Advances in Clinical Medicine
Vol.
10
No.
07
(
2020
), Article ID:
36618
,
8
pages
10.12677/ACM.2020.107210
Diffuse Pulmonary Lymphangiomatosis: Report of Two Cases
Deng Pan1, Jinpeng Cong2, Fangfang Wang2, Wei Cheng2, Liyun Mi2, Haihong Gong2, Yunqing Chen3, Wencheng Yu2*
1Medical Department of Qingdao University, Qingdao Shandong
2Respiratory and Critical Care Medicine, The Affiliated Hospital of Qingdao University, Qingdao Shandong
3Pathology Department, The Affiliated Hospital of Qingdao University, Qingdao Shandong

Received: Jul. 1st, 2020; accepted: Jul. 15th, 2020; published: Jul. 22nd, 2020

ABSTRACT
Objective: To investigate the clinical features of 2 patients with diffuse pulmonary lymphangiomatosis. Methods: To explore the clinical data of 2 cases of diffuse lymphangiomatosis admitted to the respiratory and critical care medicine department of the Affiliated hospital of Qingdao university in 2018 and 2019 (case 1 was considered as lymphangiomatosis by surgical lung biopsy and case 2 was confirmed by radionuclide lymphography). Results: Case 1, male, 58 years old, was admitted to hospital due to “cough and expectoration for more than 2 months”. Enhanced chest CT of the patient showed extensive massive and slightly low-density shadows in the mediastinum. The pathological results of surgical lung biopsy indicated that: lymph nodes were found to show reactive hyperplasia and changes in the tissue, and a large number of vessels with different sizes were found to be consistent with angioma. Case 2, female, 42 years old, was admitted to hospital due to “cough and expectoration for more than 4 months”. Enhanced chest CT showed diffuse lesions in bilateral supraclavicular fossa, mediastinum, retroperitoneum and abdominal cavity. Nuclide imaging: systemic multiple patch, nodules, and mass of soft tissue density with different degree of imaging agent poly, consider possible sources of the