Advances in Clinical Medicine
Vol.
13
No.
01
(
2023
), Article ID:
60202
,
6
pages
10.12677/ACM.2023.131038
镜面人急性阑尾炎1例
魏甜*,刘军舰,相志平
山东大学第二医院胃肠外科,山东 济南
收稿日期:2022年12月12日;录用日期:2023年1月5日;发布日期:2023年1月12日

摘要
急性阑尾炎的特征性表现是“右下腹痛”或“转移性右下腹痛”。阑尾切除术是其治疗的金标准。然而,对于左下腹痛我们常常会忽略阑尾炎的可能性。镜面人是指一类内置器官定位完全相反的人,这通常是由于在胚胎发育过程中发生异常所致。这就导致镜面人的阑尾炎诊断困难,容易漏诊、误诊,B超、CT等影像检查有助于其诊断。我们汇报了一例因左下腹痛2天而入院的47岁男性患者,CT诊断为内脏反位、左下腹阑尾粪石,急性阑尾炎表现。腹部查体示左下腹压痛。患者同意后行腹腔镜阑尾切除术。由于漏诊、误诊对患者和医生均会产生不良影响,我们认为在诊治过程中进行充分的评估非常重要,查体、影响学检查须合理充分使用。腹腔镜手术切除是治疗镜面人阑尾炎的首要选择。
关键词
急性阑尾炎,镜面人,腹痛,完全内脏反转

A Case of Acute Appendicitis in a Mirrored Man
Tian Wei*, Junjian Liu, Zhiping Xiang
Department of Gastroenterology Surgery, The Second Hospital of Shandong University, Ji’nan Shandong
Received: Dec. 12th, 2022; accepted: Jan. 5th, 2023; published: Jan. 12th, 2023

ABSTRACT
“Right lower abdominal pain” or “metastatic right lower abdominal pain” is the characteristic presentation of acute appendicitis. Appendectomy is the standard treatment for acute appendicitis. However, the possibility of appendicitis is often overlooked in the case of left lower abdominal pain. Mirrored people are a group of people with completely opposite positions of internal organs, usually due to abnormalities during embryonic development. This makes it difficult to diagnose appendicitis in mirrored people. It’s easy to miss and misdiagnose this condition. Ultrasound, CT and other imaging tests help in its diagnosis. We report a case of a 47-year-old male patient, who is admitted because of 2 days of left lower abdominal pain. His CT shows visceral inversion, left lower abdominal appendiceal faecal stone and presentation of acute appendicitis. His CT shows visceral inversion, an appendiceal fecal stone of the left lower abdomen, and the presentation of acute appendicitis. Abdominal examination showed pressure pain in the left lower abdomen. A laparoscopic appendectomy was performed after the admission of the patient. Because of the adverse effects of missed and misdiagnosis on both patients and doctors, we believe it is important to conduct an adequate assessment during the consultation and treatment process. The investigations and impact tests must be used appropriately and adequately. Laparoscopic surgical resection is the primary option for appendicitis in mirrored humans.
