Advances in Clinical Medicine
Vol.
12
No.
04
(
2022
), Article ID:
50830
,
11
pages
10.12677/ACM.2022.124491
腹腔镜手术治疗妊娠合并肾上腺源性库欣 综合征1例并文献复习
王琨翔1,孙瑞霞2,陈颖3,杨学成1,彭伟4,纪玉芝4
1青岛大学附属医院泌尿外科,山东 青岛
2青岛大学附属医院内分泌科,山东 青岛
3青岛大学附属医院代谢性疾病科,山东 青岛
4青岛大学附属医院产科,山东 青岛
收稿日期:2022年3月24日;录用日期:2022年4月20日;发布日期:2022年4月27日

摘要
目的:报道一例腹腔镜手术治疗妊娠期合并肾上腺源性库欣综合征,探讨腹腔镜手术治疗妊娠期合并肾上腺源性库欣综合征的可行性与有效性。方法:报道一例病例并回顾分析国内外妊娠合并肾上腺源性库欣综合征的相关文献。共检索到38例在妊娠期进行肾上腺切除术治疗肾上腺腺瘤引起的库欣综合征。结果:库欣综合征对母亲及胎儿的生命造成严重威胁,而妊娠使其诊断与治疗复杂化。孕中期经腹膜后腹腔镜手术是治疗肾上腺源性的库欣综合征的合理有效的方法,可降低胎儿围产期死亡率和母体妊娠相关并发症的发病率,但不能避免胎儿早产和宫内生长受限的发生。结论:妊娠合并库欣综合征诊断治疗相对复杂,应由泌尿外科、内分泌科、妇产科等多学科协同诊治。孕中期腹腔镜下肾上腺腺瘤切除术是治疗妊娠合并肾上腺源性库欣综合征的合理有效的方法。
关键词
妊娠肾上腺腺瘤,库欣综合征,腹腔镜手术

A Case of Laparoscopic Surgery in the Treatment of Pregnancy with Cushing Syndrome Caused by Adrenal Adenoma and Literature Review
Kunxiang Wang1, Ruixia Sun2, Ying Chen3, Xuecheng Yang1, Wei Peng4, Yuzhi Ji4
1Department of Urology, Affiliated Hospital of Qingdao University, Qingdao Shandong
2Department of Endocrinology, Affiliated Hospital of Qingdao University, Qingdao Shandong
3Department of Metabolic Diseases, Affiliated Hospital of Qingdao University, Qingdao Shandong
4Department of Obstetrics, Affiliated Hospital of Qingdao University, Qingdao Shandong
Received: Mar. 24th, 2022; accepted: Apr. 20th, 2022; published: Apr. 27th, 2022

ABSTRACT
Objective: To report a case of laparoscopic surgery in the treatment of Cushing’s syndrome (CS) caused by adrenal adenoma during pregnancy, the feasibility and effectiveness of laparoscopic surgery in the treatment of CS caused by adrenal adenoma during pregnancy were discussed. Methods: We report a case. Then, we review and analyze the domestic and foreign literature on pregnancy complicated with adrenal CS. We retrieved 38 cases of CS caused by adrenal adenoma treated with adrenalectomy during pregnancy. Results: CS poses a serious threat to the lives of mothers and fetuses, and pregnancy complicates the diagnosis and treatment. Laparoscopic adrenal adenoma resection in the second trimester is a reasonable and effective method for the treatment of pregnancy complicated with adrenal CS. It can reduce the fetal perinatal mortality and the incidence of maternal pregnancy-related complications, but it cannot avoid the occurrence of premature fetal delivery and intrauterine growth restriction. Conclusions: The diagnosis and treatment of pregnancy complicated with CS is relatively complicated, and the diagnosis and treatment should be coordinated by a multidisciplinary team, consisting of urologists, obstetricians, endocrinologists. Laparoscopic adrenal adenoma resection in the second trimester is a reasonable and effective method for the treatment of pregnancy complicated with CS caused by adrenal adenoma.
