Medical Diagnosis
Vol.
10
No.
01
(
2020
), Article ID:
34464
,
7
pages
10.12677/MD.2020.101003
Significance of Mitral E/Ea Estimation in Cases of Coronary Heart Disease with Different Left Ventricular Ejection Fractions
Sheng He, Yingming Liu, Xin Li, Qiuying Liu, He Ren
Dept. Ultrasonography of the Sixth Medical Center of the General Hosp. PLA, Beijing

Received: Feb. 19th, 2020; accepted: Mar. 4th, 2020; published: Mar. 11th, 2020

ABSTRACT
Object: To understand the changes and clinical meanings of mitral E/Ea in cases of coronary heart disease (CHD) with different systolic functions of left ventricle. Methods: According to LVEFs measured by echocardiography, 107 patients with CHD diagnosed by coronary arteriography were divided into three groups: 62cases of LVEF >50% in group I, 24 cases of LVEF 45%~50% in group II and 21 cases of LVEF < 45% in group III. Indications to be observed mainly included LVEF, ratio of mitral diaslotic early flow velocity E to mitral late flow velocity A (E/A), diaslotic early velocity wave of mitral anulus (e, Ea), ratio of E/Ea and levels of plasma Brain-type natriuretic peptide (BNP). Results: Diameters of left ventricle in group III were larger than those in group I, while LVEFs in group III were lower than those in group I and group II, with LVEFs in group II being lower than that in group I, too (all p < 0.05). Differences of E/A among the three groups and of E/Ea between group II and group III were not obvious(all p > 0.05), but ratios of E/Ea in group II and group III were higher than those in group I (both p < 0.05). The mean value of BNP in all the 107 cases was at a higher level, among which values of BNP in group II and group III were higher than those in group I, and the value of BNP in group III was also higher than that in group II (all p < 0.05). Based on analysis of all the 107 cases, there was a positive correlation between E/Ea and BNP, but there were negative correlations between BNP and LVEF and between E/Ea and LVEF (all p < 0.05). The similar linear correlations to those in all the 107cases were also seen in group I, however these correlations, including between E/Ea and BNP, BNP and LVEF as well as E/Ea and LVEF could not be found in group II and group III. Conclusions: Although there were clear correlations between E/Ea and both LVEF and BNP in analysis of a larger sample, there were some unidentical changes between E/Ea and LVEF, which showed that the lesions of systolic dysfunction could be inconsistent with those of diastolic dysfunction in some cases of CHD, and that the unidentical changes needed to be diagnosed by the clinical and laboratory data of the patients.
Keywords:Coronary Heart Disease, Left Ventricular Ejection Fractions, Mitral E/Ea

冠心病患者不同左心室射血分数二尖瓣口E/Ea的观测意义
贺声,刘英明,李馨,刘秋颖,任贺
中国人民解放军总医院第6医学中心超声科,北京
收稿日期:2020年2月19日;录用日期:2020年3月4日;发布日期:2020年3月11日

摘 要
目的:了解冠心病患者不同心室收缩状态下二尖瓣口E/Ea的变化及观测意义。资料与方法:107例经冠脉造影确诊的冠心病按超声心动图测定的LVEF大小分为3组:LVEF > 50% 62例为I组,LVEF45%~50% 24例为II组,LVEF < 45% 21例为III组。观测指标主要包括:超声心动图心脏常规测量计算LVEF、二尖瓣口血流E/A比值、二尖瓣环舒张早期运动速度e波(Ea)、计算E/Ea比值及BNP。结果:III组的左心室内径明显大于I组、而其LVEF明显低于I组、II组,II组的LVEF也低于I组(p值均 < 0.05);3组之间的E/A差异不显著,II组、III组之间的E/Ea差异不大(p > 0.05),但是与I组比较则均有明显差异(p值均 < 0.05);107例的BNP平均值较高,其中II组、III组明显高于I组,III组也高于II组;以107例为分析样本,E/Ea与BNP呈正相关,BNP与LVEF、E/Ea与LVEF则呈负相关(p值均 < 0.05);在I组中也基本保持了这样的相关关系,而在II组、III组中,不论是E/Ea与BNP、BNP与LVEF,还是E/Ea与LVEF之间均未呈现明显的线性相关。结论:在较大的样本中E/Ea与LVEF及BNP表现出较为明确的线性相关,但也存在着E/Ea的变化程度与LVEF不一致的情况,说明冠心病患者可存在着左心室收缩障碍与舒张功能减低程度的不一致,需要结合患者临床和相关实验室检查加以综合判断。
关键词 :冠心病,左室射血分数,二尖瓣口E/Ea

