Advances in Clinical Medicine
Vol.05 No.03(2015), Article ID:15986,6
pages
10.12677/ACM.2015.53027
Clinical Treatment of Distal Fibular Tumours in Children
Haisen Hong*, Mo Sha, Hui Liu, Yanwei Li
Department of Orthopaedics, The 175th Hospital of PLA, Zhangzhou Fujian
*通讯作者。
Email: *hhs123702@163.com
Received: Aug. 3rd, 2015; accepted: Aug. 20th, 2015; published: Sept. 4th, 2015
Copyright © 2015 by authors and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



ABSTRACT
Objective: To study the clinical and functional outcomes of surgical treatment in a case series of nine patients with distal fibular tumours. Method: Nine patients with distal fibular tumours were followed up and observed between June 2011 and September 2014. A PubMed search was performed using the terms “fibula”, “lower limb tumour (cancer)”, “sarcoma”, “Ewing”, “peroneal”, “fibular metastasis”. Result: All cases were followed-up for 3.6 ± 1.5 years. In all our patients, lesions were unilateral. All patients complained of pain; limping was present in 5 of 9 patients. Patients were managed surgically, except one who underwent local radiotherapy. In six patients, a benign or tumor-like lesion was detected. Malignancies consisted of metastatic lung adenocarcinoma (two cases) or multifocal mesenchymal cancer (one case). Non-malignant lesions were treated by curettage and filling, followed by internal fixation when needed. In malignant or locally aggressive lesions, metadiaphyseal fibular resection was performed. The literature search retrieved either case reports or small case series, reflecting the rarity of distal fibular tumours. Surgical treatment was successful in all patients with benign lesions, whereas the rate of success was 40% - 100% in case of malignancies. Conclusion: Given the low incidence of distal fibular tumours, controversies exist about the optimal surgical management. Clinical observation and imaging should be reserved to asymptomatic benign lesions. In non-malignant tumours causing pain,, limping, and pathological fractures and malignancies, surgery is recommended. Finally, in patients with asymptomatic lesions of uncertain nature, biopsy and histological examination should be performed to plan appropriate management.
Keywords:Fibula, Tumour, Limb-Salvage Surgery, Bone Graft, Internal Fixation

儿童腓骨远端肿瘤的临床处理
洪海森*,沙漠,刘晖,李延炜
解放军第175医院骨科,福建 漳州
Email: *hhs123702@163.com
收稿日期:2015年8月3日;录用日期:2015年8月20日;发布日期:2015年9月4日

摘 要
目的:观察9例儿童腓骨远端肿瘤患者手术治疗后的临床疗效和功能评定。方法:2011年6月~2014年9月期间9例儿童腓骨远端肿瘤患者获得术后随访。PubMed搜索使用术语“腓骨”,“下肢肿瘤(癌症)”,“肉瘤”、“尤文氏肉瘤”、“腓骨的”、“腓骨转移”。结果:所有患者均为单侧病变并获得随访,平均随访3.6 ± 1.5年;所有患者诉有疼痛,其中9例患者中5例出现疼痛及跛行。除了1例接受放疗外其他患者均进行手术处理。在6位患者中,1例为良性的肿瘤或肿瘤样变。2例恶性肺腺癌转移及1例多病灶的间质肿瘤。腓骨治疗性病灶清除后进行植骨,然后进行内固定处理术后没有恶变。在恶性或活动期病变中进行腓骨瘤段切除。文献检索中无论是案例报告还是小案例系列,均反映出腓骨远端的肿瘤较为罕见。在所有良性病变患者中手术治疗是成功的,而恶性肿瘤的成功率为40%~100%。结论:腓骨远端肿瘤的发病率低,最佳手术治疗方案存在争议。无症状的良性病变应进行临床观察及定期影像学检查随访。在非恶性肿瘤出现疼痛,跛行,病理骨折及恶性肿瘤时建议手术治疗。最后,在无症状患者或疾病诊断不确定时应进行穿刺活检或病理组织学检查。
关键词 :腓骨,肿瘤,保肢手术,植骨,内固定

1. 引言
近年来随着外科技术的进步,骨肿瘤的外科治疗效果明显提高,2年无瘤存活率由原来30%提高到80%左右[1] 。当前已不再把截肢手术作为治疗恶性骨肿瘤的首选方法,许多学者推崇采用局部广泛或局部根治性肿瘤切除和保留肢体的手术,即通过外科手术切除肿瘤病灶,同时应用辅助化疗消除已发生的显微转移病灶。临床上由于腓骨肿瘤涉及腓骨切除(fibular resection)的手术并不少见,儿童腓骨肿瘤切除后对踝功能的影响日益受到重视。腓骨部分切除后造成患侧踝关节不同程度的活动受限,肌力下降,对儿童甚至产生踝关节外翻畸形,近年来都有不少相关报道[1] -[4] ,对腓骨功能的重要性也有了进一步的认识。为进一步观察腓骨远端肿瘤患者手术治疗后的临床疗效,我科对2011年6月~2014年9月期间9例腓骨远端肿瘤患者术后进行随访,临床疗效满意,并文献检索腓骨远端肿瘤病例报告进行回顾性分析。现报告如下。
2. 临床资料
2.1. 一般资料
9例中女性患者3例,男性6例;平均年龄12.6岁。病程3个月~5.7年,平均10.6个月。患者的平均年龄(三个女性和六个男性)为44.3 ± 24.8岁(范围17~76岁)。所有患者均为单侧病变,在休息或活动期间均有疼痛,另外5例伴跛行。6例患者为良性或类肿瘤病变。2例患者其中一例右腓骨成纤维型骨肉瘤,一例在对侧踝远端骨间膜。其余为多病灶的间质肿瘤患者累及腓骨远端。