Keywords:Adrenal Adenomas of Pregnancy, Cushing’s Syndrome, Laparoscopic Surgery

Copyright © 2022 by author(s) and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/


1. 引言
库欣综合征(Cushing’s syndrome, CS)是糖皮质激素内源性产生过多导致的疾病,常见病因为垂体腺瘤、肾上腺腺瘤或神经内分泌肿瘤导致皮质醇分泌增多。高皮质醇血症可抑制下丘脑–垂体–卵巢轴,导致大多数女性患者排卵障碍,临床上表现为闭经和不孕,但仍有极少数女性CS妊娠 [1]。妊娠合并CS的母亲更易发生先兆子痫、高血压、糖尿病、机会性感染、骨质疏松等,胎儿流产、早产、死产、宫内发育迟缓的发生也大幅增加。及早诊断及选择合理的治疗方式对减少孕母及胎儿的不良孕产结局至关重要。现报道我院经腹膜后腹腔镜手术治疗妊娠合并肾上腺源性CS 1例,并对已发表的相关文献进行回顾复习。
2. 病例报告
患者,女,24岁,因“皮肤紫纹并体重增加2年余,孕23周”入院,既往无长期糖皮质激素应用史。查体:血压153/92 mmhg,向心性肥胖,脸圆面红,面部可见毳毛,痤疮,发际线低。颈部脂肪垫,双上肢内侧、大腿内外侧及腹部可见数条宽大皮肤紫纹。辅助检查:电解质检测:钾2.71 mmol/L (正常值3.5~5.3 mmol/L);肝肾功、血钙镁磷、粪便常规+潜血、血凝常规、传染性标志物四项未见异常。皮质醇节律测定(8 am~4 pm~0 am):543.00~594.00~553.00 nmol/L (8 am正常值140~507 nmol/L);促肾上腺皮质激素(Adrenocorticotropic Hormone, ACTH)测定(8 am~4 pm~0 am):42.10~2.97~1.89 pg/mL (8 am正常值7.2~63.3 pg/mL)。大剂量地塞米松抑制试验未被抑制。心脏超声示肺动脉高压(轻度),二尖瓣反流(轻微),三尖瓣反流(轻微);肾上腺MR示左侧肾上腺结节,大小约21.9 mm × 25.0 mm (图1)。垂体MR无明显异常。该患者皮质醇增多,昼夜节律异常,大剂量地塞米松抑制试验不受抑制,结合影像学检查及临床症状,诊断为肾上腺腺瘤引起的ACTH非依赖性CS。
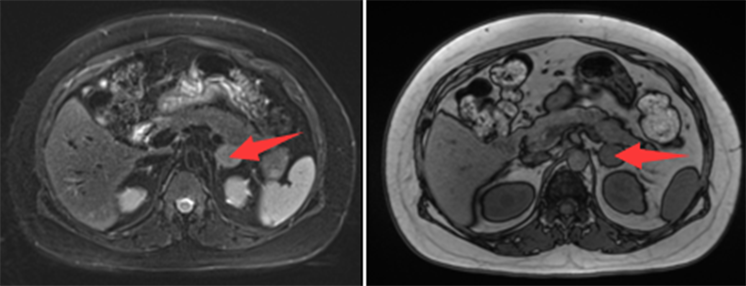
Figure 1. The patient’s preoperative MRI showed left adrenal tumor
图1. 患者术前MRI检查示左肾上腺肿瘤
经多学科讨论后,给以补钾降压,充分术前准备后于孕25+3周时在全麻下腹膜后腹腔镜下左侧肾上腺全部切除术,手术时间60 min,术中出血量约10 ml,术中患者生命体征及胎心平稳。术后病理:肾上腺皮质腺瘤。给予氢化可的松替代治疗预防肾上腺皮质功能减退,同时补钾、补钙。患者术后出现咳血,考虑气管插管损伤粘膜,毛细血管破裂出血所致,术后2周后咳血消失。术后CS体征明显缓解,血压控制良好孕36周时因子痫前期经剖宫产术娩出一女婴,体重2880 g,新生儿Apgar评分1 min及5 min均为10分,新生儿无畸形,无肾上腺皮质功能减低。产后4月后复查肾上腺功能良好,ACTH 127 pg/ml,皮质醇激素84 nmol/L,高血压药物已停用,口服激素术后半年逐渐减停。
3. 文献复习
为评估手术治疗妊娠期合并肾上腺源性CS的疗效与安全性,我们检索了在Pubmed、知网、万方数据上关键词包含库欣综合征/肾上腺皮质腺瘤/高皮质醇血症/怀孕/妊娠的病例报告及其参考文献。排除因肾上腺皮质癌或肾上腺增生(库欣病)而行肾上腺切除,以及分娩后行肾上腺切除的病例。共计检索到38例病例。病例15与16,病例22与30大部分临床特征都相同,且为同一机构报告,被认为代表同一患者,因此将病例15、病例22剔除。加上本例患者,共分析了37例手术治疗妊娠合并肾上腺源性CS的病例,记录患者的年龄、肿瘤的大小和位置、临床表现、肾上腺切除术时的胎龄、手术方式、产妇和新生儿的结局(表1,表2)。