Copyright © 2020 by author(s) and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/


1. 引言
冠心病不仅影响心室收缩功能,对舒张功能亦有明显影响,即心室收缩功能受损经常伴随着舒张功能异常,而临床上舒张功能障碍性心衰与常见的充血性心衰的治疗方法不同,如为单纯性舒张功能障碍性心衰却按收缩性功能障碍性心衰来治疗,疗效可能会不明显甚至病情加重;随着临床对心衰机制认识加深和治疗方案的改进,同时有收缩和舒张功能障碍的心衰与以舒张功能不全为主的心衰的最佳治疗方案的差异也很大,应加以鉴别 [1]。常规超声心动图可对左心室功能做出评估,其中舒张早期二尖瓣血流峰速度(E)与舒张早期二尖瓣环速度(Ea)的比值(E/Ea)被欧洲心脏病协会(ESC)推荐为评估左心室舒张末压的有效指标 [2] [3]。本文通过分析1组冠心病患者E/Ea值的改变,了解其在不同左心室收缩状态下的观测价值。
2. 资料与方法
观察对象 本组107例为我院2007年9月~2015年1月住院患者,纳入观察标准:均为经冠状动脉造影确诊为冠心病者。根据超声心动图测定左心室射血分数(LVEF)分为3个组:LVEF > 50% 62例为I (左心室收缩功能正常或射血分数正常组nEF)组,LVEF45%~50% 24例为II (左心室收缩功能保留或射血分数保留性心衰HF with preserved ejection fractions, HF-pEF)组,LVEF < 45% 21例为III (左心室收缩功能减低或射血分数减低性heart failiue with reduced ejection fraction, HF-rEF)组。排除指征:检查期间有房颤、频发早搏、起搏心律、二尖瓣环钙化、人工二尖瓣/主动脉瓣、二尖瓣、主动脉瓣明显关闭不全者不纳入观察对象。
方法:超声心动图检查用GE vivid7超声仪,探头频率为3.5 MHZ,可同步进行M型、2D动态显示。常规测量心脏各腔室大小,计算LVEF。心尖四腔心切面上频谱Doppler测量二尖瓣口血流,组织Doppler (TDI)测量二尖瓣环室间隔和左室侧壁2个位点的运动速度。二尖瓣口血流测量包括舒张早期血流速度E峰、舒张晚期血流速度A峰、E/A比值及E峰下降时间DTEV (deceleration time of E velocity);二尖瓣环测量包括舒张早期运动速度e波、舒张晚期运动速度a波、e/a比值;利用二尖瓣环2个位点的e波均值Ea计算E/Ea比值(图1)。
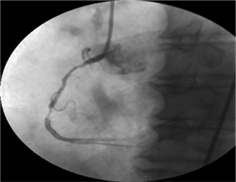
Figure 1. Male, 60 y, inferior myocardiac infarction of left ventricle, LVEF 51.09%, BNP 155.4 ng/L, E/Ea 12.55 at ventricular septal site of mitral anulus
图1. 男,60岁,下壁心梗,LVEF 51.09%,BNP 155.4 ng/L,二尖瓣环室间隔位点E/Ea 12.55
血浆脑型利钠肽(BNP)测定采用酶联免疫吸附法,所用仪器为美国产BIO-TEKELX800型酶标仪,试剂盒由美国TPI Inc.公司提供,单位ng/L,灵敏度为5 ng/L。
统计学处理:计量数据采用均数±标准误( )表示。应用t检验和配对t检验进行统计分析,p < 0.05为统计学有差异。
3. 结果
临床一般资料:3组患者的一般临床状况,包括年龄、性别比例、高血压、糖尿病、高脂血症患病率、冠状动脉介入史、搭桥史、脑卒中史、心肌梗死病史等的比较见表1。3组患者的年龄、性别比例、基础疾病等差异不明显,但是I组以往的心梗和心功能不全的发病率均低于II组与III组,I组中的冠脉多支病变率也明显低于III组。
超声心动图指标中,III组的左心室内径明显大于I组、而其LVEF明显低于I组、II组,II组的LVEF也低于I组;反映左心室舒张功能指标中,3组之间的二尖瓣口E/A差异不显著,II组、III组之间的TDIe、E/Ea差异不大,但是与I组比较则均有明显差异,而III组的DTEV较I组有延长。107例的BNP平均值较高,其中II组、III组明显高于I组,III组也高于II组(见表2)。
Table 1. Clinical data of 107 cases
表1. 107例一般临床资料的比较
注:PCI: percutaneous coronary intervention;CABG: coronary artery bypass grafting surgery;*III组与I组比较,p ≤ 0.05;#I组与II组、III组比较,p ≤ 0.05。
Table 2. Comparison of the data of echocardiography and BNP in 107 cases
表2. 107例超声心动图、BNP资料比较
注:*与I组比较,p ≤ 0.05;#与I组、II组比较,p ≤ 0.05.。
以107例为分析样本,E/Ea与BNP呈正相关,BNP与LVEF、E/Ea与LVEF则呈负相关(图2~4),在I组中也基本保持了这样的相关关系;而在II组、III组中,不论是E/Ea与BNP、BNP与LVEF,还是E/Ea与LVEF之间均未呈现明显的线性相关,见表3。
Table 3. Correlative comparison among the parameters of echocardiography and BNP in 107cases
表3. 107例超声心动图、BNP参数各组的相关性比较