2.2. 处理方式
除了一例患者因为放疗后健康状况不允许外所有患者均行手术治疗。操作均由同一骨科医生执行。患者1 (右腓骨成纤维型骨肉瘤)经过病理组织学活检诊断后再手术。根据病变位置,肿瘤范围和性质,手术治疗是在病灶清除术后加填充自体骨或骨水泥,或切除后在必要时通过钢板螺丝内固定融合处理。3例患者术后进行化疗处理。
3. 结果
3.1. 随访结果
平均随访时间为48个月,除了1例患者手术后18个月去世,1例患者手术后12个月去世,其他患者均同意并获得随访。手术后建议患者进行腿部及踝部功能锻炼。一个月后逐渐开始负重。术后所有患者患肢与对侧踝关节活动进行对比,运动的范围是正常的,除了2例患者踝关节屈曲和伸展活动受限约10˚以及1例患者行走时有轻微的疼痛外所有患者均没有疼痛或跛行(图1、图2)。在任何情况下都没有出现内翻内收踝关节不稳定、皮肤切口延迟愈合、不愈合或局部感染,没有局部病灶复发。
3.2. 文献检索
PubMed搜索使用术语“腓骨”,“下肢肿瘤(癌症)”,“肉瘤”、“尤文氏肉瘤”、“腓骨的”、“腓骨转移”。搜索没有检索到大样本研究腓骨远端肿瘤的外科手术治疗案例。仅有单一的个案报道或小样本分析报告与之相关[5] -[8] ,反映出腓骨远端肿瘤罕见性。现有证据表明,在所有良性病变患者中手术后的功能效果是良好的,而恶性肿瘤患者的成功率为40%~100% (表1)。这些研究结果与我们的结果一致。

Figure 1. Male, aged 12, patient of right fibula fibroblasts osteosarcoma
图1. 男性,12岁,右腓骨成纤维型骨肉瘤患者
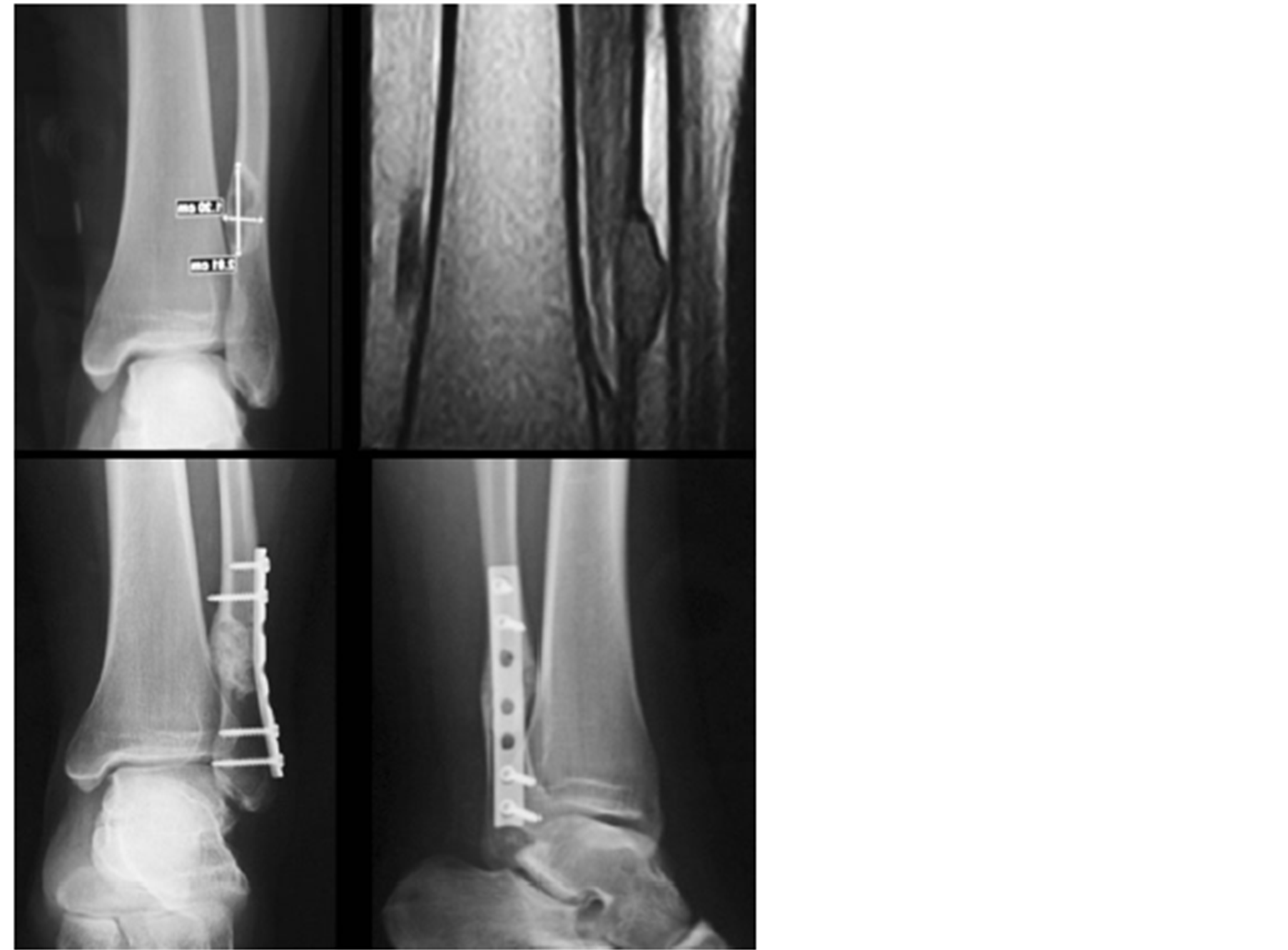
Figure 2. Male, aged 16, patient of distal fibula bone fibroma
图2. 男性,16岁,腓骨远端骨纤维瘤患者
Table 1. The rate of success was 40% - 100 % in case of malignancies
表1.恶性肿瘤患者手术后的成功率是40%~100%
4. 讨论
腓骨远端的肿瘤非常罕见,对腓骨远端肿瘤的治疗带来很大的挑战。整个腓骨远端的广泛切除术会导致踝关节稳定性和临界软组织条件的失去,故需要重建一个稳定的踝关节和足够的皮肤覆盖的区域。在恶性肿瘤患者中,保肢手术也是很少考虑的,因为大面积的切除难以实现保肢。据报道,腓骨骨肉瘤保肢手术后其周围附属物容易再次发生病变[6] ,外科手术边缘切除不足导致局部复发和转移率升高[7] 。这种观点最近受到其他作者质疑,他们观察到:在腓骨骨肉瘤患者经历了带瘤体边缘切除和辅助放化疗后肿瘤并没有复发及对生存产生影响[8] [9] 。故保肢手术配合化疗的进展很可能将越来越流行[10] 。
考虑到腓骨远端肿瘤的多样和低发病率,不同的疾病描述了一些解决方案[11] 。几十年来,恶性肿瘤的主要治疗方法为膝下截肢:包括远端腓骨和胫骨[12] 。外科技术的进步和化疗能够减少破坏性方法的选择。例如:腓骨远端肿瘤外踝切除后没有进行腓骨重建[13] [14] 。在这种情况下,踝关节稳定获得仅通过软组织和韧带重建或行踝关节融合术[15] [16] 。或者腓骨切除后采用与同种异体腓骨或自体骨,带蒂的同侧近端骨骺转移腓骨或取髂骨植骨,骨移植或假肢踝关节置换进行重建踝关节[17] 。而选择一个特定的手术方式通常是由外科医生的偏好和经验,而不是由肿瘤的性质和范围决定。
上面描述的所有外科技术均有自己的优点和缺点。腓骨远端切除的常见并发症包括弓形腿、外翻畸形、踝关节活动受限和软组织覆盖不足。患者腓骨切除后接受腓骨远端与腓骨头重建,供体部位骨坏死,同侧膝关节不稳定,腓总神经损伤,近端腓骨和下胫腓联合表面之间的不协调和骨不连、踝关节置换术后距骨塌陷等均有报道[18] 。
考虑到腓骨远端肿瘤发病率低及腓骨在踝关节生物力学中的作用,最佳手术治疗方案存在争议。基于我们的经验和在这一课题的文献报道,我们提出一个双重的方法。对于无症状的良性肿瘤或类肿瘤病变建议患者临床观察与定期影像学检查。对于非恶性肿瘤患者出现持续疼痛、跛行、病理性骨折或大型病变及恶性肿瘤患者建议手术治疗。最后,在无症状的不确定性质的病变应该执行病理活检和组织学检查。