lymphatic system. Conclusion: CT findings of DPL are mostly smooth thickening of bilateral pulmonary interlobular septum and bronchovascular interstitium, chylous pleural effusion and pleural thickening are common, mediastinal lymph node enlargement and mediastinal fat density can also be seen. Pathological biopsy is the gold standard of diagnosis.
Keywords:Diffuse Pulmonary Lymphangiomatosis, Pathology, Diagnosis

弥漫性肺淋巴管瘤病二例报告
潘登1,丛金鹏2,王芳芳2,成炜2,糜丽云2,巩海红2,陈云庆3,于文成2*
1青岛大学医学部,山东 青岛
2青岛大学附属医院,呼吸与危重症医学科,山东 青岛
3青岛大学附属医院,病理科,山东 青岛

收稿日期:2020年7月1日;录用日期:2020年7月15日;发布日期:2020年7月22日

摘 要
目的:探讨2例弥漫性肺淋巴管瘤病(DPL)患者的临床特点。方法:对2018年和2019年青岛大学附属医院呼吸与危重症医学科收治的2例淋巴管瘤病的患者(例1经外科肺活检考虑为淋巴管瘤病,例2经核素淋巴显像证实)的临床资料进行回顾性分析。结果:例1 男,58岁,因“咳嗽、咳痰2月余”入院。患者行胸部增强CT示纵隔内广泛团块状略低密度影,外科肺活检病理结果提示:淋巴结呈反应性增生改变,另见多量大小不等的脉管,符合脉管瘤。例2 女,42岁,因“咳嗽、咳痰4月余”入院。患者行胸部增强CT示双侧锁骨上窝、纵隔内、腹膜后及腹腔弥漫性病变。后核素淋巴显像显示全身多发斑片、结节及肿块状软组织密度影,来源于淋巴系统。结论:DPL的CT表现多为双肺小叶间隔和支气管血管间质的光滑性增厚,乳糜性胸腔积液和胸膜增厚常见,也可见纵隔淋巴结肿大和纵隔脂肪密度增加。病理活检是诊断的金标准。
关键词 :弥漫性肺淋巴管瘤病,病理学,诊断

Copyright © 2020 by author(s) and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/


1. 引言
弥漫性肺淋巴管瘤病(Diffuse Pulmonary Lymphangiomatosis, DPL)主要影响肺和胸膜。肺损伤的病理报告很少,伴有肺外淋巴结和周围软组织的弥漫性受累 [1]。认识异常扩张或重叠的淋巴管的特征分布是正确诊断该病的关键 [2],研究表明与儿童相比,成人DPL侵袭性较小、预后较好 [4]。有报道称手术是治疗相对局限的DPL的有效方法 [3]。我们对青岛大学附属医院呼吸与危重症医学科2018年4月及2019年3月收治的2例DPL患者(均已获得两例患者的知情同意)的临床资料进行回顾性分析,旨在提高临床医师对此病的认识,积累更多的临床经验。
2. 病历资料
例1 男,58岁,因“咳嗽、咳痰2月余”入院。胸部增强CT示双肺片状、斑片、条索影,双侧胸腔积液,心包积液,纵隔内广泛团块状略低密度影,增大淋巴结可能性大,淋巴瘤、转移瘤待排除,上纵隔后部偏左侧团块状软组织密度影并钙化。排除支气管镜术前禁忌症后于2018年4月28日行支气管镜检查:左主支气管及下叶黏膜肿胀增厚,呈纵行生长,表面散在结节样新生物,管腔通畅,右侧各级支气管管腔通畅,黏膜充血肿胀,未见新生物,过程顺利。术后咳大量橘红色浆液性痰,转入胸外科并行急诊胸腔镜辅助开胸探查 + 纵隔病损切除 + 纵隔胸膜切开引流 + 胸导管结扎 + 胸膜腔粘连松解术。病理结果回示:(胸膜)少许胶原化的纤维结缔组织呈慢性活动性炎,局灶伴退变坏死改变。(纵隔)送检组织内见4枚淋巴结呈反应性增生改变,另见多量大小不等的脉管,符合脉管瘤。既往“肝硬化、肝性脑病”病史20余年,反复出现意识障碍。否认家族遗传史。
【体格检查】T 36.1℃,P 100次/分,R 23次/分,Bp 135/90 mmHg,神志清,浅表淋巴结未触及肿大,口唇无紫绀,左侧叩诊清音,右下肺叩诊浊音,右下肺呼吸音低,右上肺可闻及哮鸣音,左下肺可闻及吸气末湿啰音,心律齐,各瓣膜听诊区未闻及病理性杂音,腹软,无压痛及反跳痛,肝脾肋下未触及,双下肢无水肿,无杵状指、趾。
