Hans Journal of Ophthalmology
Vol.
08
No.
04
(
2019
), Article ID:
33281
,
7
pages
10.12677/HJO.2019.84022
Non-Open Sky Penetrating Keratoplasty Combined with Phacoemulsification and Intraocular Lens Implantation
Yong Yao1,2*, Ye Yuan2#, Yueting Ma1, Guanglin Chen1,3, Yingying Su1, Xi Wu1
1Department of Cornea and Ocular Surface, Joint Shantou International Eye Center of Shantou University and The Chinese University of Hong Kong, Shantou Guangdong
2 Department of Cornea and Ocular Surface, C-MER Shenzhen Dennis Lam Eye Hospital, Shenzhen Guangdong
3 Department of Cornea and Ocular Surface, Dongguan Aier Eye Hospital, Dongguan Guangdong

Received: Nov. 13th, 2019; accepted: Nov. 27th, 2019; published: Dec. 4th, 2019

ABSTRACT
Purpose: To introduce a innovative triple keratoplasty of non-open sky penetrating corneal transplantation combined with cataract phacoemulsification and intraocular lens implantation, and evaluate its clinical effect and complications. Methods: Prospective non-controlled clinical study. Non-open sky penetrating corneal transplantation combined with phacoemulsification and intraocular lens implantation was performed in 17 patients (17 eyes) with keratopathy complicated with cataract. The primary pathogenesis, surgical methods, postoperative vision, postoperative astigmatism, loss of corneal endothelial cells, corneal rejection and other complications were analyzed. Results: The average age of the 17 patients with keratopathy complicated with cataract patients was 55.35 ± 11.66 years (range from 26 to 70 years), with 9 males and 8 females. Among them, Funchs corneal endothelium dystrophy complicated with cataract in 2 cases, corneal endothelium decompensation complicated with cataract in 5 cases, corneal leukoplakia com- plicated with cataract in 7 cases, herpes simplex keratitis complicated with cataract in 2 cases, and corneal graft failure complicated with cataract in 1 case. All operations were performed by the same physician. The average follow-up time was 17.47 ± 8.11 months (range from 7 to 36 months). Preoperative visual acuity (BCVA) was LP to counting fingers/50 cm. The median postoperative visual acuity (BCVA) was 0.20 (range from 0.05 to 0.5). The Median astigmatism after surgery was 1.75D (range from 0.75D to 4.25D). Intraoperative posterior capsular rupture occurred in 1 case and the intraocular lens was implanted into the ciliary sulcus (1 case, 5.9%). All other intraocular lenses were implanted into the pouch (16 cases, 94.1%). The Endothelial cell loss rate was 30.6% (Corneal endothelial cell count preop/postop: 2316.88 ± 167.26/1607.82 ± 228.45 cell/mm2). During the follow-up period of 6-36 months, 15 eyes had clear corneal grafts and the graft transparency rate was 88.2%. Corneal graft rejection occurred in 1 case (5.9%) and neovasculari- zation occurred in 1 case (5.9%). One patient (5.9%) had delayed corneal epithelialization and was cured by corneal bandages and autologous serum. No other complications occurred. Conclusion: Non-open sky penetrating corneal transplantation combined with cataract phacoemulsification and intraocular lens implantation is a safe and effective innovative triple keratoplasty method. It can be used as one of the options for the treatment of keratopathy complicated with cataract. Relevant surgical skills can reduce intraoperative complications.
