Advances in Clinical Medicine
Vol.
10
No.
11
(
2020
), Article ID:
38873
,
5
pages
10.12677/ACM.2020.1011416
CD4+T淋巴细胞计数在ANCA相关性血管炎患者治疗过程中的变化及其意义
周静月1,苏阳2,张小凡1,高鹏丽1,陈怿鹏1,邢广群1*
1青岛大学附属医院肾内科,山东 青岛
2青岛大学附属医院心内科,山东 青岛
收稿日期:2020年11月2日;录用日期:2020年11月20日;发布日期:2020年11月27日

摘要
目的:探讨CD4+T淋巴细胞计数在ANCA相关性血管炎患者治疗过程中的变化及其意义。方法:选择青岛大学附属医院2019年1月1日~2020年8月1日在肾内科初诊为AAV的患者35例,检测患者活动期和缓解期CD4+T淋巴细胞计数、白细胞计数、淋巴细胞计数、中性粒细胞计数、C反应蛋白(CRP)、白蛋白(ALB)、估算的肾小球滤过率(eGFR)、血肌酐(Scr)、BVAS评分及红细胞沉降率(ESR)的变化,并分析BVAS评分与CD4+T淋巴细胞计数之间的关系。结果:缓解期患者BVAS评分、白细胞计数、中性粒细胞计数、ALB、CRP、ESR均显著下降,而CD4+T淋巴细胞、ALB治疗后均显著升高,而淋巴细胞计数、Scr、eGFR比较差异均无统计学意义(P > 0.05)。Spearman相关性分析显示,活动期时患者BVAS评分与CD4+T淋巴细胞计数呈显著负相关关系(r = −0.398, P < 0.05)。结论:AAV患者治疗不同时期CD4+T淋巴细胞计数有明显的变化,监测血清中CD4+T淋巴细胞计数可以指导AAV患者的临床治疗。
关键词
ANCA相关性血管炎,CD4+T淋巴细胞计数,感染

The Significance of CD4+T Lymphocyte Count during the Treatment of Patients with ANCA-Associated Vasculitis
Jingyue Zhou1, Yang Su2, Xiaofan Zhang1, Pengli Gao1, Yipeng Chen1, Guangqun Xing1*
1Department of Nephrology, The Affiliated Hospital of Qingdao University, Qingdao Shandong
2Department of Cardiology, The Affiliated Hospital of Qingdao University, Qingdao Shandong
Received: Nov. 2nd, 2020; accepted: Nov. 20th, 2020; published: Nov. 27th, 2020

ABSTRACT
Objective: To investigate the changes and significance of CD4+T lymphocyte count during the treatment of patients with ANCA-related vasculitis. Methods: Thirty-five patients who were newly diagnosed with AAV in the Department of Nephrology from Qingdao University Hospital from January 1, 2019 to August 1, 2020 were selected to detect CD4+T lymphocyte counts, white blood cell counts, lymphocyte counts, medium Changes in neutrophil count, C-reactive protein (CRP), albumin (ALB), estimated glomerular filtration rate (eGFR), blood creatinine (Scr), BVAS score and erythrocyte sedimentation rate (ESR), and analyzed the relationship between BVAS score and CD4+T lymphocyte count. Results: BVAS score, white blood cell count, neutrophil count, ALB, CRP, and ESR of patients in remission stage decreased significantly, while CD4+T lymphocytes and ALB increased significantly after treatment, but there was no difference in lymphocyte count, Scr, eGFR Statistical significance (P > 0.05). Spearman correlation analysis showed that there was a significant negative correlation between the BVAS score and CD4+T lymphocyte count of patients in the active phase (r = −0.398, P < 0.05). Conclusion: The CD4+T lymphocyte counts of AAV patients have significant changes in different periods of treatment. Monitoring the serum CD4+T lymphocyte counts can guide the clinical treatment of AAV patients.
Keywords:ANCA-Associated Vasculitis, CD4+T Lymphocytes, Infection

Copyright © 2020 by author(s) and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/


