and Apoptosis. Shock, 37, 548-555. https://doi.org/10.1097/SHK.0b013e31824ddc81
- 15. Amitani, H., Asakawa, A., Cheng, K.C., et al. (2013) Hy-drogen Improves Glycemic Control in Type1 Diabetic Animal Model by Promoting Glucose Uptake into Skeletal Muscle. PLOS ONE, 8, e53913. https://doi.org/10.1371/annotation/ea26285b-dda3-470d-a8df-241df9fbc5ad
- 16. Shirahata, S., Hamasaki, T., Ha-ramaki, K., et al. (2011) Anti-Diabetes Effect of Water Containing Hydrogen Molecule and Pt Nanoparticles. BMC Pro-ceedings, 5, Article No. P18. https://doi.org/10.1186/1753-6561-5-S8-P18
- 17. Kamimura, N., Nishimaki, K., Ohsawa, I., et al. (2011) Molecular Hydrogen Improves Obesity and Diabetes by Inducing Hepatic FGF21 and Stimu-lating Energy Metabolism in db/db Mice. Obesity, 19, 1396-1403. https://doi.org/10.1038/oby.2011.6
- 18. 中华医学会糖尿病学分会. 中国2型糖尿病防治指南(2020年版) [J]. 国际内分泌代谢杂志, 2021, 41(5): 482-548.
- 19. Lebaron, T.W., Singh, R.B., Fatima, G., et al. (2020) The Effects of 24-Week, High-Concentration Hydrogen-Rich Water on Body Composition, Blood Lipid Profiles and Inflammation Bi-omarkers in Men and Women with Metabolic Syndrome: A Randomized Controlled Trial. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy, 13, 889-896. https://doi.org/10.2147/DMSO.S240122
- 20. Zheng, M., Yu, H., Xue, Y., et al. (2021) The Protective Effect of Hydrogen-Rich Water on Rats with Type 2 Diabetes Mellitus. Molecular and Cellular Biochemistry, 476, 3089-3097. https://doi.org/10.1007/s11010-021-04145-x
- 21. Ming, Y., Ma, Q.H., Han, X.L., et al. (2020) Molecular Hydrogen Improves Type 2 Diabetes through Inhibiting Oxidative Stress. Experi-mental and Therapeutic Medicine, 20, 359-366. https://doi.org/10.3892/etm.2020.8708
- 22. Wang, Q.J., Zha, X.J., Kang, Z.M., et al. (2012) Therapeutic Effects of Hydrogen Saturated Saline on Rat Diabetic Model and Insulin Resistant Model via Reduction of Oxidative Stress. Chinese Medical Journal, 125, 1633-1637.
- 23. Kajiyama, S., Hasegawa, G., Asano, M., et al. (2008) Supplementation of Hydrogen-Rich Water Improves Lipid and Glucose Metabolism in Patients with Type 2 Diabetes or Impaired Glucose Tolerance. Nutrition Research, 28, 137-143. https://doi.org/10.1016/j.nutres.2008.01.008
- 24. Aslam, M., Aggarwal, S., Sharma, K.K., et al. (2016) Postpran-dial Hypertriglyceridemia Predicts Development of Insulin Resistance Glucose Intolerance and Type 2 Diabetes. PLOS ONE, 11, e0145730. https://doi.org/10.1371/journal.pone.0145730
- 25. Qiu, J., Liu, Y., Yue, Y., et al. (2016) Dietary Tartary Buck-wheat Intake Attenuates Insulin Resistance and Improves Lipid Profiles in Patients with Type 2 Diabetes: A Randomized Controlled Trial. Nutrition Research, 36, 1392-1401. https://doi.org/10.1016/j.nutres.2016.11.007
- 26. Song, G.H., Li, M., Sang, H., et al. (2013) Hydrogen-Rich Water Decreases Serum LDL-Cholesterol Levels and Improves HDL Function in Patients with Potential Metabolic Syndrome. Journal of Lipid Research, 54, 1884-1893. https://doi.org/10.1194/jlr.M036640
- 27. Nakao, A., Toyoda, Y., Sharma, P., et al. (2010) Effectiveness of Hy-drogen Rich Water on Antioxidant Status of Subjects with Potential Metabolic Syndrome—An Open Label Pilot Study. Journal of Clinical Biochemistry and Nutrition, 46, 140-149. https://doi.org/10.3164/jcbn.09-100
- 28. Zhang, X.L., Liu, J.M., Jin, K.K., et al. (2018) Subcutaneous Injection of Hydrogen Gas Is a Novel Effective Treatment for Type 2 Diabetes. Journal of Diabetes Investigation, 9, 83-90. https://doi.org/10.1111/jdi.12674
- 29. Hong, Y., Chen, S. and Zhang, J.M. (2010) Hydrogen as a Selective Antioxidant: A Review of Clinical and Experimental Studies. Journal of International Medical Research, 38, 1893-1903. https://doi.org/10.1177/147323001003800602
- 30. Snel, M., Jonker, J.T., Schoones, J., et al. (2012) Ectopic Fat and Insulin Resistance: Pathophysiology and Effect of Diet and Lifestyle Interventions. International Journal of Endo-crinology, 2012, Article ID: 983814. https://doi.org/10.1155/2012/983814