【血清学】血常规:白细胞4.50 (正常值3.5~9.5) × 109/L,中性粒细胞2.07 (正常值1.8~6.3) × 109/L,中性粒细胞百分率46.0 (正常值40~75)%,淋巴细胞1.36 (正常值1.1~3.2) × 109/L,单核细胞0.54 (正常值0.1~0.6) × 109/L,血红蛋白141 (正常值130~175) g/L,血小板171 (正常值125~350) × 109/L,网织红细胞百分率为2.32 (正常值0.5~1.5)%,C-反应蛋白(CRP) 2.69 (正常值0~5) mg/L。血生化:总蛋白56.66 (正常值65~85) g/L,白蛋白24.21 (正常值40~55) g/L,总胆红素37.76 (正常值3~22) umol/L,直接胆红素16.03 (正常值0~8) umol/L,ALT32.0 (正常值7~40) U/L,AST50.0 (正常值13~35) U/L,碱性磷酸酶187.0 (正常值50~135) U/L,总胆汁酸97.70 (正常值0~12) umol/L。血凝常规:抗凝血酶III38.00 (正常值80~140)%,D-二聚体1620.0 (正常值0~500) ng/ml。尿常规、大便常规、CK + CKMB测定、电解质检测、血糖分析、血脂、血钙磷镁检测、均未见明显异常。风湿四项、ENA谱、抗中性粒细胞胞浆抗体(ANCA)均阴性,抗核抗体(ANA)阳性(+)。肺癌相关肿瘤标记物中癌胚抗原为5.27 (正常值0~3.4) ng/ml,糖类抗原125为56.17 (正常值0~35) U/mL,余正常。动脉血气分析(未吸氧):pH 7.47 (正常值7.35~7.45),氧分压67 (正常值83~108) mmHg,二氧化碳分压37 (正常值35~48) mmHg,实际碳酸氢盐26.90 (正常值21~28) mmol/L,氧饱和度95.70 (正常值95~98)%。血氨171.00 (正常值18~72) umol/L。降钙素原0.069 (正常值 < 0.05) ng/mL。
【病原学】结核T-SPOT检测、痰培养、痰查抗酸杆菌均为阴性。
【气管镜及外科手术】左主支气管及下叶黏膜肿胀增厚,呈纵行生长,表面散在结节样新生物,管腔通畅,右侧各级支气管管腔通畅,黏膜充血肿胀,未见新生物,过程顺利。术后咳大量橘红色浆液性痰,转入胸外科并行急诊胸腔镜辅助开胸探查 + 纵隔病损切除 + 纵隔胸膜切开引流 + 胸导管结扎 + 胸膜腔粘连松解术。
【影像学检查】术前胸部CT (图1)示双肺片状、斑片、条索影,双侧胸腔积液,心包积液,纵隔内广泛团块状略低密度影,上纵隔后部偏左侧团块状软组织密度影并钙化。胸外科术后胸部CT如图2所示。
【病理学】如图3所示,(痰)涂片内未发现恶性肿瘤细胞;(气管镜后咳出物)涂片内未发现恶性肿瘤细胞,镜下为均质红染的蛋白样物伴中性粒细胞、淋巴细胞及组织细胞;(左支气管活检)少许支气管黏膜组织呈慢性炎;(左下叶灌洗)血性涂片内未发现恶性肿瘤细胞;(痰引流液组织)镜下少许粘液分泌物内见炎细胞、组织细胞,未见确切肿瘤成分。
【诊断】淋巴管瘤病(纵隔、肺、颈部)吸入性肺炎 肝硬化 肝性脑病
【治疗】入院后给予抗感染、降血氨、保肝对症支持治疗,排除支气管镜术前禁忌症后于2018年4月28日行支气管镜检查:左主支气管及下叶黏膜肿胀增厚,呈纵行生长,表面散在结节样新生物,管腔通畅,右侧各级支气管管腔通畅,黏膜充血肿胀,未见新生物。气管镜检查术中患者咳橘黄色浆液痰,紧急转入本院胸外科行急诊胸腔镜辅助开胸探查 + 纵隔病损切除 + 纵隔胸膜切开引流 + 胸导管结扎 + 胸膜腔粘连松解术。病理结果提示:(胸膜)少许胶原化的纤维结缔组织呈慢性活动性炎,局灶伴退变坏死改变。(纵隔)送检组织内见4枚淋巴结呈反应性增生改变,另见多量大小不等的脉管,符合脉管瘤。术后留置两根右侧胸腔引流管持续引流胸腔积液,转入重症医学科,分别于2018年05月18日、05月28日拔除两根胸腔置管,经上述治疗后患者症状改善,复查胸部CT (图2)较前好转,病情相对稳定,准予出院。随访患者目前病情稳定。
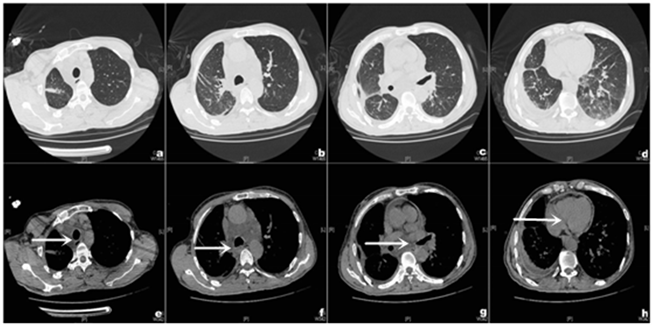