1. 引言
抗中性粒细胞胞浆抗体(anti-neutrophil cytoplasmic antibody, ANCA)相关性血管炎(ANCA-associated vasculitis, AAV)是一种可以累及肾脏、肺脏及耳鼻喉等全身多脏器的系统性血管炎。根据2012年Chapel Hill分类,主要分为显微镜下多血管炎(microscopic polyangiitis, MPA)、肉芽肿性多血管炎(granulomatosis with polyangiitis, GPA)和嗜酸性肉芽肿性多血管炎(eosinophilic granulomatosis with polyangiitis, EGPA) [1]。有研究表明,CD4+T淋巴细胞参与了AAV的病情的进展 [2],但是CD4+T细胞变化的意义尚未阐明。本文就初诊为AAV患者缓解期和活动期2个时间节点探讨CD4+T淋巴细胞变化在AAV中的临床价值,从而为疾病提供更好的治疗方案。
2. 资料与方法
回顾性分析我院2018年1月1日~2020年8月1日于我院肾内科初诊为AAV的患者,并于活动期和缓解期均检测过CD4+T淋巴细胞细胞计数的AAV患者共35例,检测患者活动期和缓解期CD4+T淋巴细胞计数、白细胞计数、淋巴细胞计数、中性粒细胞计数、C反应蛋白(CRP)、白蛋白(ALB)、估算的肾小球滤过率(eGFR)、血肌酐(Scr)、伯明翰系统性血管炎活动性评分(BVAS) [3] 及红细胞沉降率(ESR)的变化,并分析BVAS评分与CD4+T淋巴细胞计数之间的关系。患者各时期的BVAS评分通过查看病历和实验室检查计算,eGFR运用CKD-EPI [4] 公式计算。该研究已经获得相应的伦理许可。
采用SPSS21.0统计软件进行数据分析整理,计数资料以例数表示,符合正态分布计量资料以 ± s表示,活动期和缓解期前后比较采用配对样本t检验分析;不符合正态分布计量资料以M(P25, P75)表示,活动期和缓解期前后比较用Wilcoxon检验分析。CD4+T淋巴细胞计数与BVAS评分之间的关系采用Spearman相关性分析。以P < 0.05为差异有统计学意义。
3. 结果
35例患者中男19例,女16例,平均年龄63.14 ± 11.45岁,最大年龄77岁,最小年龄19岁,平均体重64.20 ± 13.80 kg,最大体重100 kg,最小体重35 kg。缓解期患者BVAS评分、白细胞计数、中性粒细胞计数、ALB、CRP、ESR均显著下降,而CD4+T淋巴细胞、ALB治疗后均显著升高,而淋巴细胞计数、Scr、eGFR比较差异均无统计学意义(P > 0.05)。见表1。Spearman相关性分析显示,活动期时患者BVAS评分与CD4+T淋巴细胞计数呈显著负相关关系(r = −0.398, P < 0.05)见图1、图2。ANCA相关性血管炎患者治疗不同时期CD4+T淋巴细胞计数有明显的变化,监测血清中CD4+T淋巴细胞计数可以指导AAV患者的临床治疗。
Table 1. Comparison of indicators before and after the active phase and remission phase of AAV patients (n = 35)
表1. AAV患者活动期和缓解期前后各指标比较(n = 35)

