Advances in Clinical Medicine
Vol.
11
No.
02
(
2021
), Article ID:
40494
,
8
pages
10.12677/ACM.2021.112081
劈离式肝移植中供肝IV段门静脉重建对受者术后早期肝功能恢复的应用价值初探
徐西良,王峰,徐庆国,王新,关鸽,孙延东,辛洋,臧运金
青岛大学附属医院器官移植中心,山东 青岛

收稿日期:2021年1月17日;录用日期:2021年2月2日;发布日期:2021年2月23日

摘要
目的:探讨在劈离式肝移植中供肝IV段门脉重建对术后早期肝功能恢复的意义。方法:回顾性分析2015年1月1日至2019年12月31日青岛大学附属医院器官移植中心16例劈离式肝移植右三叶受者的临床资料,按照是否进行IV段肝门脉重建分为两组,其中未进行门脉重建组(对照组) 4例,进行门脉重建组(重建组) 12例。观察两组受者术前、术后第1、3、7、14、30天丙氨酸氨基转移酶(alanine aminotransferase, ALT)、天冬氨酸氨基转移酶(aspartate aminotransferase, AST)、碱性磷酸酶(alkaline phosphatase, ALP)、γ-谷氨酰转肽酶(gamma-glutamyltransferase, GGT)、总胆红素(total bilirubin, TB)、直接胆红素(direct bilirubin, DB)、乳酸(lactic acid, lac)水平。使用R语言统计软件进行数据处理,正态分布计量资料以均值 ± 标准差表示,对独立样本采用t检验比较重建组与对照组。计数资料采用卡方检验进行比较。对P值小于0.05的数据认为具有统计学差异。结果:在受者观察指标中,两组受者术后第1天ALT、AST、ALP、lac,术后第3天ALT、ALP,术后7天ALT、lac,术后14天ALT、TB、DB差异存在统计学意义(P < 0.05),其余结果差异均无统计学意义(P > 0.05) 结论:供肝IV段门静脉重建对术后2周内肝功能恢复具有积极作用,应用供肝IV段门静脉重建技术有利于术后早期肝功能恢复。统计学上未发现供肝IV段门静脉重建对肝移植术后2周后肝功能恢复情况存在明显影响。
关键词
肝移植,劈离式,门静脉重建
Preliminary Study on Application Value of Segment IV Portal Vein Reconstruction in Split Liver Transplantation for Early Postoperative Recovery of Liver Function
Xiliang Xu, Feng Wang, Qingguo Xu, Xin Wang, Ge Guan, Yandong Sun, Yang Xin, Yunjin Zang
Organ Transplantation Center, The Affiliated Hospital of Qingdao University, Qingdao Shandong
Received: Jan. 17th, 2021; accepted: Feb. 2nd, 2021; published: Feb. 23rd, 2021

ABSTRACT
Objective: To explore the clinical value of segment IV portal vein reconstruction in split liver transplantation for early postoperative recovery of liver function. Methods: A retrospective analysis of 16 recipients with split liver transplantation from the Organ Transplantation Center of the Affiliated Hospital of Qingdao University from January 1st, 2015 to December 31st, 2019 was conducted. Two groups were divided according to whether IV portal vein reconstruction was performed. No portal vein reconstruction was performed in 4 patients (control group). Portal vein reconstruction was performed in 12 patients (reconstruction group). Alanine Aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), gamma-glutamyltransferase (GGT), Total bilirubin (TB), Direct bilirubin (DB), lactic acid (lac) levels were observed before surgery, 1 day after surgery, 3 days after surgery, 7 days after surgery, 14 days after surgery, and 30 days after surgery. Statistical software in R language was used for data processing. Normal distribution measurement data were expressed as mean ± standard deviation, and independent samples were compared between reconstruction group and control group by T-test. Non-normal distribution measurement data are represented by the median. Data with P value less than 0.05 were considered to have statistical difference. Results: Among the observed indicators of recipients, ALT, AST, ALP, lac of the two groups on the first day after surgery, ALT, ALP of the third day after surgery, ALT, lac of the seventh day after surgery, and ALT, TB, DB of the fourteenth day after surgery showed statistically significant differences (P < 0.05), while the other results showed no statistically significant differences (P > 0.05). Conclusions: IV portal vein reconstruction of the donor liver has a positive effect on the recovery of liver function within 2 weeks after the operation. The application of IV portal vein reconstruction of the donor liver is beneficial to the early recovery of liver function after the operation. There was no statistically significant effect of donor IV portal vein reconstruction on the recovery of liver function 2 weeks after liver transplantation.
Keywords:Liver Transplantation, Split Type, Portal Vein Reconstruction