Figure 1. Chest routine scan (2018-04-26). (a)-(d) Multiple patches, plaques and striations of both lungs. (e)-(h) In the mediastinum, there was a mass of slightly lower density shadow and partial fusion. The posterior part of the upper mediastinum was to the left, showing a mass of soft tissue density shadow with a diameter of about 33 mm. Calcification was observed (arrow indicated the lesion location)
图1. 胸部CT平扫(2018-04-26)。(a)~(d) 双肺多发片状、斑片、条索影。(e)~(h) 纵隔内广泛团块状略低密度影,部分融合状,上纵隔后部偏左侧示团块状软组织密度影,直径约33 mm,内见钙化(箭头标注为病变位置)
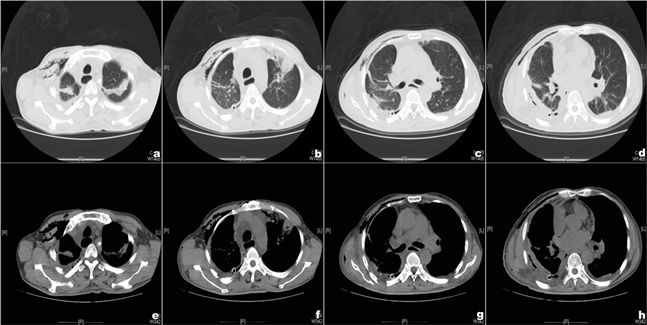
Figure 2. Chest routine scan (2018-05-07). (a)-(d) Multiple patches, plaques and striations of both lungs. Fluid density shadow was seen in bilateral pleural cavity, and the right pleural thickening was more obvious. (e)-(h) In mediastinum, the mass was slightly low density shadow, which was smaller than the previous range. The posterior part of the upper mediastinum was to the left, showing mass soft tissue density shadow and calcification
图2. 胸部CT平扫(2018-05-07)。(a)~(d) 双肺多发片状、斑片、条索影。双侧胸腔内见液性密度影,右侧胸膜增厚较明显。(e)~(h) 纵隔内广泛团块状略低密度影,较前范围减小,上纵隔后部偏左侧示团块状软组织密度影,内见钙化
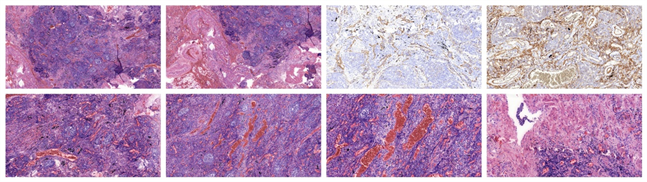
Figure 3. Pathological results: 5.0×, 5.0×, D2-40_20×, CD31_20×, 10.0×, 10.0×, 20.0×, 20.0× from top left to bottom right
图3. 病理结果:从左上至右下依次为5.0×,5.0×,D2-40_20×,CD31_20×,10.0×,10.0×,20.0×,20.0×
例2 女,42岁,2019-03-08因“咳嗽、咳痰4月余”入院。病程中患者行胸部增强CT示双侧锁骨上窝、纵隔内、腹膜后及腹腔弥漫性病变,右侧胸腔积液,甲状腺右叶内低密度影。该患者病程较长,既往“纵隔占位”病史16年,未明确诊断,无特殊诊治,“血小板减少”病史16年,血小板最低波动在20~31 × 109/L,14年前及9月前两次行剖宫产手术,14年前因“产后出血”输注血浆治疗,9月前因“产后出血”多次输注血小板、血浆、红细胞等,均无输血反应。右侧附件区2处软组织密度结节,较小者轻度代谢增高,SUVmax约3.6。
【体格检查】颈部对称,软,颈动脉搏动正常,右侧颈静脉怒张,气管居中,右侧甲状腺弥漫性肿大I度,无压痛,未闻及血管杂音。双肺呼吸音清,未闻及干湿性啰音,心界无扩大,律齐,各瓣膜听诊区未闻及病理性杂音,腹软,无压痛、反跳痛及肌紧张,肝脾未扪及,肝肾区无叩击痛,肠鸣音正常,生理反射存在,病理反射未引出,双下肢无水肿。