Figure 1. Correlation analysis of activity CD4+T lymphocyte count in AAV patients
图1. AAV患者活动期CD4+淋巴细胞计数相关性分析
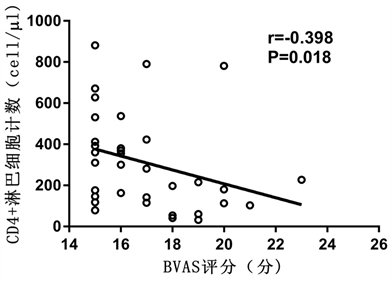
Figure 2. Correlation analysis of remission CD4+T lymphocyte count in AAV patients
图2. AAV患者缓解期CD4+T淋巴细胞计数相关性分析
4. 讨论
AAV是一组以小血管壁炎症和纤维素样坏死为特征的系统性自身免疫性疾病,可累积全身多个系统。大剂量的激素和免疫抑制剂的使用极大地提高了AAV患者的长期生存率,同时也是导致AAV患者发生感染的重要危险因素 [5] [6]。T细胞介导的免疫反应被认为在AAV的发病机制中起重要作用。CD4+T淋巴细胞亚群的异常可能参与了AAV的发病,可能对疾病的持续状态有着重要作用,而且在AAV患者中发现持续激活的T淋巴细胞,并且与AAV的严重程度呈正相关 [7]。相关研究表明T淋巴细胞的衰竭在决定自身免疫性疾病的结局中起着核心作用,对这一过程的靶向操作可能会带来新的治疗机会 [8]。相关研究报道,在GPA患者活动期时CD4+T淋巴细胞水平明显低于缓解期,可能是在抗原的触发下,CD4+T淋巴细胞在活动期选择性的迁移至炎症部位的结果 [2]。Sakatsume等发现新月体肾炎患者肾组织浸润的T细胞与患者尿T细胞表型均为CD4+T淋巴细胞 [9]。而且Abdulahad等 [10] 研究证实尿液中的CD4+T淋巴细胞的出现反映了AAV患者肾损害程度。
本研究中, AAV患者初诊时CD4+T淋巴细胞数量明显减少,并且与BVAS评分呈负相关。我们推测AAV患者初诊时CD4+T淋巴细胞数量的下降可能与AAV活动时导致CD4+T淋巴细胞发生凋亡,是免疫过度激活从而引起免疫失衡的结果。AAV患者初诊时CD4+T淋巴细胞明显下降是AAV活动的现象,不能因为CD4+T淋巴细胞数量的下降而放弃激素和免疫制剂的使用,此时经过积极治疗,可明显降低感染率的发生。本研究存在一定的局限性,我院诊治的AAV患者虽然较多,但符合该研究的纳入和排除标准的研究人群并不多,且纳入的重症AAV患者较多,这可能对结果有一定的影响,需要后期加大样本量更进一步证实。综上,使用激素及免疫抑制剂治疗后发生感染住院的AAV患者,淋巴细胞和CD4+T淋巴细胞减少与死亡相关,因此,在AAV治疗过程中密切监测患者的淋巴细胞及其亚群计数具有重要意义。
文章引用
周静月,苏 阳,张小凡,高鹏丽,陈怿鹏,邢广群. CD4+T淋巴细胞计数在ANCA相关性血管炎患者治疗过程中的变化及其意义
The Significance of CD4+T Lymphocyte Count during the Treatment of Patients with ANCA-Associated Vasculitis[J]. 临床医学进展, 2020, 10(11): 2733-2737. https://doi.org/10.12677/ACM.2020.1011416
参考文献
- 1. Jennette, J.C., Falk, R.J., Bacon, P.A., et al. (2013) 2012 Revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis & Rheumatology, 65, 1-11. https://doi.org/10.1002/art.37715
- 2. Abdulahad, W.H., van der Geld, Y.M., Stegeman, C.A., et al. (2006) Persistent Expansion of CD4+ Effector Memory T Cells in Wegener’s Granulomatosis. Kidney International, 70, 938-947. https://doi.org/10.1038/sj.ki.5001670
- 3. Jennette, J.C., Falk, R.J., Andrassy, K., Bacon, P.A., Churg, J., Gross, W.L., Hagen, E.C., Hoffman, G.S., Hunder, G.G., Kallenberg, C.G., et al. (1994) Nomenclature of Systemic Vasculitides. Proposal of an International Consensus Conference. Arthritis & Rheumatology, 37, 187-192. https://doi.org/10.1002/art.1780370206
- 4. Levey, A.S., Stevens, L.A., Schmid, C.H., Zhang, Y.L., Castro 3rd, A.F., Feldman, H.I., Kusek, J.W., Eggers, P., Van Lente, F., Greene, T., Coresh, J., CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) (2009) A New Equation to Estimate Glomerular Filtration Rate. Annals of Internal Medicine, 150, 604-612. https://doi.org/10.7326/0003-4819-150-9-200905050-00006
- 5. Itabashi, M., Takei, T., Yabuki, Y., et al. (2010) Clinical Outcome and Prognosis of Anti-Neutrophil Cytoplasmic Antibody-Associated Vasculitis in Japan. Nephron Clinical Practice, 115, c21-c27. https://doi.org/10.1159/000286346
- 6. Fauci, A.S., Dale, D.C. and Wolff, S.M. (1974) Cyclophosphamide and Lymphocyte Subpopulations in Wegener’s Granulomatosis. Arthritis & Rheumatology, 17, 355-361. https://doi.org/10.1002/art.1780170404
- 7. Kallenberg, C.G. (2011) Pathogenesis of ANCA-Associated Vasculitis, an Update. Clinical Reviews in Allergy & Immunology, 41, 224-231. https://doi.org/10.1007/s12016-011-8258-y
- 8. McKinney, E.F., Lee, J.C., Jayne, D.R., et al. (2015) T-Cell Exhaustion, Co-Stimulation and Clinical Outcome in Autoimmunity and Infection. Nature, 523, 612-616. https://doi.org/10.1038/nature14468
- 9. Sakatsume, M. and Gejyo, F. (2003) Effector T Cells and Macrophages in Urine as a Hallmark of Systemic Vasculitis Accompanied by Crescentic Glomerulonephritis. Nephrology Dialysis Transplantation, 18, 607-609. https://doi.org/10.1093/ndt/18.3.607
- 10. Abdulahad, W.H., Kallenberg, C.G., Limburg, P.C., et al. (2009) Urinary CD4+ Effector Memory T Cells Reflect Renal Disease Activity in Antineutrophil Cytoplasmic Antibody-Associated Vasculitis. Arthritis & Rheumatology, 60, 2830-2838. https://doi.org/10.1002/art.24747
NOTES
*通讯作者。