Copyright © 2021 by author(s) and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/


1. 引言
劈离式肝移植已经成为扩大儿童和成人供肝来源的一种成熟的肝移植术式 [1] [2],在一些技术成熟的移植中心,劈离式肝移植受体存活率与全肝移植相当 [3] [4] [5]。在供肝劈离过程中,左外叶供肝获取后,IV段肝脏的门静脉分支在矢状部离断,使留下的部分IV段肝脏无门脉血供,影响术后肝功能恢复,术后肝脏缺血坏死、断面胆瘘等并发症的发生率约为40% [6]。我中心以供体髂血管架桥重建已经离断的部分IV段门脉分支,从而保留了IV段肝脏的门脉血供,保证有功能肝脏体积,提高了劈离式肝移植的移植效果,促进了移植肝功能早期恢复。同时扩大劈离式肝移植适用范围,扩大儿童和成人供肝来源。本研究回顾性分析青岛大学附属医院器官移植中心右三叶受者临床资料,比较供肝未进行门脉重建受者和供肝进行门脉重建受者的肝功能恢复情况。
2. 资料和方法
2.1. 研究对象
2015年1月1日至2019年12月31日在我中心接受右半肝、右三叶肝移植的受者,纳入标准:(1)具有肝移植的适应证,无禁忌证;(2) 术前终末期肝病模型(Model for end-stage liver disease, MELD)评分 < 30分 [7];(3) 成人受者移植物重量/受者体重(GRWR) ≥ 1.2%,儿童受者GRWR为2%~4% [8] [9];(4) 无多次腹部手术史。且供体符合米兰建议标准 [10]:(1) 年龄 < 55岁;(2) 血流动力学稳定,无需大剂量升压药物维持(多巴胺 ≤ 5mg/kg∙min,多巴酚丁胺 ≤ 10 mg/kg∙min,无肾上腺素或去甲肾上腺素);(3) ICU住院日 < 5天;(4) AST、ALT低于正常值2倍;(5) 肉眼下无脂肪肝表现,如进行肝穿刺活检则脂肪浸润 < 20%;(6) 血钠 < 155 mmol/L。所有供肝均为心脏死亡器官捐献,均由直系亲属签署器官捐献知情同意书,所有受者均签署由医院伦理委员会批准的患者知情同意书,符合医学伦理学规定。符合入组标准受者共16例,基本情况如下(见表1)。
Table 1. Recipient basic information
表1. 受者基本情况
2.2. 分组和观察指标
将16例受者中未进行门脉重建者纳入对照组(共4例),将进行门脉重建的患者纳入重建组(共12例)。比较患者术前、术后1天、术后3天、术后7天、术后14天、术后30天ALT、AST、ALP、GGT、TB、DB、lac水平。分析供肝IV段门脉重建在患者术后早期肝功能恢复中的意义。
2.3. 统计学方法
使用R语言统计软件进行数据处理,正态分布计量资料以均值 ± 标准差表示,对独立样本采用t检验比较重建组与对照组。计数资料采用卡方检验进行比较。对P值小于0.05的数据认为具有统计学差异。
3. 结果
3.1. 重建组和对照组受者术前资料的比较
两组患者术前各项指标差异均无统计学意义(P > 0.05),见表2。
Table 2. Comparison of preoperative data between reconstruction group and control group
表2. 重建组和对照组受者术前资料的比较
3.2. 重建组和对照组受者术后资料的比较
通过对重建组和对照组术后1天、3天、7天、14天、30天的ALT、AST、ALP、GGT、TB、DB、lac水平的比较可以发现,两组受者术后第1天ALT、AST、ALP、lac,术后第3天ALT、ALP,术后7天ALT、lac,术后14天ALT、TB、DB差异存在统计学意义(P < 0.05),其余指标未发现统计学差异。见表3~9。
Table 3. Postoperative ALT comparison between reconstruction group and control group (U/L)