Table 1. Surgical treatment of pregnancy with adrenal Cushing’s syndrome case summary
表1. 手术治疗妊娠合并肾上腺源性库欣综合征的病例汇总
Table 2. Prognosis of the cases shown in Table 1
4. 手术时机及预后
4.1. 手术时机的选择
妊娠的各个时期皆有接受手术治疗的报道,最早为孕4周,最晚为孕32周。其中2例(5.4%)在妊娠早期(孕1~12周)、27例(73%)在妊娠中期(孕13~27周)、8例(21.6%)在妊娠晚期(≥孕28周)进行了手术(见表1)。8例妊娠晚期手术治疗的患者,除病例10是保守治疗后临床症状难以控制方才选择手术治疗外,其余7例明确诊断的时间偏晚。
4.2. 手术方式的选择
21例(56.8%)接受了腹腔镜下肾上腺切除术,16例(43.2%)在孕期行开放手术治疗。两组手术时平均胎龄为22.47 ± 5.71周和21.43 ± 6.84周,手术方式的选择可能与所处的年代有关,2000年出现第一例腹腔镜手术治疗妊娠合并肾上腺肿瘤的患者,之后仅报道了2例开放手术,且均在2004年以前。
4.3. 产妇结局
37例中有27例报道了肾上腺切除术对患者临床症状的影响(表2),其中26例(96%)库欣综合征相关症状缓解,术前合并的高血压、高血糖更容易控制达标;另外1例患者术后第7周发生了重度先兆子痫和HELLP综合征(溶血、肝酶升高和血小板减少为特点,是妊娠期高血压疾病的严重并发症)。
4.4. 妊娠结局
37例报道中,有1例(2.7%)患者在术后第3周,即孕21周发生了自然流产,该患者术前患有严重的心力衰竭,尚不清楚这一结果是否与手术有关。1例(2.7%)患者在孕28周,术后第10周发生了自然流产。其余35例(94.6%)患者皆为活产,平均孕周为35.54 ± 2.79周。21例(60%)分娩发生在孕37周之前,其中9例(25.7%)因胎儿或者母体因素导致早产;10例(27%)在孕34周之前进行了分娩;14例(40%)患者足月分娩(≥37周)。其中14例(40%)患者接受了剖宫产手术,21例(60%)患者为经阴道分娩。28例报道了新生儿的体重,其中有15例(53.6%)低出生体重儿(低于2500 g),有13例(46.4)为早产儿;2例(7.1%)极低出生体重儿(低于1500 g),其余11例(39.3)新生儿出生体重正常。22例早产儿中有6例(27.2%)发生了早产后遗症,但并不严重(见表2)。
4.5. 手术并发症
37例报道中,仅有1例(2.7%)发生了术中并发症,即在开放手术中不慎造成脾脏裂伤。术后并发症包括1例肺水肿,1例尿路感染,1例术后咳血以及1例术后12小时胎心异常。患者术后多需要长期的类固醇激素替代治疗,有30例报道进行了激素替代治疗,其中18例报道了激素替代的治疗时间,8例替代治疗超过6个月,而6例超过了1年。
5. 讨论
库欣综合征(CS)是内源性糖皮质激素过度产生导致的临床综合征,包括垂体或垂体外分泌ACTH的肿瘤、肾上腺皮质肿瘤或结节、增生 [37] [38]。妊娠合并CS罕见,70%~85%的患者排卵障碍,月经紊乱或闭经,难以妊娠。妊娠合并CS增加孕妇和胎儿不良事件发生的风险 [39],如高血压、子痫、糖尿病、骨质疏松或骨折、心衰、精神障碍、感染、流产、早产、胎儿发育缓慢、围产期死亡等。因此早期诊断CS并采取积极合理的治疗措施具有重要的临床意义。
妊娠时胎盘产生促肾上腺皮质激素释放激素(CRH)、ACTH,下丘脑–垂体–肾上腺轴被激活,皮质醇分泌增加,妊娠时皮质类固醇结合球蛋白(CBG)增加,导致孕期血清ACTH、总皮质醇和24小时尿游离皮质醇(UFC)浓度均升高,在妊娠末期达到非妊娠期的2~3倍 [40]。妊娠期机体对外源性糖皮质激素的反应减弱,可不被大剂量地塞米松抑制。妊娠期经典体征与CS的临床表现有较多重叠,比如疲劳、体重增加、多毛、痤疮、情绪不稳、高血压、高血糖可等,给CS的诊断带来困难。