【血清学】血常规:白细胞9.15 (正常值3.5~9.5) × 109/L,中性粒细胞5.44 (正常值1.8~6.3) × 109/L,中性粒细胞百分率59.60 (正常值40~75)%,嗜酸细胞0.61 (正常值0.02~0.52) × 109/L,淋巴细胞2.54 (正常值1.1~3.2) × 109/L,单核细胞0.51 (正常值0.1~0.6) × 109/L,红细胞2.77 (正常值4.3~5.8) × 1012/L,血红蛋白83.00 (正常值130~175) g/L,血小板32.00 (正常值125~350) × 109/L。血生化:总蛋白63.58 (正常值65~85) g/L,白蛋白37.44 (正常值40~55) g/L,ALT6.0 (正常值7~40) U/L,AST12.0 (正常值13~35) U/L,碱性磷酸酶31.00 (正常值50~135) U/L,LDL (正常值1.9~3.2) 1.64 mmoL。血凝常规:纤维蛋白原1.13 (正常值1.7~4.7) g/L,凝血酶时间19.60 (正常值10~18) sec,D-二聚体为20790.00 (正常值0~500) ng/mL。尿常规:隐血3+,红细胞212.06 (正常值0~5) uL。大便常规、电解质检测、血糖分析未见明显异常。
【气管镜】因病人血小板最低波动在20~31 × 109/L,暂未予患者支气管镜检查。
【影像学检查】图4为2013年首次发现胸部CT异常,图5为本次入院时胸部CT。
【PET-CT】双肺门及纵隔内弥漫分布斑片、结节及肿块状软组织密度影,内见脂肪密度,包绕双肺动脉、气管、食管、心包,并沿支气管血管束向右肺蔓延,右肺中下叶支气管管腔狭窄,未见异常代谢;右侧胸腔积液;双侧颈后三角区、双侧锁骨上区、右侧胸大肌深部脂肪间隙内弥漫分布斑片及结节状软组织密度影,未见异常代谢。
【核素淋巴显像】如图6,全身多发斑片、结节及肿块状软组织密度影,不同程度显像剂浓聚,来源于淋巴系统可能性大。
【诊断】弥漫性淋巴管瘤病?贫血 血小板减少
【治疗】入院后完善相关检查,给予升血小板胶囊升血小板治疗,转至上级医院治疗,随访得知上级医院未给予特殊处理。
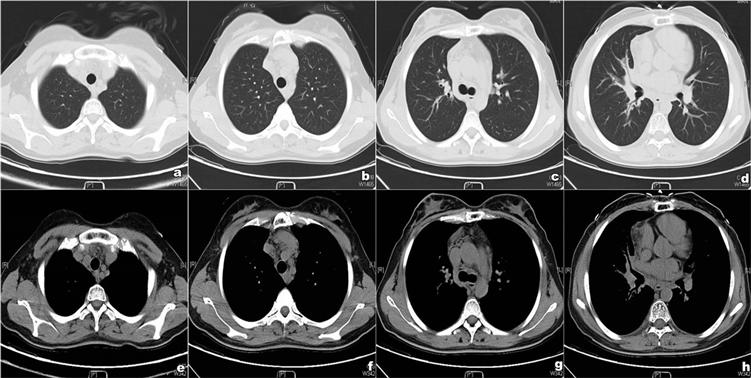
Figure 4. Chest routine scan (2013-03-18). (a)-(d) Showed clear lung texture in both lungs, enlarged right hilar shadow, thickened bronchial wall, scattered soft tissue shadow around, slightly narrowed lumen. (e)-(h) There are multiple lesions in the mediastinum, diffuse soft tissue density and fat density can be seen in the mediastinum, with unclear boundary and slightly enlarged mediastinal lymph nodes
图4. 胸部CT平扫(2013-03-18)。(a)~(d) 双肺纹理清晰,右肺门影增大,支气管壁增厚,周围可见散在软组织影,管腔略变窄。(e)~(h) 纵隔多发病变,纵隔内可见弥漫性软组织密度及脂肪密度,边界不清,纵隔淋巴结略肿大

Figure 5. Chest routine scan (2019-03-09). (a)-(d) Thickened the interlobular septa of the middle and lower lobes of the right lung, and the bronchus of trachea and various lobes was unobstructed. (e)-(h) bilateral hilar shadows increased, bilateral supravicular fossa, mediastinal, bilateral hilar, retroperitoneal and peritoneal diffuse patchy distribution, nodular soft tissue density interspersed with heteroadipose density shadow, lesions surrounded bilateral arteries, branches and esophagus. A watery density shadow was seen in the right thoracic cavity (arrow indicated the lesion location)
图5. 胸部CT平扫(2019-03-09)。(a)~(d) 右肺中下叶小叶间隔增厚,气管、诸叶段支气管通畅。(e)~(h) 双肺门影增大,双侧锁骨上窝、纵隔内、双侧肺门、腹膜后及腹膜内弥漫分布斑片状、结节状软组织密度间杂脂肪密度影,病变包绕双侧动脉及分支、食管。右侧胸腔内见水样密度影(箭头标注为病变位置)

