Advances in Clinical Medicine
Vol.
13
No.
02
(
2023
), Article ID:
61875
,
7
pages
10.12677/ACM.2023.132402
单侧PVP治疗胸腰椎骨质疏松性压缩骨折安全有效:同一术者连续性病例分析
王冠兴1,李彦明2*,刘相旭1
1济宁医学院,临床医学院,山东 济宁
2济宁医学院附属医院,山东 济宁
收稿日期:2023年1月26日;录用日期:2023年2月19日;发布日期:2023年2月27日

摘要
目的:观察单侧穿刺经皮椎体成形术治疗骨质疏松性胸腰椎骨折的临床疗效及安全性。方法:骨质疏松性胸腰椎骨折患者91例,采用单侧穿刺经皮椎体成形术治疗,分别于术前、术后1天、术后3个月采用oswestry功能障碍指数(oswestry disability index, ODI)和疼痛强度数字评分法(numeric rating scales, NRS)评估患者疼痛情况。结果:治疗前、后比较ODI指数、NRS评分差异有统计学意义(P < 0.05)。结论:单侧PVP治疗骨质疏松性胸腰椎骨折安全性好、疗效满意。
关键词
NRS,ODI,骨质疏松性椎体压缩性骨折,PVP,PKP

Unilateral Percutaneous Vertebroplasty Is Safe and Effective in the Treatment of Osteoporotic Vertebral Compression Fractures: Continuous Case Analysis of the Same Surgeon
Guanxing Wang1, Yanming Li2*, Xiangxu Liu1
1College of Clinical Medicine, Jining Medical University, Jining Shandong
2Affiliated Hospital of Jining Medical University, Jining Shandong
Received: Jan. 26th, 2023; accepted: Feb. 19th, 2023; published: Feb. 27th, 2023

ABSTRACT
Background: To observe the clinical efficacy and safety of unilateral percutaneous vertebroplasty (PVP) in the treatment of osteoporotic vertebral compression fractures (OVCFs). Methods: The retrospective study included 91 patients (age range 53~91 years) with OVCFs treated with PVP from March 2018 to December 2019 in our department. A visual analog scale (VAS) and the Chinese modified Oswestry Disability Index were used to evaluate the pain before and after PVP. The numeric rating scales (NRS) and Oswestry Disability Index (ODI) were used to evaluate the pain preoperative, 1 day and 3 months postoperative respectively. Results: The mean NRS score and ODI were reduced from 7.25% ± 0.77% to 2.79% ± 0.80%, 1.40% ± 0.53% and 69.65% ± 4.41% to 20.95% ± 5.55%, 10.24% ± 3.92%, respectively. Postoperative NRS score and ODI were significantly improved (P < 0.05). Conclusion: Unilateral PVP is safe and effective in the treatment of OVCF.