妊娠期CS以肾上腺源性更多见,因此对所有ACTH较低的患者均应行肾上腺的影像学检查。超声是妊娠CS初诊时首选的筛查方式,有研究显示73%的肾上腺源性妊娠期CS患者通过超声发现了肾上腺病变,影像学检查首选肾上腺磁共振检查 [41]。为排除垂体性病变,ACTH高的患者应行垂体MRI检查。影像学检查时还应考虑垂体或肾上腺在妊娠期生理性增大。
妊娠合并CS的患者若明确肾上腺腺瘤,多推荐在妊娠中期行手术治疗,研究证实手术治疗与药物保守治疗相比可以降低围产期死亡率和并发症发病率 [41] [42]。Lo和Lau [14] 的研究比较了12名妊娠期接受肾上腺切除术的患者与25名接受药物治疗的患者的结局,结果显示,妊娠期接受手术治疗的患者围产期结局有所改善。有研究对妊娠晚期的妇女行腹腔镜手术切除患侧肾上腺并使其受益 [18] [27] [39];但也有研究认为妊娠晚期患者应用药物控制,并于产后进行手术切除肾上腺肿瘤可能更加安全 [43] [44] [45]。我们的研究发现在妊娠中期进行肾上腺切除术似乎是安全的,孕妇及胎儿结局良好,因此我们建议肾上腺库欣综合征患者立即手术治疗。
随着腹腔镜技术的发展及经验积累,近年来妊娠期肾上腺切除术的手术方式多选择腹腔镜(见表1),腹腔镜手术母胎不良事件发生率较开放手术更低。但是妊娠患者进行腔镜手术时,增大的子宫导致视野受阻、器械操作空间有限容易损伤子宫与其内容物,另外气腹时腹内压升高会降低胎盘血流量,吸入二氧化碳会导致胎儿酸中毒,增加胎儿出生时并发症的发生几率,因此,我们认为,当肾上腺皮质腺瘤被怀疑是库欣综合征的潜在原因时,腹腔镜手术应该是首选治疗方法,术中需注意将气腹维持在12 mmHg以下,避免手术期间器械与子宫肌肉直接接触等 [21] [26]。
肾上腺腺瘤自主分泌皮质醇,导致腺瘤侧及对侧肾上腺正常组织萎缩,垂体ACTH分泌功能受抑制,腺瘤切除后,下丘脑–垂体–肾上腺轴功能短时间内不能恢复,导致肾上腺皮质功能不全,术后大多需要糖皮质激素替代治疗。替代治疗的剂量一般为孕早期和中期给非妊娠时一样的生理替代量,孕晚期剂量略增加,分娩时剂量需要大幅增加。替代治疗的时间与CS的病程及被抑制的程度有关,直到正常肾上腺完全恢复。本例患者术后接受了6个月的替代治疗,其他病例也大多接受时间不等的替代治疗(见表2)。
妊娠期接受肾上腺切除术的患者能获得更好的母体和胎儿结局 [46],我们分析的37例患者中只有2例发生宫内胎儿死亡(5.4%),而未经治疗的患者的围产期死亡率为18%~30% [9] [20],所有库欣综合征患者的围产期死亡率为15%~21% [47] [48]。Lindsay [41] 等人证明,怀孕期间接受干预治疗,活产率从76%增加到89%。我们的分析显示,手术后产科并发症的发生率高于预期。关于妊娠合并库欣综合征治疗在改善结局方面的有效性的数据并不一致,早产和先兆子痫的发生也无法通过治疗加以预防 [41],早产(60%)和宫内生长受限(53.6%)的发生率与妊娠期未经治疗的库欣综合征患者无显著差异 [1] [47] [48] [49]。这些结果强调,妊娠合并库欣综合征患者即使经过手术治疗,也需要进行密切的产前随访。
本研究有一定的局限性。首先,现有数据表明存在发表偏倚。其次,我们收集了自1952年以来的病例,纳入的患者来自一个广泛的历史时期,当时的治疗和诊断与近期存在明显差异。此外,由于患者来自不同的中心,并有自己的标准,因此定义母体和胎儿并发症的标准可能有所不同。由于没有来自单一中心的大系列CS和妊娠,我们认为该文献回顾有助于了解这种罕见但具有挑战性的临床情况下的预后因素。
6. 结论
妊娠合并CS病情复杂,应由泌尿外科、内分泌科、妇产科等多学科协同诊治。已有的37例手术治疗妊娠合并肾上腺源性CS的患者表明,孕中期腹腔镜下手术切除腺瘤是安全和有效的方法,手术时机和方式应由有经验的外科医师根据病情的严重程度、患者的个人意愿和胎龄来确定。但目前病例数目较少,无法提供循证学依据。