Figure 6. Radionuclide lymphography of the patient
图6. 患者核素淋巴显像图
3. 讨论
淋巴管瘤病是淋巴管内皮细胞的异常增殖。它通常是一种儿童疾病,但它可能通过浸润器官,而在成年期出现临床表现 [5]。当淋巴管瘤病浸润到肺部时,即为DPL。浅表淋巴结淋巴管瘤病主要累及淋巴结囊及其周围软组织。从淋巴结活组织检查获得的信息可以提示并协助DPL的诊断 [6]。第一例患者经过外科肺活检最终确诊为DPL,第二例患者因为“血小板减少”病史16年,未给予气管镜检查,随访得知上级医院也因为病人血小板减少的原因,暂予升血小板治疗。曾有报道称DPL患者的胸膜活检显示弥漫性胸膜淋巴增生,可能以非特异性反应性变化而被忽视或被误诊为特发性间质性肺病 [2]。
DPL病情缓慢进展,肺部受累可能是轻微的,或引起弥漫性间质性肺病,气道阻塞,咯血,乳糜胸,心包积液,以及呼吸衰竭等 [5]。患者常有咳嗽、咳痰,多呈良性经过,但预后差,最终往往因肺内淋巴管弥漫增殖导致呼吸衰竭或继发感染而死亡 [2]。两例患者均出现“咳嗽、咳痰”症状,由于DPL多进展缓慢,所以肺部受累比较轻微。
淋巴管瘤病的胸部CT多表现为双肺片状、斑片、条索影,双侧胸腔积液,心包积液,纵隔内广泛团块状略低密度影。曾有报道称两例儿童DPL,双肺的小叶间隔和支气管血管束弥漫性增厚,双侧胸膜增厚 [7]。例一患者胸部CT纵隔窗可见广泛团块状略低密度影,部分融合状,未侵及周围组织、血管等,可能与该患者术后预后较好有关。另外,核素显像特点为全身淋巴管有不同程度的显像剂浓聚,例二中核素显像特点与文献报道一致。
DPL是一种罕见的淋巴病,其特征是淋巴管不受控制的增殖 [2],淋巴管生长受血管内皮生长因子(VEGF)的影响 [8]。临床表现无特异性,肺功能早期可正常,胸部CT多表现为双肺片状、斑片、条索影,纵隔内团块状略低密度影。气管镜检查需谨慎操作,例一患者气管镜术后咳大量橘红色浆液性痰,高度怀疑为纵隔内广泛融合的淋巴液。病理可见淋巴结呈反应性增生改变及大小不等的脉管 [9],病理结果为诊断该病的金标准。应与以下疾病相鉴别:肺静脉闭塞性疾病、癌性淋巴管炎、淋巴管平滑肌瘤病等 [10]。
目前DPL诊断困难,尚无有效的治疗方法。研究发现贝伐单抗有助于治疗以过度血管增殖为特征的疾病 [8] [11]。已有研究表明贝伐单抗成功治疗DPL [12]。临床工作中,DPL患者临床症状不典型,需要影像科、病理科等多学科协助诊断。
文章引用
潘 登,丛金鹏,王芳芳,成 炜,糜丽云,巩海红,陈云庆,于文成. 弥漫性肺淋巴管瘤病二例报告
Diffuse Pulmonary Lymphangiomatosis: Report of Two Cases[J]. 临床医学进展, 2020, 10(07): 1397-1404. https://doi.org/10.12677/ACM.2020.107210
参考文献
- 1. Libby, L.J., Narula, N., Fernandes, H., et al. (2016) Imatinib Treatment of Lymphangiomatosis. Journal of the National Comprehensive Cancer Network (JNCCN), 14, 383. https://doi.org/10.6004/jnccn.2016.0045
- 2. Lim, H.J., Han, J., Kim, H.K., et al. (1900) A Rare Case of Diffuse Pulmonary Lymphangiomatosis in a Middle-Aged Woman. Korean Journal of Radiology Official Journal of the Korean Radiological Society, 15, 295-299. https://doi.org/10.3348/kjr.2014.15.2.295
- 3. Liu, J.R., Shen, W.B., Wen, Z., et al. (2016) Clinical Analysis of Two Cases with Diffuse Pulmonary Lymphatic Disease. Zhonghua Er Ke Za Zhi, 54, 360-364.