Keywords:Acute Appendicitis, Mirrored Man, Abdominal Pain, Situs Inversus Totalis

Copyright © 2023 by author(s) and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/


1. 前言
急性阑尾炎是最常见的急腹症之一,其终身发病率约为7%~8% [1],占所有急诊就诊人数4%~8%左右 [2]。完全内脏反转Situs inversus totalis (SIT)是一种罕见的常染色体隐性遗传病,发生率约为0.1~0.6/10,000 [3] [4] [5] [6]。SIT患者又称镜面人,指主要内脏器官完全呈镜像排列,包括心、肝、肺等 [7] [8],其阑尾也位于左下腹。绝大多数镜面人不自知,往往在就诊其他疾病时意外发现。据研究,SIT合并阑尾炎概率约为0.016%~0.024% [9] [10],它常表现为不典型左下腹痛。
左下腹痛的常见病因包括肠梗阻或穿孔、胃肠炎;肾/输尿管结石或炎症、附睾炎、睾丸扭转等,发生在镜面人上的左下腹阑尾炎通常不在考虑范围内,在这种情况下,阑尾炎症状不典型,诊断存在困难,极易导致误诊或漏诊,延误病情 [11] [12] [13]。因此在临床诊断中,应结合病史、查体、影响学手段等,充分评估并病情,对发生在左下腹的疼痛需考虑镜面人阑尾炎的可能性。
2. 病例汇报
我院2022年10月24日收治1例镜面人合并急性阑尾炎患者,现报告如下:
患者男,47岁。入院2天前无明显诱因出现腹部胀痛不适,左下腹为重,伴呕吐1次,呕吐物为胃内容物。无发热,无腹泻、脓血便,无腰痛、肩背部放射痛,无尿频、尿痛、血尿,无咳嗽、咯痰。自服胃药无明显好转。既往体健,无胃肠道病史。
查体:体温36.8℃,脉搏76次/分,呼吸18次/分,血压126/77 mmHg。神清语利,急性病容,双肺呼吸音清,心尖搏动位于右侧锁骨中线第五肋间旁开1.0 cm处,未闻及瓣膜杂音。腹部平坦,未见肠型及蠕动波,左下腹反麦氏点压痛明显,局部腹肌紧,反跳痛。其余腹部无压痛,左锁骨中线第五肋间叩诊可及浊音界,右侧肝浊音界未叩及,代之鼓音,肝肾区无叩痛,腹部移动性浊音阴性肠鸣音4次/分。
血化验结果示:白细胞计数209 × 109 (参考区间3.5~9.5 × 109),中性粒细胞百分率91.8% (参考区间40%~75%),血小板计数(参考区间125~350 × 109),红细胞计数5.23 × 1012 (参考区间4.30~5.80 × 109),血红蛋白浓度160 g/L (参考区间130~175 g/L);肝肾功、血凝无异常。
CT示:胸腹腔脏器转位;回盲部位于左下腹,提示急性阑尾炎,阑尾粪石;镜面右位心(见图1)。入院后初步诊断为:① 全内脏反位;② 急性阑尾炎。

Figure 1. The preoperative examination suggests complete visceral inversion. (A) The heart is located on the right side of the thorax (arrow); (B) ① the stomach in the right upper abdomen; ② the liver in the left upper abdomen; (C) The inverted pancreas (arrow); (D) The appendix is located in the left lower abdomen and contains a high-density appendiceal fecal stone (arrow)
图1. 术前检查提示完全性内脏反位。(A) 心脏位于胸腔右侧(箭头);(B) ①为位于右上腹的胃;②为位于左上腹的肝脏;(C) 为反位的胰腺(箭头);(D) 阑尾位于左下腹,内有高密度阑尾粪石(箭头)
患者诊断明确,行急诊手术治疗。手术分别在脐上1 cm、左、右髂前上嵴与脐连线中外三分之一处取1 cm、1 cm、0.5 cm小切口,建立操作孔,术中探查证实,阑尾位于左下腹,盲肠外位,长约6 cm,直径约1 cm,充血肿胀,呈坏疽性改变,表覆脓苔,周围大量黄色脓液,与周围组织粘连,积液约50 ml,行腹腔镜下阑尾切除术(见图2)。于盆腔放置引流管一根。术后标本送病理(见图3)。术后第3天拔出引流管,进食无不适,顺利出院。
3. 讨论
急性阑尾炎是腹部外科急诊最常见的疾病之一 [14]。典型的症状是转移性右下腹痛,即患者最初可能表现为中上腹部疼痛,随后出现右下腹痛,可能伴随有发热、恶心等不适 [15]。近一个世纪来,手术切除一直是治疗急性阑尾炎的金标准 [16]。然而,在极少数情况下,阑尾炎也可以表现为左下腹痛,常见于生长于左侧的阑尾发生炎症,见于中肠旋转不良 [2]、内脏反位 [17] 两种先天性疾病,也可偶见于生长于右侧的过长的阑尾伸入右下腹而引起左下腹痛 [18]。本病例是一例典型的先天性内脏反位合并急性阑尾炎患者。
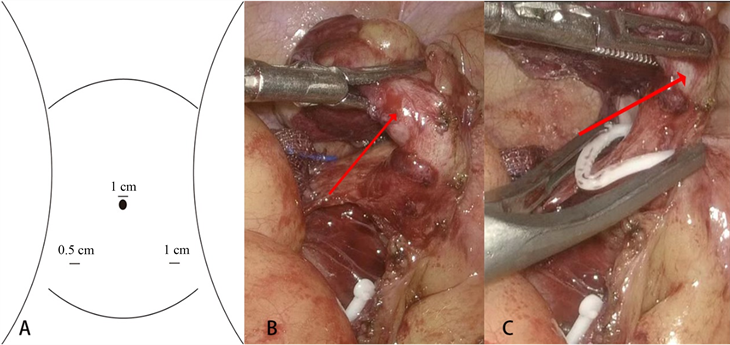
Figure 2. The surgical procedure. (A) shows a diagram of the trocar; (B) (C) the appendix is seen intraoperatively in the lower left abdomen (arrow), which is congested and swollen, the appendiceal artery is clamped and the appendix is removed at the root of the appendix