文章引用
王琨翔,孙瑞霞,陈 颖,杨学成,彭 伟,纪玉芝. 腹腔镜手术治疗妊娠合并肾上腺源性库欣综合征1例并文献复习
A Case of Laparoscopic Surgery in the Treatment of Pregnancy with Cushing Syndrome Caused by Adrenal Adenoma and Literature Review[J]. 临床医学进展, 2022, 12(04): 3393-3403. https://doi.org/10.12677/ACM.2022.124491
参考文献
- 1. Kyriakos, G., Farmaki, P., Voutyritsa, E., et al. (2021) Cushing’s Syndrome in Pregnancy: A Review of Reported Cases. Endokrynologia Polska, 72, 64-72. https://doi.org/10.5603/EP.a2020.0089
- 2. Eisenstein, A.B., Karsh, R. and Gall, I. (1963) Occurrence of Pregnancy in Cushing’s Syndrome. The Journal of Clinical Endocrinology & Metabolism, 23, 971-974. https://doi.org/10.1210/jcem-23-10-971
- 3. Grimes, E.M., Fayez, J.A. and Miller, G.L. (1973) Cushing’s Syndrome and Pregnancy. Obstetrics & Gynecology, 42, 550-559. https://doi.org/10.1097/00006250-197310000-00012
- 4. Blumsohn, D., Munyadziwa, E.H., Dajie, S.K., Sher, R.C. and Prajapat, D.K. (1978) Cushing’s Syndrome and Pregnancy: A Case Report. South African Medical Journal, 53, 338-340.
- 5. Abrahamson, M.J., Miller, J.L., Alperstein, A.L. and Barron, J.L. (1986) Cushing’s Syndrome in Pregnancy. A Case Report. South African Medical Journal, 69, 834-835.
- 6. Bevan, J.S., Gough, M.H., Gillmer, M.D. and Burke, C.W. (1987) Cushing’s Syndrome in Pregnancy: The Timing of Definitive Treatment. Clinical Endocrinology (Oxf), 27, 225-233. https://doi.org/10.1111/j.1365-2265.1987.tb01148.x
- 7. Barasch, E., Sztern, M., Spinrad, S., et al. (1988) Pregnancy and Cushing’s Syndrome: Example of Endocrine Interaction. Israel Journal of Medical Sciences, 24, 101-104.
- 8. Cook, D.J., Riddell, R.H. and Booth, J.D. (1989) Cushing’s Syndrome in Pregnancy. CMAJ, 141, 1059-1061.