Keywords:Corneal Transplantation, Cataract Phacoemulsification, Artificial Crystal Implant, Triple Surgery
非开天窗穿透性角膜移植联合白内障超声乳化及人工晶体植入术
姚勇1,2*,袁野2#,马月庭1,陈冠麟1,3,苏莹莹1,吴熙1
1汕头大学·香港中文大学联合汕头国际眼科中心角膜与眼表科,广东 汕头
2深圳希玛林顺潮眼科医院角膜与眼表科,广东 深圳
3东莞爱尔眼科医院角膜与眼表科,广东 东莞

收稿日期:2019年11月13日;录用日期:2019年11月27日;发布日期:2019年12月4日

摘 要
目的:介绍一种新的非开天窗穿透性角膜移植联合白内障超声乳化及人工晶体植入的三联手术,并初步评价其临床效果及并发症。方法:前瞻性非对照临床研究,角膜病变合并白内障进行非开天窗穿透性角膜移植联合白内障超声乳化及人工晶体植入术17例(17只眼)。分析其手术原因,手术方法,术后视力,术后散光,角膜内皮细胞丢失,角膜排斥及其他并发症。结果:17例角膜病变合并白内障患者,其中男9例,女8例。年龄最小26岁,最大70岁,平均年龄55.35 ± 11.66岁。其中Funchs角膜内皮营养不良合并白内障2例,角膜内皮失代偿合并白内障5例,角膜白斑合并白内障7例,单纯疱疹病毒性角膜炎合并白内障2例,角膜移植术后排斥合并白内障1例。所有患者由同一医师操作行非开天窗穿透性角膜移植联合白内障超声乳化及人工晶体植入术。随访时间最短7月,最长36月,平均随访时间17.47 ± 8.11月。术前视力(BCVA)均为LP到数指/50 cm。术后视力(BCVA)中位数0.20 (范围:0.05~0.5)。术后散光中位数1.75D (范围:0.75D~4.25D)。术中1例后囊破裂发生,人工晶状体植入睫状沟(1例,5.9%),其余所有人工晶状体均植入囊袋(16例,94.1%)。术前角膜内皮细胞计数为2316.88 ± 167.26 (cell/mm2);术后6月角膜内皮细胞计数为1607.82 ± 228.45 (cell/mm2);内皮细胞丢失率为30.6%。在6~36月的随访中,15只眼术后角膜移植片透明,植片透明率88.2%。1例(5.9%)发生角膜移植排斥,1例(5.9%)发生角膜新生血管化。1例(5.9%)角膜上皮化延迟,经角膜绷带镜及自体血清治疗痊愈。未发生其他并发症。结论:非开天窗穿透性角膜移植联合白内障超声乳化及人工晶体植入术,是安全有效的新的三联手术方法,可以作为治疗角膜病变合并白内障的选择之一。掌握相关手术技巧,可以减少术中并发症。
关键词 :角膜移植,白内障超声乳化,人工晶体植人,三联手术

Copyright © 2019 by author(s) and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


1. 前言
角膜病变合并白内障是临床上经常遇到的问题,手术方式的选择也各不相同。许多医师倾向于先行穿透性角膜移植(penetrating keratoplasty, PKP),二期再行白内障超声乳化联合人工晶状体植入手术。其理由是角膜移植术后角膜曲率不稳定且不规则,角膜缝线拆除后再二期行白内障超声摘出及人工晶状体植入,可以精确测算人工晶状体的度数以减少术后的屈光误差 [1]。但再次白内障手术,容易导致角膜内皮细胞的损伤,手术刺激的炎症反应也容易导致角膜植片排斥,而且多次手术也给病人增加了额外的经济和精神负担。Taylor [2] 最早报道了应用PKP联合白内障摘出及人工晶状体植入的方法,即三联手术来治疗合并白内障的角膜病变患者。这种三联手术方法需要先将病变角膜去除,在开窗条件下行白内障摘出及人工晶状体植入,然后将角膜植片缝合于植床上。由于避免了角膜植片二次手术遭受损伤,并能快速恢复视力,这种三联术式一度成为角膜病变合并白内障的主流手术。但是,开天窗下PKP联合白内障摘除及人工晶状体植入,不容易环行撕囊,容易发生后囊破裂玻璃体脱出,皮质不容易清除干净,人工晶体不易植入到囊袋内。然而,最大的缺点在于发生暴发性脉络膜上腔出血的几率明显增加,这种严重的并发症对于眼球来说是毁灭的。近年来,有作者报道稳定前房的穿透性角膜移植及联合白内障摘出和人工晶体植入术,可以减少暴发性脉络膜上腔出血的发生,且不增加角膜内皮丢失率 [3] [4] [5]。然而这种方法能否改良后用于联合白内障超声乳化的三联手术,还少有人进行尝试。此研究的目的是介绍一种新的非开天窗穿透性角膜移植联合白内障超声乳化及人工晶体植入的三联手术方法,并初步评价其临床效果及并发症。