Keywords:Numeric Rating Scales, Oswestry Disability Index, Osteoporotic Vertebral Compression Fractures, Percutaneous Vertebroplasty, Percutaneous Kyphoplasty

Copyright © 2023 by author(s) and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/


1. 引言
世界上很多国家,包括中国,已经进入老龄化社会,骨质疏松性椎体压缩骨折(osteoporotic vertebral compressrion fratures, OVCF)已经成为中国医疗工作者必须面临的严重公共健康问题。经皮穿刺椎体成形术(percutaneous vertebroplasty, PVP)和经皮穿刺后凸成形术(percutaneous kyphoplasty, PKP)是治疗OVCF的常用方法。孰优孰劣目前尚无定论。双侧穿刺方法治疗OVCF为经典入路 [1] ,但是单侧穿刺手术时间短、出血少、骨水泥用量少,越来越获得矫形外科医生的认可。为了进一步探讨单侧穿刺PVP治疗OVCF患者的临床效果,该研究对本人于2018年03月~2019年12月连续接诊并手术的91例患者进行疗效分析。本研究是回顾性资料,术前均已签署知情同意书,数据为通过查阅患者的病史资料及随访获得,不涉及生物样本,故无需再获得患者的知情同意。现报道如下。
2. 资料与方法
2.1. 一般资料
纳入标准:1) 符合骨质疏松症诊断标准(基于DXA骨密度或脆性骨折);2) 无明显脊髓和神经根受压症状和体征;3) 因疼痛接受椎体骨水泥强化治疗;4) 无原发或转移肿瘤并排除感染;5) MRI检查明确诊断为椎体新鲜压缩性骨折或kummell病;6) 随访资料完整。
2018年03月至2019年12月我院脊柱外科连续收住院、符合纳入标准接受手术并本人主刀的OVCF患者共91例。患者年龄53~91岁,平均70岁。女72例,男19例。总椎体数116个。其中伤椎数量:1个节段72例,2节段14例,3节段4例,4个节段1例。伤椎数量分布:T6 1例,T7 1例,T8 7例,T9 5例,T10 5例,T11 15例,T12 18例,L1 28例,L2 16例,L3 9例,L4 6例,L5 5例(图1)。病史最长15年,最短2天。术前有血栓患者4例。术后再骨折2例。多次骨折19例,其中相邻椎体再骨折8例。发病诱因:无明显外伤56例,轻微外伤(扭伤、站立位摔倒) 25例,暴力外伤(车祸、高处坠落) 10例。

Figure 1. The distribution of the fractured vertebrae
图1. 骨折椎体的分布情况
2.2. 手术方法
患者俯卧位,C型臂X线机透视定位病变椎体,定位体表标志,确定进针点,用1%利多卡因局部麻醉,透视下利用直向穿刺针经左侧椎弓根穿刺直至病椎椎体后缘前约5 mm处,正位透视确认入针点位于椎弓根影的外上象限且未突破椎弓根内壁,侧位透视调节穿刺针的深度和方向,拔出穿刺针芯,经穿刺针外套管置入实心钻,侧位透视下达到椎体前中1/3处,正位透视钻头接近或达到中体中线位置。准备骨水泥,于骨水泥拔丝期时,缓慢推注,C型臂X线机全程透视下观察骨水泥弥散情况,当其充盈接近椎体后壁时,立即停止注入。待骨水泥稍硬化后,先旋转穿刺针再拔出,以便分离管腔内与椎体内的骨水泥,防骨水泥拖尾现象。
患者术后平卧,观察生命体征及双下肢感觉运动情况,术后4 h佩戴腰围等支具可下地活动。
2.3. 观察指标
所有患者均进行3月以上随访。记录患者手术时间和骨水泥注入量,以及术前、术后1天及3个月oswestry功能障碍指数(oswestry disability index, ODI)和疼痛强度数字评分(numeric rating scales, NRS)。
2.4. 统计学分析
所得数据均采用SPSS 18.0进行统计学处理分析,计量资料用均数 ± 标准差(x ± s)示,采用t检验,P < 0.05为差异有统计学意义。
3. 结果
3.1. 患者一般情况
所有患者手术过程顺利,术后随访3~24个月。术后其他节段椎体再发骨折2例,给予再次经皮椎体成形术、加强抗骨质疏松后症状明显好转。