- 9. Pricolo, V.E., Monchik, J.M., Prinz, R.A., DeJong, S., Chadwick, D.A. and Lamberton, R.P. (1990) Management of Cushing’s Syndrome Secondary to Adrenal Adenoma during Pregnancy. Surgery, 108, 1072-1077.
- 10. Pickard, J., Jochen, A.L., Sadur, C.N. and Hofeldt, F.D. (1990) Cushing’s Syndrome in Pregnancy. Obstetrical & Gynecological Survey, 45, 87-93. https://doi.org/10.1097/00006254-199002000-00002
- 11. Motta, L., Barbosa, A.M., Ferreira, M.A. and Gagliardi, A.R. (1991) Two Pregnancies in a Cushing’s Syndrome. Case Report. Panminerva Medica, 33, 44.
- 12. MacGibbon, A.L. and Brieger, G.M. (1995) Cushing Syndrome in Pregnancy Secondary to an Adrenal Cortical Adenoma. The Australian and New Zealand Journal of Obstetrics and Gynaecology, 35, 217-219. https://doi.org/10.1111/j.1479-828X.1995.tb01878.x
- 13. Kamiya, Y., Okada, M., Yoneyama, A., et al. (1998) Surgical Successful Treatment of Cushing’s Syndrome in a Pregnant Patient Complicated with Severe Cardiac Involvement. Endocrine Journal, 45, 499-504. https://doi.org/10.1507/endocrj.45.499
- 14. Lo, K.W. and Lau, T.K. (1998) Cushing’s Syndrome in Pregnancy Secondary to Adrenal Adenoma. A Case Report and Literature Review. Gynecologic and Obstetric Investigation, 45, 209-212. https://doi.org/10.1159/000009958
- 15. Nakashima, Y.M., Itonaga, Y., Inoue, H. and Takahashi, S. (2000) Pulmonary Edema after laparoscopic Adrenalectomy in a Pregnant Patient with Cushing’s Syndrome. Journal of Anesthesia, 14, 157-159. https://doi.org/10.1007/s005400070026
- 16. Aishima, M., Tanaka, M., Haraoka, M. and Naito, S. (2000) Retroperitoneal Laparoscopic Adrenalectomy in a Pregnant Woman with Cushing’s Syndrome. The Journal of Urology, 164, 770-771. https://doi.org/10.1016/S0022-5347(05)67300-4
- 17. Lo, C.Y., Lo, C.M. and Lam, K.Y. (2002) Cushing’s Syndrome Secondary to Adrenal Adenoma during Pregnancy. Surgical Endoscopy, 16, 219-220. https://doi.org/10.1007/s00464-001-4105-1
- 18. Shaw, J.A., Pearson, D.W., Krukowski, Z.H., Fisher, P.M. and Bevan, J.S. (2002) Cushing’s Syndrome during Pregnancy: Curative Adrenalectomy at 31 Weeks Gestation. European Journal of Obstetrics & Gynecology and Reproductive Biology, 105, 189-191. https://doi.org/10.1016/S0301-2115(02)00148-3
- 19. Doshi, S., Bhat, A. and Lim, K.B. (2003) Cushing’s Syndrome in Pregnancy. Journal of Obstetrics and Gynaecology, 23, 568-569. https://doi.org/10.1080/0144361031000156582
- 20. Blanco, C., Maqueda, E., Rubio, J.A. and Rodriguez, A. (2006) Cushing’s Syndrome during Pregnancy Secondary to Adrenal Adenoma: Metyrapone Treatment and Laparoscopic Adrenalectomy. Journal of Endocrinological Investigation, 29, 164-167. https://doi.org/10.1007/BF03344091
- 21. Klibanski, A., Stephen, A.E., Greene, M.F., Blake, M.A. and Wu, C.L. (2006) Case Records of the Massachusetts General Hospital. Case 36-2006. A 35-Year-Old Pregnant Woman with new Hypertension. The New England Journal of Medicine, 355, 2237-2245. https://doi.org/10.1056/NEJMcpc069027
- 22. 陈蔚琳, 边旭明, 刘俊涛, 杨剑秋. 继发于肾上腺腺瘤的库欣综合征孕期诊治[J]. 中华围产医学杂志, 2009, 12(5): 378-379.