- 4. Onyeforo, E., Barnett, A., Zagami, D., et al. (2018) Diffuse Pulmonary Lymphangiomatosis Treated with Bevacizumab. Respirology Case Reports. https://doi.org/10.1002/rcr2.384
- 5. Boland, J.M., Tazelaar, H.D., Colby, T.V., et al. (2013) Diffuse Pulmonary Lymphatic Disease Presenting As Interstitial Lung Disease in Adulthood: Report of 3 Cases Erratum. The American Journal of Surgical Pathology, 37. https://doi.org/10.1097/PAS.0b013e31829179c8
- 6. Ayadi-Kaddour, A., Cherif, J., Mlika, M., et al. (2009) Pulmonary Lymphangiomatosis Revealed by an Interstitial Syndrome in a Young Adult. La Tunisie Médicale, 87, 289-291.
- 7. Fang, X., Huang, Z., Zeng, Y., et al. (2017) Lymphangiomatosis Involving the Pulmonary and Extrapulmonary Lymph Nodes and Surrounding Soft Tissue. Medicine, 96, e9032. https://doi.org/10.1097/MD.0000000000009032
- 8. Aman, J., Thunnissen, E., Paul, M.A., et al. (2012) Successful Treatment of Diffuse Pulmonary Lymphangiomatosis with Bevacizumab. Annals of Internal Medicine, 156, 839. https://doi.org/10.7326/0003-4819-156-11-201206050-00016
- 9. Gurskyt, V., Zeleckien, I., Maskoliūnait, V., et al. (2020) Successful Treatment of Diffuse Pulmonary Lymphangiomatosis with Sirolimus. Respiratory Medicine Case Reports, 29, 101014. https://doi.org/10.1016/j.rmcr.2020.101014
- 10. Zhao, J., Wu, R. and Gu, Y. (2016) Pathology Analysis of a Rare Case of Diffuse Pulmonary Lymphangiomatosis. Annals of Translational Medicine, 4, 114. https://doi.org/10.21037/atm.2016.03.30
- 11. Zhang, J., Jin, H., Wang, Y., et al. (2015) A Case of Diffuse Pulmonary Lymphangiomatosis with Unilateral Lung Invasion. Oxford Medical Case Reports, 10, 346-348. https://doi.org/10.1093/omcr/omv059
- 12. Espinosa, V., Martin-Achard, A. and Guinand, O. (2012) Diffuse Pulmonary Lymphangiomatosis: (Corrected) Case Report and Literature Review. Revue Médicale Suisse, 8, 1125.
NOTES
*通讯作者。