3.2. NRS评分
术前、术后1天和术后3个月NRS评分分别为7.3 0.8、2.8 0.8和1.4 0.5。术后疼痛明显低于术前(P < 0.01),术后3个月也显著低于术后1天(P < 0.01;图2)。术后1天、3个月NRS较术前明显降低,术后1天、3个月NRS未见明显升高。
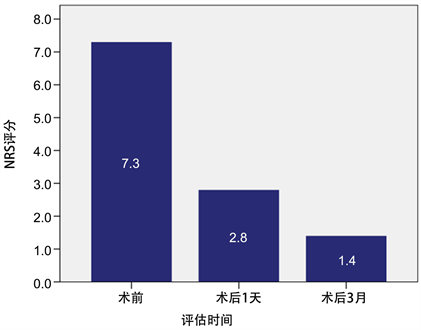
Figure 2. NRS scores before and 1 day, 3 months after surgery
图2. 术前、术后1天、术后3个月NRS评分
3.3. ODI指数
术前、术后1天、3个月ODI分别为69.6 4.4%、20.9 5.5%、10.2 3.9%。术后较术前明显降低(P < 0.01),术后3个月,ODI也低于术后1天(P < 0.01;图3) (表1)。术后1天、3个月ODI指数,较术前明显下降,术后1天、术后3个月ODI指数未见明显变化。
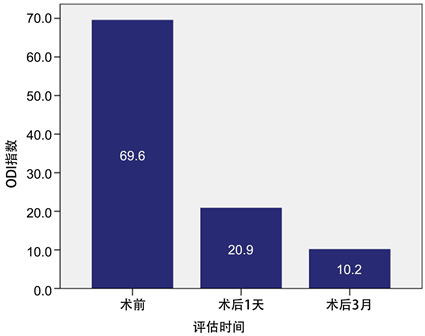
Figure 3. ODI before and 1 day, 3 months after surgery
图3. 术前、术后1天、术后3个月ODI (%)
Table 1. NRS scores and ODI of patients at different time
表1. 不同时间患者的NRS评分及ODI ( )
注:与术前比较*P < 0.01;与术后1天比较§P < 0.01。
3.4. 手术情况
所有患者在透视下规范采用经皮椎体成形术,未见神经、脊髓、大血管损伤及肺栓塞。未见椎体后方渗漏。术中3例患者出现骨水泥毒性反应,给予静推5 mg地塞米松后很快缓解。所有患者疼痛耐受性好,未有因疼痛终止手术者。所有患者术后1天拆线出院。术口愈合良好,无感染。
4. 讨论
我国已经进入老龄化社会,2019年我国人口已经突破14亿,60岁以上老人占18.1%,65岁以上老人占12.6%。约50%的女性和20%的男性在50岁之后会遭遇初次OVCF。随着人口老龄化日趋严重,OVCF已成为我国面临的重要公共健康问题。骨质疏松性骨折长期卧床者的致死率可达20%、永久性致残率可达50%。作为医务工作者,我们必须使OVCF患者尽快从床上站立来,恢复正常活动。
而目前治疗OVCF的方法有保守治疗和微创手术治疗,而最常用的微创手术方法就是PVP或PKP。术后数小时即可下床活动,手术治疗可迅速缓解疼痛,改善日常活动能力。穿刺方法有单侧穿刺或双侧穿刺。到底应该采用PVP还是PKP,应该采取单侧穿刺还是双侧穿刺?这两个问题是困扰脊柱外科医师治疗OVCF时手术选择的主要问题。
4.1. PVP还是PKP?
PVP是指经皮通过椎弓根或椎弓根外向骨折的椎体内注入骨水泥,以达到稳定骨折、恢复椎体力学强度和刚度、防止椎体进一步压缩,从而起到缓解腰背部疼痛为目的的一种微创技术 [2] 。1987年Galibert和Deramond采用PVP治疗1例颈椎血管瘤取得成功 [3] ,PVP技术从1994年率先介绍到美国 [4] 。随着其应用逐渐推广,不仅在脊椎血管瘤、溶骨性转移瘤、骨髓瘤中适用,而且在骨质疏松性胸腰椎压缩性骨折中逐渐应用起来。逐渐成为治疗骨质疏松性胸腰椎压缩性骨折最为常用的方案,其止痛效果立竿见影。PKP是在PVP基础上发展而来的微创技术,它是利用一种可膨胀性球囊经皮穿刺置入椎体并扩张,从而抬高终板,恢复椎体高度。
PVP通过向伤椎体内注入骨水泥,改善伤椎强度及脊柱后凸畸形,恢复伤椎高度,提高脊柱稳定性,能较快减轻患者的背部疼痛及预防椎体塌陷加重,且能避免因长期卧床导致的多种并发症 [5] [6] 。此外,PVP术局麻风险小、创伤小、手术时间短,操作简单、恢复快,向椎体注入少量骨水泥即可达到手术目的 [7] [8] 。
Hu等 [9] 人在一项回顾性研究中发现,PKP组手术时间长于PVP组,术后随访期间,两组患者再发骨折的风险无显著差异。Zhang等 [10] 在纳入2852例椎体压缩骨折的网状Meta分析中发现PVP在改善椎体后凸畸形和降低再骨折方面更有优势。PVP手术时间较PKP短,可降低手术风险,有利于患者术后的恢复 [11] 。
本研究所有患者均采用PVP治疗,住院总费用约15,000元。如果使用PKP,费用将增加一倍左右。PVP大大降低了患者的成本,节省了社会资源,减轻了患者家庭的负担。
4.2. 单侧穿刺还是双侧穿刺?