- 23. Terhune, K.P., Jagasia, S., Blevins, L.S. and Phay, J.E. (2009) Diagnostic and Therapeutic Dilemmas of Hypercortisolemia during Pregnancy: A Case Report. The American Surgeon, 75, 232-234. https://doi.org/10.1177/000313480907500309
- 24. Rask, E., Schvarcz, E., Hellman, P., Hennings, J., Karlsson, F.A. and Rao, C.V. (2009) Adrenocorticotropin-Independent Cushing’s Syndrome in Pregnancy Related to Overexpression of Adrenal Luteinizing Hormone/Human Chorionic Gonadotropin Receptors. Journal of Endocrinological Investigation, 32, 313-316. https://doi.org/10.1007/BF03345718
- 25. Pollack, R.P. and Brett, E.M. (2010) Adrenocorticotropic Hormone-Independent Cushing Syndrome Manifesting during Pregnancy. Endocrine Practice, 16, 260-263. https://doi.org/10.4158/EP09232.CR
- 26. Toutounchi,, S., Makowska, A., Krajewska, E., et al. (2011) Laparoscopic Treatment of Cushing’s Syndrome in a Woman in Late Pregnancy—A Case Presentation. Wideochirurgia I Inne Techniki Maloinwazyjne, 6, 261-263. https://doi.org/10.5114/wiitm.2011.26263
- 27. Sammour, R.N., Saiegh, L., Matter, I., et al. (2012) Adrenalectomy for Adrenocortical Adenoma Causing Cushing’s Syndrome in Pregnancy: A Case Report and Review of Literature. European Journal of Obstetrics & Gynecology and Reproductive Biology, 165, 1-7. https://doi.org/10.1016/j.ejogrb.2012.05.030
- 28. Diri, H., Bayram, F., Simsek, Y., et al. (2014) A Pregnant Woman Who Underwent Laparoscopic Adrenalectomy Due to Cushing’s Syndrome. Case Reports in Endocrinology, 2014, Article ID: 283458. https://doi.org/10.1155/2014/283458
- 29. Martínez García, R., Martínez Pérez, A., Domingo del Pozo, C. and Sospedra Ferrer, R. (2016) Cushing’s Syndrome in Pregnancy. Laparoscopic Adrenalectomy during Pregnancy: The Mainstay Treatment. Journal of Endocrinological Investigation, 39, 273-276. https://doi.org/10.1007/s40618-015-0345-0
- 30. 吴兴成, 李汉忠, 纪志刚, 张玉石, 严维刚, 张学斌. 妊娠合并肾上腺库欣腺瘤的诊治经验总结[J]. 中华泌尿外科杂志, 2018, 39(4): 305-306.
- 31. Zhang, X., Liao, H., Zhu, X., Shi, D. and Chen, X. (2019) A Successful Pregnancy in a Patient with Secondary Hypertension Caused by Adrenal Adenoma: A Case Report. BMC Pregnancy and Childbirth, 19, Article No. 116. https://doi.org/10.1186/s12884-019-2262-2
- 32. Lin, W., Huang, H.B., Wen, J.P., et al. (2019) Approach to Cushing’s Syndrome in Pregnancy: Two Cases of Cushing’s Syndrome in Pregnancy and a Review of the Literature. Annals of Translational Medicine, 7, 490. https://doi.org/10.21037/atm.2019.07.94
- 33. Lu, Z., Luo, B., Yuan, Y., et al. (2020) Retroperitoneal Laparoscopic Resection of Adrenal Tumor in Pregnant Woman with Cushing’s Syndrome. Gynecological Endocrinology, 36, 465-468. https://doi.org/10.1080/09513590.2019.1698022
- 34. Gaujoux, S., Hain, É., Marcellin, L., et al. (2020) Adrenalectomy during Pregnancy: A 15-Year Experience at a Tertiary Referral Center. Surgery, 168, 335-339. https://doi.org/10.1016/j.surg.2020.03.019
- 35. Ildefonso-Najarro, S.P., Plasencia-Dueñas, E.A., Benites-Moya, C.J., Carrion-Rojas, J. and Concepción-Zavaleta, M.J. (2020) Pregnancy during the Course of Cushing’s Syndrome: A Case Report and Literature Review. Endocrinology, Diabetes & Metabolism Case Reports, 2020, Article ID: 20-0022. https://doi.org/10.1530/EDM-20-0022
- 36. 赵宁宁, 赵广彩, 王凤华, 侯灵彤, 刘海英. 妊娠合并库欣综合征2例报道并文献复习[J]. 现代妇产科进展, 2020. 29(9): 719-720.