表3. 重建组和对照组受者术后ALT对比(U/L)
Table 4. Postoperative AST comparison between reconstruction group and control group (U/L)
表4. 重建组和对照组受者术后AST对比(U/L)
Table 5. Postoperative ALP comparison between reconstruction group and control group (U/L)
表5. 重建组和对照组受者术后ALP对比(U/L)
Table 6. Postoperative GGT comparison between reconstruction group and control group (U/L)
表6. 重建组和对照组受者术后GGT对比(U/L)
Table 7. Postoperative TB comparison between reconstruction group and control group (µmol/L)
表7. 重建组和对照组受者术后TB对比(µmol/L)
Table 8. Postoperative DB comparison between reconstruction group and control group (µmol/L)
表8. 重建组和对照组受者术后DB对比(µmol/L)
Table 9. Postoperative lac comparison between reconstruction group and control group (mmol/L)
表9. 重建组和对照组受者术后lac对比(mmol/L)
3.3. 供肝IV段门脉重建对患者术后早期肝功能恢复的意义
从两组受者术后的各项指标恢复情况看,重建组肝功恢复情况明显优于对照组。两组受者术后均未发生严重的出血、胆瘘等并发症。对照组4例受者由于未进行IV段肝门脉重建,IV段肝脏灌注不足,超声均提示IV段肝脏较早出现萎缩坏死,ALT下降缓慢,术后早期肝功能恢复较差,导致TB、DB水平较高。重建组12例受者术后超声提示,受者术后2周内门脉重建血管均有血流通过,IV段肝脏萎缩速度较对照组明显减慢,术后肝功能恢复较快。
由此可见,术中对供肝IV段门静脉进行重建可有效减少肝细胞的破坏,保留更多的有功能肝组织,促进患者术后早期肝功能恢复,进而提高患者预后水平。
4. 讨论
1988年Pichlmayr等 [11] 完成了世界首例受者为1例儿童1例成人的劈离式肝移植。同年,Bismuth等 [12] 完成了世界首例受者为2例成人的劈离式肝移植。自此,劈离式肝移植技术开始应用,扩大了供肝来源,使更多终末期肝病患者获得及时的肝移植手术治疗。2002年我国上海瑞金医院完成了国内首例劈离式肝移植 [13],随着该技术的不断成熟,劈离式肝移植在我国已成为安全可靠的有效手术方式 [14],受限于供肝质量及外科技术,目前国内仅有几家大的移植中心开展。
供肝劈离过程中,关于供肝第IV肝段门静脉的处理仍存在争论,目前国外常采用的处理方式是结扎门静脉残端 [15]。门脉结扎后,肝IV无门脉血供萎缩坏死,影响肝功能恢复。我中心以供体髂血管架桥重建已经离断的部分Ⅳ段门脉分支,从而保证Ⅳ段肝脏的门脉血液供应,恢复门脉血供后,架桥血管充盈,肝脏未见明显缺血带(见图1~3)。
目前国内外尚缺少对劈离式肝移植中肝IV段门脉重建的报道,仅回顾性分析我中心两组受者可以发现,重建组和对照组受者在术后第1天ALT、AST、ALP、lac,术后第3天ALT、ALP,术后7天ALT、lac,术后14天ALT、TB、DB差异存在统计学意义。且由于重建组IV段肝脏存在门脉血供,减缓了IV段肝脏的萎缩坏死速度,争取到了更多有功能肝组织,可以有效避免出血、胆瘘等并发症的发生,有利于术后早期肝功能的恢复。这一结果提示我们,劈离式肝移植术中进行IV段门脉重建对受者术后早期肝功能的恢复具有积极作用,在临床实践中具有一定的指导意义。