2. 材料和方法
前瞻性、非对照临床研究。本研究遵循赫尔辛基宣言,并获得了本中心伦理委员会的审核同意。对象为2013年1月至2018年10月在汕头大学·香港中文大学联合汕头国际眼科中心收治的角膜病变合并白内障患者。所有患者纳入前均书面告知并签署知情同意书。共纳入17例角膜病变合并白内障患者,其中男9例,女8例。年龄最小26岁,最大70岁,平均年龄55.4岁。入选标准为:1、诊断为角膜病变合并白内障需要光学性角膜移植术;2、年龄在18岁至70岁之间,同意进入本研究并且承诺能配合随访至少6月。排除标准为:1、年龄在18岁以下或70岁以上者;2、对本试验中任何药物及其他成分过敏者;3、有干燥综合征,眼部外伤史或其他眼部手术史者;4、有眼睑结构异常如内外翻、倒睫、睑闭合不全;5、有全身炎症或眼部感染性疾病,如慢性泪囊炎,感染性结膜炎或活动性角膜炎者;6、合并其他眼病如青光眼,葡萄膜炎,视网膜脱离,甲状腺相关眼病等者;7、既往合并有严重心脑血管、肝、肾、内分泌和造血系统疾病者;8、瘢痕体质者;9、有精神损伤障碍病史,或智能缺陷,无法遵循试验要求者。所有的手术操作均由同一医生完成。术后抗炎、抗排斥及促进角膜上皮生长用药同常规PKP及白内障手术。所有患者术前、术后检查视力、眼压、裂隙灯检查、角膜荧光素钠染色,术前及术后6月角膜内皮细胞计数检查。观察时间为治疗前、术后7 (±2)、术后30 (±4)、术后90 (±7)、术后180 (±14)、术后360 (±14)天复查。随访至少半年,记录并观察比较术前术后视力,术后散光,角膜内皮细胞丢失,角膜排斥及手术并发症。
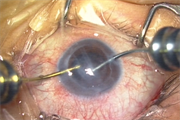
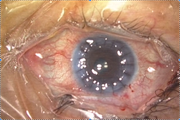
手术方法(见图1):
 (a)
(a)
 (b)
(b)
 (c)
(c)
 (d)
(d)
 (e)
(e)
 (f)
(f)
 (g)
(g)
 (h)
(h)
Figure 1. Surgical steps diagram ((a): trephine demarcation; (b): excision of about 80% - 90% lesions of the cornea; (c): dye the anterior capsule and complete CCC; (d): cataract phacoemulsification; (e): bimunal I/A suction cortex; (f): implant the intraocular lens into the pouch; (g): cut off the interrupted suture and extract the remaining lesions cornea; (h): suture the corneal graft)
图1. 手术步骤示意图((a):环钻划界;(b):切除约80%~90%左右病变角膜;(c):前囊染色,完成CCC;(d):行白内障超声乳化;(e):Bimunal双手I/A吸除皮质;(f):植入人工晶体于囊袋内;(g):剪刀剪断病变角膜的间断缝线,将剩余的病变角膜抽出;(h):10-0尼龙线间断缝合角膜植片)
1) 2%利多卡因及5%布比卡因等量混合行球后麻醉,局部按压降低眼压;
2) 环钻划界,钻取并切除约80-90%左右病变角膜(图1(a),图1(b));
3) 滴BSS以观察剩余中央病变角膜的浑浊情况及前房的可视性,必要时可根据情况再次剖切;
4) 常规透明角膜白内障手术切口,前房内注入台盼蓝前囊染色,完成CCC及水分离、水分层,必要时可用23G或25G导光辅助照明(图1(c));