Figure 2. Correlation of BNP and E/Ea
图2. BNP与E/Ea的相关图

Figure 3. Correlation of LVEF and BNP
图3. LVEF与BNP相关图
4. 讨论
心力衰竭是包括冠心病在内的多数器质性心脏病患者中常见的危重症,主要表现为心脏收缩及/或舒张功能障碍,不能排出足量的血液以满足机体代谢需要的一种病理状态。根据基本的心脏病变、临床表现和实验室检查,心衰一般不难作出诊断,但是,不论收缩性或舒张性功能障碍引起的心衰均可表现为
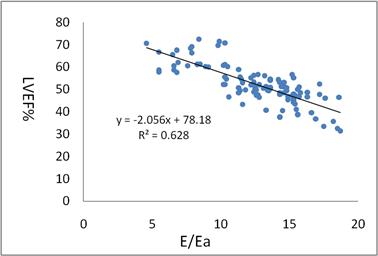
Figure 4. Correlation of LVEF and E/Ea
图4. LVEF与E/Ea相关图
体循环和/或肺循环淤血,从症状和体征上难以区别二者 [4]。从本组107例的检查结果看,在年龄、性别和基础病变基本相同的情况下,随着左心室功能不全加重,相应于LVEF测值的降低,可定量评定心衰进程和判断预后的BNP因心室扩张、心肌应力增加迅速合成释放入血而水平升高 [5] [6],提示左心室舒张末期充盈压(LVDP)的变化E/Ea也有明显的增大,两者均与LVEF呈负性相关(表1~3,图2~4),表明冠心病患者可同时存在心脏收缩和舒张功能损伤。
在LVEF测定正常的I组,其平均E/Ea为12.8 ± 4.5,高于正常人群E/Ea < 8的水平 [7],其变化与BNP、LVEF呈线性相关,说明在左心室整体收缩尚未出现异常时便可能存在局部或整体舒张功能减退的变化引起了LVDP的升高;而该组既反映左室收缩功能障碍、又可反映左室舒张功能障碍的BNP平均值达148.6 ± 34.8 ng/L,较临床作为常规排除急性心衰切点的BNP < 100 ng/L水平高,也与冠心病常出现节段性局部室壁功能异常的病理生理特点相符合,提示尽管DTEV延长和TDIe减低没有III组、II组明显,也有着年龄、性别和体重对E/Ea和BNP测量的干扰,但仍预示着该组患者有着舒张功能障碍加重的风险 [4] [5] [7]。
II组患者的LVEF轻度减低,舒张功能指标及BNP与I组即有差异,有着射血分数正常的心力衰竭(HFNEF或HF-pEF)的特点,升高的E/Ea表明左室处在必须用提高左室充盈压的途径来获得正常的心室充盈和心搏量的一种代偿状态,但该组病例的BNP、E/Ea并没有呈现出随着LVEF减低而升高的线性相关关系,提示左心室收缩功能轻度下降或近乎正常LVEF的冠心病患者的舒张功能即可有明显障碍,与Morris [8] 等观察的HFNEF患者的左心室心肌收缩、舒张做功能力降低、心功能分级高、心输出量减低及左心室充盈压升高的结果相符。III组的左心室扩大、容量负荷增加、BNP和E/Ea升高明显,有与LVEF变化线性相关的趋势,却并不显著,与I组和全部107例的结果显示不一致,推测可能与Ⅲ组样本量较少有关,但异常升高的BNP、E/Ea仍不失为该组病例心功能不全较为严重的反映 [9]。
基于本组资料的分析表明,在较大的样本中E/Ea与LVEF及BNP表现出较为明确的线性相关,但也存在着E/Ea的变化程度与LVEF不一致的情况,除了受到样本大小、病史背景差异、心室负荷和E/Ea主要反应左心室长轴功能变化等因素的影响外,也说明冠心病患者可存在着左心室收缩障碍与舒张功能减低程度不一致或非同步性,需要结合患者临床和相关实验室检查如BNP等加以综合判断 [10]。
文章引用
贺 声,刘英明,李 馨,刘秋颖,任 贺. 冠心病患者不同左心室射血分数二尖瓣口E/Ea的观测意义
Significance of Mitral E/Ea Estimation in Cases of Coronary Heart Disease with Different Left Ventricular Ejection Fractions[J]. 医学诊断, 2020, 10(01): 13-19. https://doi.org/10.12677/MD.2020.101003
参考文献
- 1. Galderisi, M. (2011) Diagnosis and Management of Left Ventricular Diastolic Dysfunction in the Hypertensive Patient. American Journal of Hypertension, 24, 507-517. https://doi.org/10.1038/ajh.2010.235
- 2. Kadappu, K.K. and Thomas, L. (2015) Tissue, Doppler Imaging in Echocardiography: Value and Limitations. Heart, Lung and Circulation, 24, 224-233. https://doi.org/10.1016/j.hlc.2014.10.003