图2. 手术过程。(A) 为戳卡孔示意图;(B) (C) 术中见阑尾位于左下腹(箭头),充血肿胀,夹闭阑尾动脉,于阑尾根部切除阑尾
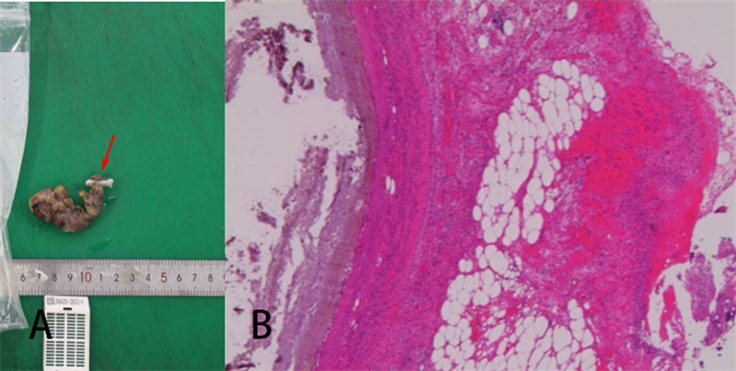
Figure 3. Postoperative pathology. (A) Gross pathology (arrows); (B) Microscopic pathology
图3. 术后病理。(A) 为大体病理(箭头);(B) 为镜下病理
内脏反位又称镜面人,是一类罕见的先天性隐形遗传学疾病,指器官从其正常部位反转到身体另一侧的位置,呈现镜像状态。其发生率据统计约在0.1~0.6/10,000不等 [3] [4] [5] [6]。可能包括胸腔内脏或腹腔内脏的转位,或者两者都有,前者称部位内脏转位,后者为完全内脏转位。本例患者属于完全内脏转位。当其合并有阑尾炎时,往往会表现为不典型的左下腹痛。
左下腹痛的最常见原因是急性乙状结肠炎 [19] [20],其他有诸如憩室炎、肠易激综合征、克罗恩病、溃疡性结肠炎、肠穿孔或梗阻等消化系统疾病,还可以是泌尿系统疾病、妇科疾病等 [2] [21] [22],然而左下腹的阑尾炎很少被考虑。尽管腹部超声、CT等影像学检查可以有助于疾病鉴别及内脏转位的诊断,但仍然容易误诊或漏诊,据相关报到误诊率可高达24% [11]。这一方面可能延误病情,导致疾病加重如发生阑尾穿孔、坏疽、腹膜炎等并发症 [12] [13],甚至因延误手术而增加死亡率 [23] [24];另一方面额外的检查也会加重患者负担。本例患者入院2天前突发左下腹疼痛,伴恶心、呕吐,无发热,单纯从症状考虑,很难想到和阑尾炎相关。
对于镜面人合并阑尾炎患者的诊断,除需要全面仔细的体格检查外,影像学检查是不可或缺的。胸部X线片可以提示右位心,腹部CT扫描可以提示有异位的内脏器官 [13] [22],腹部超声也是一项方便快捷的检查,具有提示意义。其中CT对于内脏反位合并阑尾炎的诊断最具敏感性 [13] [25] [26] [27]。而事实上,对于不明原因左下腹痛,美国放射学学会也是建议将CT作为评估的初始影像学检查 [28]。本病例患者提供了自己“镜面人”的病史,给疾病诊断提供了极大的帮助。考虑患者存在左侧阑尾炎可能性大,我们进行了CT检查,明确了左侧阑尾粪石,急性阑尾炎的诊断。对于左侧急性阑尾炎,治疗与正常阑尾相同,手术切除是标准治疗。而腹腔镜手术仍然是首要选择,兼具诊断和治疗作用 [25] [26] [27] [29]。经患者同意后,我们对患者急诊行腹腔镜下阑尾切除术。戳卡孔的选择没有固定或统一标准,以三切口居多,左侧反麦氏点、脐部成为相对固定选择,而另外1个戳卡空可以是耻骨上、右侧麦氏点等,根据阑尾具体位置或个人习惯有所不同 [13] [25] [26] [27];也有关于单孔腹腔镜下左侧阑尾切除术的报道 [30]。此例患者我们选择的是脐上置入10 mm戳卡作为观察孔,左、右髂前上嵴与脐连线中外三分之一处分别置入1 cm、0.5 cm戳卡作为操作孔。手术较为顺利。
4. 结论
镜面人阑尾炎是一类罕见疾病,多表现为不典型左下腹痛,临床诊断存在困难,容易误诊或漏诊,给患者及医生均会带来不良影响。建议把左侧阑尾炎纳入左下腹痛的鉴别诊断之一。详细采集病史及全面仔细的体格检查对于诊断非常重要,在怀疑左侧阑尾炎或诊断存在困难时,可选择CT作为首选检查。镜面人的阑尾炎诊断明确后,手术治疗尤其是腹腔镜手术仍然是首要治疗手段。
文章引用
魏 甜,刘军舰,相志平. 镜面人急性阑尾炎1例
A Case of Acute Appendicitis in a Mirrored Man[J]. 临床医学进展, 2023, 13(01): 246-251. https://doi.org/10.12677/ACM.2023.131038
参考文献
- 1. Ellis, K., Fleming, R.J., Griffiths, S.P., et al. (1966) New Con-cepts in Dextrocardia. Angiocardiographic Considerations. American Journal of Roentgenology, 97, 295-313. https://doi.org/10.2214/ajr.97.2.295
- 2. Rosenberg, H.N. and Rosenberg, I.N. (1949) Simultaneous Association of Situs Inversus, Coronary Heart Disease and Hiatus Hernia: Report of a Case and Review of Literature. Annals of In-ternal Medicine, 30, 851-859. https://doi.org/10.7326/0003-4819-30-4-851
- 3. Perera, W.R. and Hennessy, O.F. (2010) Clinical Images. An Unusual Case of Appendicitis. The American Journal of Surgery, 199, e79-e81. https://doi.org/10.1016/j.amjsurg.2009.08.047