基于我们的系列随访及文献报告:我们认为良性和类肿瘤病变可以成功地通过病灶刮除术和填充植骨,自体骨移植或骨水泥。对于局部活动性强波及腓骨骨骺的良性肿瘤应该使用瘤体切除和螺丝钉内固定。最后,在恶性病变的存在并不涉及外踝且距离下胫腓联合至少
腓骨切除后导致踝关节不稳可能与腓骨失去完整性,生理负重功能的丧失,足外翻时距骨向外上方挤压外踝导致外踝移位,胫骨轴承重过多及软组织的牵拉作用等因素相关[19] 。近年来不少学者提出运用手术预防或减轻儿童腓骨切除后踝关节不稳定的发生,对于切除腓骨中下段的患者尤为必要[20] 。临床上不少手术均涉及腓骨的切除,其术后对踝关节稳定性的影响不容忽视,临床上需重视以下几点:1) 腓骨切除的长度和远端保留的长度与并发症相关,须认真考虑;2) 儿童行腓骨切除后的并发症较成人多且严重,要严格控制手术指征;3) 胫腓远端固定术防治踝关节不稳的疗效尚存在争议;4) 积极的术后康复治疗对患侧肢体功能的恢复是有利的。
文章引用
洪海森,沙 漠,刘 晖,李延炜. 儿童腓骨远端肿瘤的临床处理
Clinical Treatment of Distal Fibular Tumours in Children[J]. 临床医学进展, 2015, 05(03): 171-176. http://dx.doi.org/10.12677/ACM.2015.53027
参考文献 (References)
- 1. González-Herranz, P., del Río, A., Burgos, J., López-Mondejar, J.A. and Rapariz, J.M. (2003) Valgus deformity after fibular resection in children. Journal of Pediatric Orthopaedics, 23, 55-59. http://dx.doi.org/10.1097/00004694-200301000-00011
- 2. Chin, K.R., Kharrazi, F.D., Miller, B.S., Mankin, H.J. and Gebhardt, M.C. L (2000) Osteochondromas of the distal aspect of the tibia or fibula. Natural history and treatment. The Journal of Bone & Joint Surgery (American Volume), 82, 1269-1278.
- 3. Fragniere, B., Wicart, P., Mascard, E. and Dubousset, J. (2003) Prevention of ankle valgus after vascularized fibular grafts in children. Clinical Orthopaedics & Related Research, 408, 245-251. http://dx.doi.org/10.1097/00003086-200303000-00032
- 4. Lambert, K.L. (1971) The weight bearing function of the fibula: a strain gauge study. The Journal of Bone & Joint Surgery (American Volume), 53, 507-513.
- 5. Wang, Q., Whittle, M., Cunningham, J. and Kenwright, J. (1996) Fibular and its ligments in load transmission and ankle joint sta-bility. Clinical Orthopaedics and Related Research, 70, 261-270.