目前PVP的手术入路主要分为单侧与双侧经椎弓根穿刺两种,但选择何种入路方式更佳一直存在着争议 [12] 。有研究认为骨水泥在伤椎体内弥散情况与缓解疼痛的效果相关,而双侧入路较单侧更有利于骨水泥广泛弥散,双侧入路更有优势 [13] 。然而单侧入路因为有手术时间短、放射次数少、创伤小等优势,被大多数临床医师所选择 [14] 。
Chen等 [15] 通过Meta分析,发现椎体成形术对于治疗OVCF,单侧穿刺入路优于双侧穿刺入路。此外,对于强化椎体强度、骨水泥充盈、止痛效果方面,单侧与双侧穿刺差异无统计学意义 [16] 。因此,对于相邻多节段椎体骨折患者和不能耐受长期手术的老年患者,双侧穿刺更容易造成手术困难或增加手术风险。为了提高单侧穿刺成功率,临床应用了实时ct-超声融合成像技术,该技术易于实施,提高了无放射 [17] 的穿刺成功率。
所有病例均采用单侧穿刺,本研究均取得成功。如果一开始穿刺角度较小,可以借助术中透视加大穿刺角度,顺利完成手术。
OVCF患者就医的主要原因是腰痛,少数患者出现腹痛。PVP的主要目的是缓解疼痛,让患者尽早下床,提高生活质量。但部分OVCF患者在PVP后仍存在不同程度的残留疼痛 [18] [19] [20] [21] 。Yan等认为胸腰筋膜损伤与PVP [22] 后残留的腰痛可能有一定的关系。应进一步研究术后残余疼痛与下背部软组织损伤的关系。
我们的研究有几个局限性。首先,虽然ODI被广泛用于测量脊柱疾病的残疾,但由于保守的思维和回答性相关问题的禁忌,它无法被中国大陆的人们正确理解和接受 [23] 。本研究使用中国改良的ODI [24] 来评估残疾。这个版本的ODI删除了性生活项目,只剩下9个项目。然而,与其他语言的对外直接投资评估相比,它要粗略得多。第二,本研究样本量较小,仅有91例患者116个椎体。我们将继续积累病例资料,以获得更有说服力的结论。第三,这项研究是一项回顾性研究。需要大样本的随机对照研究来证实这些结果。
5. 结论
综上所述,OVCF患者应尽早采取微创手术,减轻疼痛,尽早起床,提高生活质量。单侧PVP治疗OVCF安全、有效、经济。
文章引用
王冠兴,李彦明,刘相旭. 单侧PVP治疗胸腰椎骨质疏松性压缩骨折安全有效:同一术者连续性病例分析
Unilateral Percutaneous Vertebroplasty Is Safe and Effective in the Treatment of Osteoporotic Vertebral Compression Fractures: Continuous Case Analysis of the Same Surgeon[J]. 临床医学进展, 2023, 13(02): 2847-2853. https://doi.org/10.12677/ACM.2023.132402
参考文献
- 1. 杨惠林, Hansen A Yuan, 等. 椎体后凸成形术疗老年骨质疏松脊柱压缩骨折[J]. 中华骨科杂志, 2003, 23(5): 262-265.
- 2. Fahed, R., et al. (2016) Safety and Clinical Effectiveness of Percutaneous Vertebroplasty in the Elderly (≥80 Years). European Radiology, 26, 2352-2358. https://doi.org/10.1007/s00330-015-4035-2
- 3. Galibert, P., Deramond, H., et al. (1987) Preliminary Note on the Treatment of Vertebral Angioma by Percutaneous Acrylic Vertebro-plasty. Neuro-Chirurgie, 33, 166-168.
- 4. 赵必增, 贾连顺, 等. 椎体成形术及其进展[J]. 骨与关节损伤杂志, 2001, 16(6): 470.
- 5. Yi, H., Jeong, J., et al. (2016) Percutaneous Vertebroplasty versus Conservative Treatment for One Level Thoracolumbar Osteoporotic Compression Fracture: Results of an over 2-Year Follow-Up. Pain Physician, 19, E743-E750. https://doi.org/10.36076/ppj/2019.19.E743
- 6. Suhail, A., Shabir, D., et al. (2007) Percutaneous Vertebroplasty for Osteoporotic Fractures. Pain Physician, 10, 559-563.
- 7. Kaufmann, T.J., et al. (2006) The Effects of Cement Volume on Clinical Outcomes of Percutaneous Vertebroplasty. AJNR. American Journal of Neuroradiology, 27, 1933-1937.
- 8. Liebschner, M., Rosenberg, W., et al. (2001) Effects of Bone Cement Volume and Distribution on Vertebral Stiffness after Vertebroplasty. Spine, 26, 1547-1554. https://doi.org/10.1097/00007632-200107150-00009
- 9. Hu, K.-Z., Chen, S.-C. and Xu, L. (2018) Comparison of Percutaneous Balloon Dilation Kyphoplasty and Percutaneous Vertebroplasty in Treatment for Thoracolumbar Verte-bral Compression Fractures. European Review for Medical and Pharmacological Sciences, 22, 96-102.