- 4. Huang, S.-M., Yao, C.-C., Tsai, T.-P. and Hsu, G.-W. (2008) Acute Appendicitis in Situs Inversus Totalis. Journal of the American College of Surgeons, 207, 954. https://doi.org/10.1016/j.jamcollsurg.2008.03.030
- 5. Kryzauskas, M., Danys, D., Poskus, T., et al. (2016) Is Acute Appendicitis Still Misdiagnosed? Open Medicine, 11, 231-236. https://doi.org/10.1515/med-2016-0045
- 6. Papandria, D., Goldstein, S.D., Rhee, D., et al. (2013) Risk of Perfo-ration Increases with Delay in Recognition and Surgery for Acute Appendicitis. Journal of Surgical Research, 184, 723-729. https://doi.org/10.1016/j.jss.2012.12.008
- 7. Contini, S., Dalla Valle, R. and Zinicola, R. (1998) Sus-pected Appendicitis in Situs Inversus Totalis: An Indication for a Laparoscopic Approach. Surgical Laparoscopy & En-doscopy, 8, 393-394. https://doi.org/10.1097/00019509-199810000-00017
- 8. Kong, L., Zhang, H., Liu, K., Zhao, L. and Lu, B. (2022) How to Manage Appendicitis in Pregnancy Better. Gastrointestinal Endoscopy, 95, 1018-1019. https://doi.org/10.1016/j.gie.2022.01.011
- 9. Sandell, E., Berg, M., Sandblom, G., et al. (2015) Surgical Deci-sion-Making in Acute Appendicitis. BMC Surgery, 15, Article No. 69. https://doi.org/10.1186/s12893-015-0053-x
- 10. Krzyzak, M. and Mulrooney, S.M. (2020) Acute Appendicitis Review: Background, Epidemiology, Diagnosis, and Treatment. Cureus, 12, e8562. https://doi.org/10.7759/cureus.8562
- 11. Evola, G., Ferrara, F., Di Fede, G.F., et al. (2022) Left-Sided Acute Ap-pendicitis in a Patient with Situs Viscerum Inversus Totalis: A Case Report. International Journal of Surgery Case Re-ports, 90, Article ID: 106658. https://doi.org/10.1016/j.ijscr.2021.106658
- 12. Keli, E., Ndri, K.J., Ahue, K.H., et al. (2019) Laparoscopic Ap-pendicectomy in a Patient with Situs Inversus Totalis. South African Journal of Surgery, 57, 66-67. https://doi.org/10.17159/2078-5151/2019/v57n2a2951
- 13. Aassouani, F., Charifi, Y., Hajjar, C., et al. (2022) Left-Sided Appendicitis Revealing a Common Mesentery: A Case Report. Radiology Case Reports, 17, 3718-3721. https://doi.org/10.1016/j.radcr.2022.07.009
- 14. Cartwright, S.L. and Knudson, M.P. (2015) Diagnostic Imaging of Acute Abdominal Pain in Adults. American Family Physician, 91, 452-459.