- 6. Lee, S.H., Kim, H.S., Park, Y.B., Rhie, T.Y. and Lee, H.K. (1999) Prosthetic reconstruction for tumours of the distal tibia and fibula. The Bone & Joint Journal, 81, 803-807. http://dx.doi.org/10.1302/0301-620X.81B5.9588
- 7. Schneiderbauer, M.M., Gullerud, R., Harmsen, W.S. and Scully, S.P. (2007) Fibular osteosarcomas: Contaminated margins may not impact survival. Clinical Ortho-paedics and Related Research, 456, 182-187. http://dx.doi.org/10.1097/01.blo.0000238834.95928.0f
- 8. Grimer, R.J., Taminiau, A.M. and Cannon, S.R. (2002) Surgical outcomes in osteosarcoma. The Bone & Joint Journal, 84, 395-400. http://dx.doi.org/10.1302/0301-620X.84B3.12019
- 9. Lindner, N.J., Ramm, O., Hillmann, A., Roedl, R., Go-sheger, G., Brinkschmidt, C., Juergens, H., Winkelmann, W. (1999) Limb salvage and outcome of osteosarcoma. The University of Muenster experience. Clinical Orthopaedics and Related Research, 358, 83-89. http://dx.doi.org/10.1097/00003086-199901000-00011
- 10. Kanazawa, Y., Tsuchiya, H., Nonomura, A., Taka-zawa, K., Yamamoto, N. and Tomita, K. (2003) Intentional marginal excision of osteosarcoma of the proximal fibula to preserve limb function. Journal of Orthopaedic Science, 8, 757-761. http://dx.doi.org/10.1007/s00776-003-0714-y
- 11. Dieckmann, R., Ahrens, H., Streitbürger, A., Budny, T.B., Henrichs, M.P., Vieth, V., Gebert, C. and Hardes, J. (2011) Reconstruction after wide resection of the entire distal fibula in malignant bone tumours. International Orthopaedics, 35, 87-92. http://dx.doi.org/10.1007/s00264-009-0931-x
- 12. Ozaki, T., Hillmann, A., Lindner, N. and Winkelmann, W. (1997) Surgical treatment of bone sarcomas of the fibula. Analysis of 19 cases. Archives of Orthopaedic and Trauma Surgery, 116, 475-479. http://dx.doi.org/10.1007/BF00387580
- 13. Norman-Taylor, F.H., Sweetnam, D.I. and Fixsen, J.A. (1994) Distal fibulectomy for Ewing’s sarcoma. The Bone & Joint Journal, 76, 559-562.
- 14. Carnesale, P. (1998) General principals of tumors. In: Canale, S.T., Ed., Campbells’s operative orthopaedics, 10th Edition, Mosby, St. Louis, 647-648.
- 15. Yadav, S.S. (1981) Ankle stability after resection of the distal third of the fibula for giant-cell lesions: Report of two cases. Clinical Orthopaedics and Related Research, 156, 105-107. http://dx.doi.org/10.1097/00003086-198103000-00019
- 16. Pickering, R. (2003) Arthrodesis of ankle, knee, and hip. In: Pickering, R.M., Ed., Campbells’s operative orthopaedics, 10th Edition, Mosby, St. Louis.
- 17. Capanna, R., van Horn, J.R., Biagini, R., Ruggieri, P., Bettelli, G. and Campanacci, M. (1986) Reconstruction after resection of the distal fibula for bone tumor. Acta Orthopaedica Scandinavica, 57, 290-294. http://dx.doi.org/10.3109/17453678608994394
- 18. Lubliner, J.A., Robbins, H., Lewis, M.M., Present, D. (1985) Aneurysmal bone cyst of the fibula: En bloc resection with allograft reconstruction. Bulletin of the Hospital for Joint Diseases Orthopaedic Institute, 45, 80-86.
- 19. He, X.J., Li, H.P., Jin, L.S., Lan, B.S., Wang, K.Z. and Mao, L.Z. (2000) Functional development of the donor leg after vascularized fibula graft in childhood. Journal of Pediatric Surgery, 35, 1226-1229. http://dx.doi.org/10.1053/jpsu.2000.8759
- 20. Kanaya, K., Wada, T., Kura, H., Yamashita, T., Usui, M. and Ishii, S. (2002) Valgus deformity of the ankle following harvesting of a vascularized fibular graft in children. Journal of Re-constructive Microsurgery, 18, 91-96. http://dx.doi.org/10.1055/s-2002-19888