- 10. Zhang, Y.L., et al. (2017) Comparison of the Efficacy between Two Micro-Operative Therapies of Old Patients with Osteopo-rotic Vertebral Compression Fracture: A Network Meta-Analysis. Journal of Cellular Biochemistry, 118, 3205- 3212. https://doi.org/10.1002/jcb.25966
- 11. Katrin, E., Stephan, Z., et al. (2014) Outcome of Long-Axis Percutaneous Sacroplasty for the Treatment of Sacral Insufficiency Fractures with a Radiofrequency-Induced, High-Viscosity Bone Cement. Skeletal Radiology, 43, 493-498. https://doi.org/10.1007/s00256-013-1811-4
- 12. Teles, A.R. and Mattei, T.A. (2015) Vertebral Augmentation in Thoracolumbar Compression Fractures: A Critical Review on Available Evidence and Ongoing Controversies. Minerva Ortopedica e Traumatologica, 66, 25-39.
- 13. Agnieszka, S. and Zbigniew, K. (2014) Treatment of Multiple Osteopo-rotic Vertebral Compression Fractures by Percutaneous Cement Augmentation. International Orthopaedics, 38, 2309-2312. https://doi.org/10.1007/s00264-014-2470-3
- 14. Yang, J.Y., Lee, J.K., et al. (2011) Clinical Results of Unilateral Partial Vertebroplasty (UPVP) in Osteoporotic Vertebral Fracture. Journal of Korean Society of Spine Surgery, 18, 64-69. https://doi.org/10.4184/jkss.2011.18.2.64
- 15. Chen, X.F., et al. (2018) Is Unilateral Percutaneous Kyphoplasty Superior to Bilateral Percutaneous Kyphoplasty for Osteoporotic Vertebral Compression Fractures? Evidence from a Systematic Review of Discordant Meta-Analyses. Pain Physician, 21, 327-336.
- 16. Dones, I., Messina, G., et al. (2011) A Modified Visual Analogue Scale for the Assessment of Chronic Pain. Neurological Sciences, 32, 731-733. https://doi.org/10.1007/s10072-011-0570-z
- 17. Li, S., Mi, S., et al. (2019) Application of Ultrasound Fusion Im-aging Technique for Unilateral Percutaneous Vertebroplasty in Treatment of Osteoporotic Thoracolumbar Compression Fracture. Journal of X-Ray Science and Technology, 28, 171-183. https://doi.org/10.3233/XST-190563
- 18. Barr, Lemley, et al. (2000) Percutaneous Vertebroplasty for Pain Relief and Spinal Stabilization. Spine (Phila Pa 1976), 25, 923-928. https://doi.org/10.1097/00007632-200004150-00005
- 19. Diamond, T.H., Champion, B., et al. (2003) Management of Acute Osteoporotic Vertebral Fractures: A Nonrandomized Trial Comparing Percutaneous Vertebro-plasty with Conservative Therapy. The American Journal of Medicine, 114, 257-265. https://doi.org/10.1016/S0002-9343(02)01524-3
- 20. Layton, K.F., Thielen, K.R., et al. (2007) Vertebroplasty, First 1000 Levels of a Single Center: Evaluation of the Outcomes and Complications. American Journal of Neuroradiol-ogy, 28, 683-689.
- 21. Kobayashi, K., Shimoyama, K., et al. (2005) Percutaneous Vertebroplasty Immediately Relieves Pain of Osteoporotic Vertebral Compression Fractures and Prevents Prolonged Immobilization of Patients. European Radiology, 15, 360- 367. https://doi.org/10.1007/s00330-004-2549-0
- 22. Yan, Y., Xu, R. and Zou, T. (2015) Is Thoracolumbar Fascia Injury the Cause of Residual Back Pain after Percutaneous Vertebroplasty? A Prospective Cohort Study. Osteoporosis International, 26, 1119-1124. https://doi.org/10.1007/s00198-015-3177-z
- 23. Liu, H., Tao, H.R. and Luo, Z.J. (2009) Validation of the Simpli-fied Chinese Version of the Oswestry Disability Index. Spine, 34, 1211-1216. https://doi.org/10.1097/BRS.0b013e31819e2b34
- 24. Zhen, G.X. and Zhao, X.O. (2002) Reliability of the Modi-fied Oswestry Disability Index for Evaluating Patients with Low Back Pain.
NOTES
*通讯作者。