- 3. Pugliese, N.R., Fabiani, J., Carrubba, S., et al. (2017) Classification and Prognostic Evaluation of Left Ventricular Remodeling in Patients with Asymptomatic Heart Failure. The American Journal of Cardiology, 119, 71-77.https://doi.org/10.1016/j.amjcard.2016.09.018
- 4. Pernot, M., Lee, W.N., Bel, A., et al. (2016) Shear Wave Imaging of Passive Diastolic Myocardial Stiffness: Stunned versus Infarcted Myocardium. JACC: Cardiovascular Imaging, 9, 1023-1030. https://doi.org/10.1016/j.jcmg.2016.01.022
- 5. Hinderliter, A.L., Blumenthal, J.A., O’Conner, C., et al. (2008) Independent Prognostic Value of Echocardiography and N-Terminal Pro-B-Type Natriuretic Peptide in Patients with Heart Failure. American Heart Journal, 156, 1191-1195. https://doi.org/10.1016/j.ahj.2008.07.022
- 6. McGrady, M., Reid, C.M., Shiel, L., et al. (2013) NT-ProB Natriuretic Peptide, Risk Factors and Asymptomatic Left Ventricular Dysfunction: Results of the Screen Evaluation of the Evolution of New Heart Failure Study (SCREEN-HF). International Journal of Cardiology, 169, 133-168. https://doi.org/10.1016/j.ijcard.2013.08.089
- 7. Desai, C.S., Colangeno, L.A., Liu, K., et al. (2013) Prevalence, Prospective Risk Markers, and Prognosis Associated with the Present of Left Ventricular Diastolic Dysfunction in Young Adults: The Coronary Artery Risk Development in Young Adults Study. American Journal of Epidemiology, 177, 20-32. https://doi.org/10.1093/aje/kws224
- 8. Morris, D.A., Boldt, L.H., Eichst, H., et al. (2012) Myocardial Systolic and Diastolic Performance Derived by 2-Dimensional Speckle Tracking Echocardiography in Heart Failure with Normal Left Ventricular Ejection Fraction. Circulation: Heart Failure, 5, 610-620. https://doi.org/10.1161/CIRCHEARTFAILURE.112.966564
- 9. Shah, K.B., Kop, W.J., Christenson, R.H., et al. (2009) Natriuretic Peptides and Echocardiography in Acute Dyspnoea: Implication of Elevated Levels with Normal Systolic Function. European Journal of Heart Failure, 11, 659-567. https://doi.org/10.1093/eurjhf/hfp075
- 10. Caraso, S., Williams, L.K., Hazanov, Y., et al. (2016) Comparision of Echocardiographic Parameters between Pre-Clinical and Clinical Advanced Diastolic Dysfunction Patients. International Journal of Cardiology, 224, 165-169.https://doi.org/10.1016/j.ijcard.2016.09.023