Figure 1. Iliac vessel reconstruction
图1. 髂血管架桥
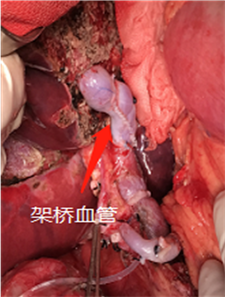
Figure 2. Reconstruction of blood vessels after restoration of blood supply
图2. 恢复血供后架桥血管

Figure 3. The liver after restoration of blood supply
图3. 恢复血供后肝脏
综上所述,我中心对于劈离式肝移植中对于肝IV段门脉重建的探索,是基于解剖学基础上的合理尝试,在临床实践中有利于患者术后早期肝功能的恢复。探究供肝IV段门脉重建在劈离式肝移植中的应用价值,为进一步完善手术方式提供理论依据,为扩大儿童和成人供肝来源提供新的思路。但由于该手术方式处于早期探索阶段,本次研究纳入样本数量有限,且受限于术者技术水平差异,该结果存在一定的局限性,有待继续扩大样本量、多中心实践进一步验证。
文章引用
徐西良,王 峰,徐庆国,王 新,关 鸽,孙延东,辛 洋,臧运金. 劈离式肝移植中供肝IV段门静脉重建对受者术后早期肝功能恢复的应用价值初探
Preliminary Study on Application Value of Segment IV Portal Vein Reconstruction in Split Liver Transplantation for Early Postoperative Recovery of Liver Function[J]. 临床医学进展, 2021, 11(02): 559-566. https://doi.org/10.12677/ACM.2021.112081
参考文献
- 1. Gavriilidis, P., Roberts, K.J. and Azoulay, D. (2018) Right Lobe Split Liver Graft versus Whole Liver Transplantation: A Systematic Review by Updated Traditional and Cumulative Meta-Analysis. Digestive and Liver Disease, 50, 1274-1282. https://doi.org/10.1016/j.dld.2018.08.025
- 2. Gavriilidis, P., Tobias, A., Sutcliffe, R.P., et al. (2018) Survival Following Right Lobe Split Graft, Living- and Deceased-Donor Liver Transplantation in Adult Patients: A Systematic Review and Network Meta-Analysis. Transplant International, 31, 1071-1082. https://doi.org/10.1111/tri.13317
- 3. Mourad, M.M., Liossis, C., Kumar, S., et al. (2014) Vasculobiliary Complications Following Adult Right Lobe Split Liver Transplantation from a Perspective of Reconstruction Techniques. Liver Transplantation, 21, 63-71. https://doi.org/10.1002/lt.24015
- 4. Moussaoui, D., Toso, C., Nowacka, A., et al. (2017) Early Complications after Liver Transplantation in Children and Adults: Are Split Grafts Equal to Each Other and Equal to Whole Livers? Pediatric Transplantation, 21, e12908. https://doi.org/10.1111/petr.12908
- 5. Zimmerman, A., Flahive, J.M., Hertl, M., et al. (2016) Outcomes of Full-Right-Full-Left Split Liver Transplantation in Adults in the USA: A Propensity-Score Matched Analysis. International Journal of Organ Transplantation Medicine, 7, 69-76.
- 6. 滕大洪. 劈离式肝移植术临床进展[J]. 实用器官移植电子杂志, 2017, 5(4): 309-314.
- 7. Nadalin, S., Schaffer, R. and Fruehauf, N. (2009) Split-Liver Transplantation in the High-MELD Adult Patient: Are We Being Too Cautious? Transplant International, 22, 702-706. https://doi.org/10.1111/j.1432-2277.2009.00850.x
- 8. Lee, W.C., Chan, K.M., Chou, H.S., et al. (2013) Feasibility of Split Liver Transplantation for 2 Adults in Themodel of End-Stage Liver Disease Era. Annals of Surgery, 258, 306-311. https://doi.org/10.1097/SLA.0b013e3182754b8e
- 9. Hashimoto, K., Quintini, C., Aucejo, F.N., et al. (2014) Split Liver Transplantation Using Hemiliver Graft in the MELD Era: A Single Center Experience in the United States. American Journal of Transplantation, 14, 2072-2080. https://doi.org/10.1111/ajt.12791
- 10. Aseni, P., De Feo, T.M., De Carlis, L., Valente, U., et al. (2014) A Prospective Policy Development to Increase Split-Liver Transplantation for 2 Adult Recipients: Results of a 12-Year Multicenter Collaborative Study. Annals of Surgery, 259, 157-165. https://doi.org/10.1097/SLA.0b013e31827da6c9
- 11. Pichlmayr, R., Ringe, B., Gubernatis, G., et al. (1988) Transplantation of a Donor Liver to 2 Recipients (Splitting Transplantation)—A New Method in the Further Development of Segmental Liver Transplantation. Langenbecks Archiv für Chirurgie, 373, 127-130. https://doi.org/10.1007/BF01262776
- 12. Bismuth, H., Morino, M., Castaing, D., et al. (1989) Emergency Orthotopic Liver Transplantation in Two Patients Using One Donor Liver. British Journal of Surgery, 76, 722-724. https://doi.org/10.1002/bjs.1800760723
- 13. 黄洁夫. 中国肝脏移植[M]. 北京: 人民卫生出版社, 2008.
- 14. Shen, Z. (2011) The Liver Transplant Program at Tianjin First Center Hospital. Clinical Transplantation, 203-211.
- 15. Frühauf, N., Malagó, M., Frilling, A., et al. (2004) Latest Development in Split Liver Transplantation. Surgical Technology International, 13, 183-189.