- 15. Yang, C.-Y., Liu, H.-Y., Lin, H.-L. and Lin, J.-N. (2012) Left-Sided Acute Appendicitis: A Pitfall in the Emergency Department. The Journal of Emergency Medicine, 43, 980-982. https://doi.org/10.1016/j.jemermed.2010.11.056
- 16. Cartwright, S.L. and Knudson, M.P. (2008) Evaluation of Acute Abdominal Pain in Adults. American Family Physician, 77, 971-978.
- 17. Saliba, C., Diab, S.H., Nicolas, G., et al. (2019) Pitfalls of Diagnosing Left Lower Quadrant Pain Causes: Making the Uncommon Com-mon Again. American Journal of Case Reports, 20, 78-82. https://doi.org/10.12659/AJCR.912226
- 18. Seifmanesh, H., Jamshidi, K., Kordjamshidi, A., et al. (2010) Acute Left-Sided Appendicitis with Situs Inversus Totalis: A Case Report. The American Journal of Emergency Medicine, 28, 1058.e5-1058.e7. https://doi.org/10.1016/j.ajem.2010.01.020
- 19. Stewart, B., Khanduri, P., Mccord, C., et al. (2014) Global Disease Burden of Conditions Requiring Emergency Surgery. British Journal of Surgery, 101, e9-e22. https://doi.org/10.1002/bjs.9329
- 20. Nelson, M.J. and Pesola, G.R. (2001) Left Lower Quadrant Pain of Unusual Cause. Journal of Emergency Medicine, 20, 241-245. https://doi.org/10.1016/S0736-4679(00)00316-4
- 21. Oh, J.S., Kim, K.W. and Cho, H.J. (2012) Left-Sided Appendicitis in a Patient with Situs Inversus Totalis. Journal of the Korean Surgical Society, 83, 175-178. https://doi.org/10.4174/jkss.2012.83.3.175
- 22. Akbulut, S., Caliskan, A., Ekin, A. and Yagmur, Y. (2010) Left-Sided Acute Appendicitis with Situs Inversus Totalis: Review of 63 Published Cases and Report of Two Cases. Journal of Gastrointestinal Surgery, 14, 1422-1428. https://doi.org/10.1007/s11605-010-1210-2
- 23. Palanivelu, C., Rangarajan, M., John, S.J., Senthilkumar, R. and Madhankumar, M.V. (2007) Laparoscopic Appendectomy for Appendicitis in Uncommon Situations: The Advantages of a Tailored Approach. Singapore Medical Journal, 48, 737-740.
- 24. Akbulut, S., Ulku, A., Senol, A., Tas, M. and Yagmur, Y. (2010) Left-Sided Appendicitis: Review of 95 Published Cases and a Case Report. World Journal of Gastroenterology, 16, 5598-5602. https://doi.org/10.3748/wjg.v16.i44.5598
- 25. Golash, V. (2006) Laparoscopic Management of Acute Appendicitis in Situs Inversus. Journal of Minimal Access Surgery, 2, 220-221. https://doi.org/10.4103/0972-9941.28184
- 26. Galgano, S.J., Mcnamara, M.M., Peterson, C.M., et al. (2019) ACR Appropriateness Criteria® Left Lower Quadrant Pain-Suspected Diverticulitis. Journal of the American College of Radi-ology, 16, S141-S149. https://doi.org/10.1016/j.jacr.2019.02.015
- 27. Pipal, D.K., Pipal, V.R. and Yadav, S. (2022) Acute Appendicitis in Situs Inversus Totalis: A Case Report. Cureus, 14, e22947. https://doi.org/10.7759/cureus.22947
- 28. Budhiraja, S., Singh, G., Miglani, H.P. and Mitra, S.K. (2000) Ne-onatal Intestinal Obstruction with Isolated Levocardia. Journal of Pediatric Surgery, 35, 1115-1116. https://doi.org/10.1053/jpsu.2000.7839
- 29. Evans, W.N., Acherman, R.J. and Restrepo, H. (2015) Heterotaxy in Southern Nevada: Prenatal Detection and Epidemiology. Pediatric Cardiology, 36, 930-934. https://doi.org/10.1007/s00246-015-1099-3
- 30. Rajkumar, J.S., Syed, A., Anirudh, J.R., Kishor, C.M. and Ganesh, D. (2016) Single-Incision Multi-Port Appendectomy for a Pa-tient with Situs Inversus Totalis: First Case Report. Sultan Qaboos University Medical Journal, 16, 242-245. https://doi.org/10.18295/squmj.2016.16.02.018
NOTES
*通讯作者。