5) 行白内障超声乳化,为减少后囊破裂的几率,必要时可前房内超声乳化(图1(d));
6) Bimunal双手I/A吸除皮质,植入人工晶体于囊袋内,卡米可林缩瞳,10-0尼龙线缝合白内障角膜切口(图1(e),图1(f));
7) 15度刀沿环钻边缘刺穿剩余病变角膜,一边用剪刀剪切,一边用10-0尼龙线缝合,每个象限一针共4针;
8) 病变角膜上注射粘弹剂以保护角膜植片内皮,将角膜植片放于植床,10-0尼龙线间断缝合4针;
9) 再次注射粘弹剂保护角膜植片内皮细胞,剪刀剪断病变角膜的间断缝线,将剩余的病变角膜抽出(图1(g));
10) 10-0尼龙线间断缝合角膜植片,I/A抽吸前房粘弹剂,BSS形成前房(图1(h))。
3. 结果
17例角膜病变合并白内障患者,其中男9例,女8例。年龄最小26岁,最大70岁,平均年龄55.35 ± 11.66岁。其中Funchs角膜内皮营养不良合并白内障2例,角膜内皮失代偿合并白内障5例,角膜白斑合并白内障7例,单纯疱疹病毒性角膜炎合并白内障2例,角膜移植术后排斥合并白内障1例。所有患者由同一医师操作行非开天窗穿透性角膜移植联合白内障超声乳化及人工晶体植入术。随访时间最短7月,最长36月,平均随访时间17.47 ± 8.11月。术前视力(BCVA)均为LP到数指/50 cm。术后视力(BCVA)中位数0.20 (范围:0.05~0.5)。术后散光中位数1.75D (范围:0.75D~4.25D)。术中1例后囊破裂发生,人工晶状体植入睫状沟(1例,5.9%),其余所有人工晶状体均植入囊袋(16例,94.1%)。术中无任何其他并发症,包括暴发性脉络膜上腔出血、晶状体损伤、虹膜损伤等。术前角膜内皮细胞计数为2316.88 ± 167.26 (cell/mm2);术后6月角膜内皮细胞计数为1607.82 ± 228.45 (cell/mm2);内皮细胞丢失率为30.6%。在6~36月的随访中,15只眼术后角膜移植片透明,植片透明率88.2%。1例(5.9%)发生角膜移植排斥,经局部类固醇和他克莫司治疗后逆转;1例(5.9%)发生角膜新生血管化;1例(5.9%)角膜上皮化延迟,经角膜绷带镜及自体血清治疗痊愈。未发生其他并发症。术后未发生继发性青光眼、眼内炎、角膜感染溃疡、创口裂开等缝合相关并发症(见表1)。
Table 1. Patient information and examination results
表1. 病人资料和检查结果
4. 讨论
暴发性脉络膜上腔出血是PKP手术术中最危险的并发症,严重者可以导致眼球萎缩,发生率大约0.05%左右 [6]。主要是病变角膜切除与角膜植片缝合之间的过程中,眼球完全暴露于空气中,手术无法控制眼压,患者任何紧张、血压升高、憋气或咳嗽都可能导致眼内容物脱出,甚或爆发性脉络膜上腔出血等严重并发症。常规的三联手术眼球完全暴露于空气中的时间更长,并且在开天窗条件下有前后房压力差,撕囊裂向周边,娩核时后囊破裂明显增加,更增加了玻璃体脱出和暴发性脉络膜上腔出血等严重并发症的风险。我们方法的主要优点是在完全密闭条件下进行超声乳化白内障手术,无论是撕囊、核乳化、I/A、还是人工晶体植入的过程,都和常规白内障超声乳化过程无异。此外,在完成白内障超声乳化及人工晶体植入后,我们通过边剪切边缝合的方法 [3],构建了一个非开天窗系统,避免了眼球完全暴露于空气中,同时维持对前房及人工晶体的均衡的压力,所有这些因素都有助于降低手术风险和减少与开天窗手术相关的并发症,从本质上改变了手术的安全系数。
连续环形撕囊术(continuous curvilinear capsulorhexis, CCC)是超声乳化白内障手术的关键步骤之一。CCC对于三联手术的安全性及效率更加重要。完整的CCC可安全抽吸皮质以减少后囊破裂及术后后囊混浊发生的几率、准确地放置人工晶状体于囊袋内。在三联手术中应用台盼蓝进行囊膜染色后撕囊,能够提高撕囊完成率,降低后囊破裂机会,且未发现与台盼蓝有关的不良反应 [7] [8]。如果剩余病变角膜混浊,在囊膜染色后仍然窥视不清,可以应用23G或者25G眼内光纤后部反光照明法下行CCC,这种方法有助于提高对比度,顺利完成CCC。我们的观察对象中就有2例使用这种技术后才顺利完成CCC。另外,可以应用吊顶灯 [9] 或者25G眼内光纤后部反光照明法 [10] 在后囊破裂时,有利于充分清除脱出到前房的玻璃体,并将人工晶体准确植入到睫状沟。对于核乳化步骤,在前房可视性尚可的情况下,可以同常规白内障超声乳化技术,不过我们建议设置低吸力及适当的超声能量,可以减少晶状体核乳化过程中出现的并发症。如果前房可视性差或者核比较硬,可以将核快吸到或者手法旋拨到前房内,再超声乳化。因为这种情况下我们不用再考虑保护病变角膜的内皮细胞,而且可以最大程度的减少后囊破裂等并发症。