- 37. Bronstein, M.D., Machado, M.C. and Fragoso, M.C. (2015) Management of Endocrine Disease: Management of Pregnant Patients with Cushing’s Syndrome. European Journal of Endocrinology, 173, R85-R91. https://doi.org/10.1530/EJE-14-1130
- 38. Kamoun, M., Mnif, M.F., Charfi, N., et al. (2014) Adrenal Diseases during Pregnancy: Pathophysiology, Diagnosis and Management Strategies. The American Journal of the Medical Sciences, 347, 64-73. https://doi.org/10.1097/MAJ.0b013e31828aaeee
- 39. Baghlaf, H.A., Badeghiesh, A.M., Suarthana, E. and Dahan, M.H. (2021) The Effect of Cushing’s Syndrome on Pregnancy Complication Rates: Analysis of More than 9 Million Deliveries. The Journal of Maternal-Fetal & Neonatal Medicine, 1-7. https://doi.org/10.1080/14767058.2021.1910658
- 40. Sridharan, K., Sahoo, J., Palui, R., et al. (2021) Diagnosis and Treatment Outcomes of Cushing’s Disease during Pregnancy. Pituitary, 24, 670-680. https://doi.org/10.1007/s11102-021-01142-7
- 41. Lindsay, J.R., Jonklaas, J., Oldfield, E.H. and Nieman, L.K. (2005) Cushing’s Syndrome during Pregnancy: Personal Experience and Review of the Literature. The Journal of Clinical Endocrinology & Metabolism, 90, 3077-3083. https://doi.org/10.1210/jc.2004-2361
- 42. Caimari, F., Valassi, E., Garbayo, P., et al. (2017) Cushing’s Syndrome and Pregnancy Outcomes: A Systematic Review of Published Cases. Endocrine, 55, 555-563. https://doi.org/10.1007/s12020-016-1117-0
- 43. Kita, M., Sakalidou, M., Saratzis, A., Ioannis, S. and Avramidis, A. (2007) Cushing’s Syndrome in Pregnancy: Report of a Case and Review of the Literature. Hormones (Athens), 6, 242-246.
- 44. Sek, K.S., Deepak, D.S. and Lee, K.O. (2017) Use of Cabergoline for the Management of Persistent Cushing’s Disease in Pregnancy. BMJ Case Reports, 2017, bcr2016217855. https://doi.org/10.1136/bcr-2016-217855
- 45. Pourali, L., Vatanchi, A.M. and Hamidi, A. (2017) A Case of Cushing’s Syndrome in Pregnancy. Iranian Journal of Medical Sciences, 42, 607-610.
- 46. Caimari, F., Corcoy, R. and Webb, S.M. (2018) Cushing’s Disease: Major Difficulties in Diagnosis and Management during Pregnancy. Minerva Endocrinology, 43, 435-445. https://doi.org/10.23736/S0391-1977.18.02803-1
- 47. Aron, D.C., Schnall, A.M. and Sheeler, L.R. (1990) Cushing’s Syndrome and Pregnancy. American Journal of Obstetrics & Gynecology, 162, 244-252. https://doi.org/10.1016/0002-9378(90)90859-6
- 48. Buescher, M.A., McClamrock, H.D. and Adashi, E.Y. (1992) Cushing Syndrome in Pregnancy. Obstetrics & Gynecology, 79, 130-137.
- 49. Vilar, L., Freitas Mda, C., Lima, L.H., Lyra, R. and Kater, C.E. (2007) Cushing’s Syndrome in Pregnancy: An Overview. Arquivos Brasileiros de Endocrinologia e Metabologia, 51, 1293-1302. https://doi.org/10.1590/S0004-27302007000800015