与之前报道方法稍有不同,我们用边剪切边缝线的方法缝线,替代残留少量剩余角膜不完全切穿的方法。我们的角膜内皮丢失率,手术并发症与之比较,并没有明显差异。改良后的方法可能更加简便易行。传统的PKP角膜内皮丢失率大约25.7%到40.9%之间 [11] [12] [13]。我们的三联手术方法内皮丢失率为30.6%,与之比较并没有明显增加。我们认为可能和整个白内障超声乳化及人工晶体植入过程中,并没有接触植片角膜,以及在病变角膜抽出前粘弹剂对角膜内皮细胞的保护有关。二次分期手术的患者需要等待至少12~18个月以上再行白内障手术,而且两次面临爆发性脉络膜上腔出血、角膜植片内皮损伤及眼内炎的风险。角膜移植术后行白内障超声乳化手术所造成的角膜内皮损失率明显增高,可能会引起角膜植片排斥及角膜失代偿 [14]。三联手术与单纯PKP角膜植片衰竭及排斥的风险相当,我们的结果与Green及Oie等 [15] [16] 报道相近。
我们的研究尽管是前瞻性,但是收集的病例数较少,病因和随访时间不一,研究跨度时间长,年龄跨度大,且是单中心、非对照的临床研究。未来我们需要扩大样本量,进行多中心、前瞻、对照的临床研究,以获得更加科学的结果。
总之,非开天窗穿透性角膜移植联合白内障超声乳化及人工晶体植入术,可以快速的恢复视力,且不增加手术的风险。掌握相关手术技巧,可以减少术中特别是爆发性脉络膜上腔出血及眼内容物脱出等并发症的风险。可以作为治疗角膜病变合并白内障的一种选择。
致谢
本项目由广东省科学技术研究基金(A2017486)支持。
文章引用
姚 勇,袁 野,马月庭,陈冠麟,苏莹莹,吴 熙. 非开天窗穿透性角膜移植联合白内障超声乳化及人工晶体植入术
Non-Open Sky Penetrating Keratoplasty Combined with Phacoemulsification and Intraocular Lens Implantation[J]. 眼科学, 2019, 08(04): 134-140. https://doi.org/10.12677/HJO.2019.84022
参考文献
- 1. Chen, W., Ren, Y., Zheng, Q., et al. (2014) Stabilized Triple Procedure for Management of Coexisting Corneal Opacity and Cataract. Journal of Cataract & Refractive Surgery, 40, 1966-1970.
https://doi.org/10.1016/j.jcrs.2014.09.031 - 2. Yang, S., Wang, B., Zhang, Y., et al. (2017) Evaluation of an Interlaced Triple Procedure: Penetrating Keratoplasty, Extracapsular Cataract Extraction, and Non-Open-Sky Intraocular Lens Implantation. Medicine, 96, e7656.
https://doi.org/10.1097/MD.0000000000007656 - 3. Tan, D., Dart, J., Holland, E. and Kinoshita, S. (2012) Corneal Transplantation. The Lancet, 379, 1749-1761.
https://doi.org/10.1016/S0140-6736(12)60437-1 - 4. Yamamoto, N., Ozaki, N. and Murakami, K. (2005) Trypan-Blue- and Endoillumination-Assisted Phacoemulsification in Eyes with Vitreous Hemorrhage during Combined Cataract and Vitreous Surgery. Ophthalmologica, 219, 338-344.
https://doi.org/10.1159/000088375 - 5. Nagashima, T., Yuda, K. and Hayashi, T. (2019) Comparison of Trypan Blue and Brilliant Blue G for Staining of the Anterior Lens Capsule during Cataract Surgery: Short-Term Results. International Ophthalmology, 39, 33-39.
https://doi.org/10.1007/s10792-017-0779-9 - 6. Yokokura, S., Hariya, T., Uematsu, W., et al. (2015) Efficacy of Chandelier Illumination for Combined Cataract Operation and Penetrating Keratoplasty. Cornea, 34, 275-278.
https://doi.org/10.1097/ICO.0000000000000319 - 7. Rosen, E.S. (1998) Combined or Sequential Keratoplasty and Cataract Surgery? Journal of Cataract & Refractive Surgery, 24, 1283-1284.
https://doi.org/10.1016/S0886-3350(98)80214-9 - 8. Yokokura, S., Hariya, T., Kobayashi, W., et al. (2017) Twenty-Nine-Gauge Dual-Chandelier Retroillumination for the Non-Open-Sky Continuous Curvilinear Capsulorhexis in the Penetrating Keratoplasty Triple Procedure. Journal of Cataract & Refractive Surgery, 43, 305-308.
https://doi.org/10.1016/j.jcrs.2017.02.004 - 9. Acar, B.T., Utine, C.A., Acar, S., et al. (2011) Endothelial Cell Loss after Phacoemulsification in Eyes with Previous Penetrating Keratoplasty, Previous Deep Anterior Lamellar Keratoplasty, or No Previous Surgery. Journal of Cataract & Refractive Surgery, 37, 2013-2017.
https://doi.org/10.1016/j.jcrs.2011.05.033 - 10. Taylor, D.M. (1976) Keratoplasty and Intraocular Lenses. Journal of Ophthalmic Surgery, 7, 31-42.
- 11. Borderie, V.M., Sandali, O., Bullet, J., et al. (2012) Long-Term Results of Deep Anterior Lamellar versus Penetrating Keratoplasty. Ophthalmology, 119, 249-255.
https://doi.org/10.1016/j.ophtha.2011.07.057 - 12. Chen, W., Ren, Y., Zheng, Q., Li, J.Y. and Waller, S. (2013) Securing the Anterior Chamber in Penetrating Keratoplasty: An Innovative Surgical Technique. Cornea, 32, 1291-1295.
https://doi.org/10.1097/ICO.0b013e31829954c5 - 13. Kim, E.C. and Kim, M.S. (2010) A Comparison of Endothelial Cell Loss after Phacoemulsification in Penetrating Keratoplasty Patients and Normal Patients. Cornea, 29, 510-515.
https://doi.org/10.1097/ICO.0b013e3181c11e0e - 14. Green, M., Chow, A. and Apel, A. (2007) Outcomes of Combined Penetrating Keratoplasty and Cataract Extraction Compared with Penetrating Keratoplasty Alone. Clinical & Experimental Ophthalmology, 35, 324-329.
https://doi.org/10.1111/j.1442-9071.2007.01481.x - 15. Arslan, O.S., Ünal, M., Arici, C., et al. (2014) Novel Method to Avoid the Open-Sky Condition in Penetrating Keratoplasty- Covered Cornea Technique. Cornea, 33, 994-998.
https://doi.org/10.1097/ICO.0000000000000186 - 16. Oie, Y. and Nishida, K. (2017) Triple Procedure: Cataract Extraction, Intraocular Lens Implantation, and Corneal Graft. Current Opinion in Ophthalmology, 28, 63-66.
https://doi.org/10.1097/ICU.0000000000000337
NOTES
*通讯作者。
#第一作者。
