Advances in Clinical Medicine
Vol.
11
No.
04
(
2021
), Article ID:
41860
,
6
pages
10.12677/ACM.2021.114263
肠系膜脂膜炎合并卡氏肺孢子菌肺炎1例报告
刘珍慧,王志强,栾琳慧,万甜甜,于文成*
青岛大学附属医院呼吸与危重症医学科,山东 青岛
收稿日期:2021年3月19日;录用日期:2021年4月19日;发布日期:2021年4月26日

摘要
目的:探讨肠系膜脂膜炎合并卡氏肺孢子菌肺炎的临床表现、诊断方法及治疗策略,加强对肠系膜脂膜炎合并卡氏肺孢子菌肺炎的理解。方法:介绍1例肠系膜脂膜炎合并卡氏肺孢子菌肺炎的临床资料,并进行相关文献复习。结果:该患者在服用激素治疗肠系膜脂膜炎减量过程中出现胸闷、憋气、发热,胸部CT出现双肺多发磨玻璃影,确诊肠系膜脂膜炎合并卡氏肺孢子菌肺炎,应用复方新诺明及卡波芬净及时治疗后好转出院。结论:肠系膜脂膜炎合并卡氏肺孢子菌肺炎如能早期确诊,治疗效果较好。
关键词
卡氏肺孢子菌肺炎,肠系膜脂膜炎,诊治
Reports of a Case of Mesenteric Panniculitis Complicated with Pneumocystis Carinii Pneumonia
Zhenhui Liu, Zhiqiang Wang, Linhui Luan, Tiantian Wan, Wencheng Yu*
The Affiliated Hospital of Qingdao University, Qingdao Shandong

Received: Mar. 19th, 2021; accepted: Apr. 19th, 2021; published: Apr. 26th, 2021

ABSTRACT
Objective: To investigate the clinical features, diagnosis and treatment strategies of patients with mesenteric panniculitis (MP) complicated with pneumocystis carinii pneumonia (PCP), and to strengthen the understanding of mesenteric panniculitis complicated with Pneumocystis carinii pneumonia. Methods: Introduce the clinical data of 1 case of mesenteric panniculitis complicated with pneumocystis carinii pneumonia, and review the relevant literature. Results: The patient diagnosed with mesenteric panniculitis combined with Pneumocystis carinii pneumonia is treated promptly, and is discharged from the hospital. The outpatient return visit did not have obvious respiratory symptoms. Conclusion: If patients with mesenteric panniculitis complicated with Pneumocystis carinii pneumonia can be diagnosed early, the treatment effect is better.
Keywords:Mesenteric Panniculitis, Pneumocystis Carinii Pneumonia (PCP), Diagnosis and Treatment

Copyright © 2021 by author(s) and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/


1. 引言
卡氏肺孢子菌肺炎是一种严重的呼吸系统机会性感染,误诊率及病死率均较高,临床更多见于人类免疫缺陷病毒(Human immunodeficiency virus, HIV)感染患者,但非HIV感染合并卡氏肺孢子菌肺炎发病率逐年增加。目前仍未有肠系膜脂膜炎合并卡氏肺孢子菌肺炎的病例报告。为提高临床认识,实现早期诊断,减少误诊、漏诊,经患者本人知情同意,现将我院收治的1例肠系膜脂膜炎合并卡氏肺孢子菌肺炎病例介绍如下。
2. 病例资料
患者青年女性,主因“胸闷、憋气3天,发热1天”于2020年9月12日入院。患者3天前着凉后出现胸闷、憋气,多于侧卧位时明显,未予重视。1天前患者出现发热,体温最高达39.6℃,胸闷、憋气较前加重,无咳嗽、咳痰,自服“对乙酰氨基酚”后体温降低,数小时后体温再次上升至38℃以上来诊。给予患者左氧氟沙星0.5 g静滴后体温逐渐降至正常,胸闷、憋气等不适较前减轻,以“社区获得性肺炎”收入我院急诊内科。既往:外院确诊“肠系膜脂膜炎”4月,予甲泼尼龙片24 mg bid、环磷酰胺片0.1 g qod,后因胃、后背及脊柱疼痛,停用环磷酰胺,换用吗替麦考酚酯。40余天前我院风湿免疫科住院期间更换治疗方案为甲泼尼龙片40 mg qd,吗替麦考酚酯分散片0.75 g bid。其后规律门诊复诊激素减量,1月前激素减量至36 mg qd,环磷酰胺0.1g qd隔周服用。体检:T:36.3℃ P:87次/分 R:20次/分BP:152/73 mmHg。双肺呼吸音清,未闻及干湿性啰音,右下腹压痛,双下肢指凹性水肿。余查体阴性。入院前查血常规:白细胞计数12.21 * 109/L;中性粒细胞计数10.15 * 109/L;胸部CT提示:双肺炎症可能性大。入院诊断:社区获得性肺炎、肠系膜脂膜炎。
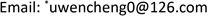
入院后辅助检查:血常规 + CRP:白细胞计数7.81 * 109/L (4.0~10.0 * 109/L),中性粒细胞计数6.69 * 109/L (2.0~7.0 * 109/L),血红蛋白108 g/L (110~150 g/L),中性粒细胞百分率85.60% (50%~75%),全血C反应蛋白16.43 mg/L (<5 mg/L);肝功:乳酸脱氢酶288.00 U/L (135~215 U/L);血糖分析:葡萄糖7.05 mmol/L (3.9~7.0 mmol/L);血脂分析:总胆固醇6.09 mmol/L (3~5.2 mmol/L),低密度脂蛋白3.67 mmol/L (<3.12 mmol/L);电解质、肾功、血磷、血钙、血镁、CK + CKMB、降钙素原、传染性标志物4项均未见明显异常。入院后经验性给予左氧氟沙星抗感染,甲泼尼龙片抗炎等治疗,胸闷、憋气无明显缓解,抗生素升级为莫西沙星后因恶心、头晕等不良反应,换用哌拉西林纳他唑巴坦纳继续抗感染治疗。期间患者仍有反复高热,体温最高达39.3℃,更换口服甲泼尼龙片为甲强龙20 mg qd静滴,并予对乙酰氨基酚对症降温,发热无明显好转。完善CD4绝对计数435 cells/UL,EB病毒衣壳抗原IgG、核抗原IgG阳性,巨细胞病毒抗体及DNA,血培养、痰培养、抗酸菌检测、真菌G试验、曲霉菌GM试验等均为阴性。复查胸部CT:双肺多发磨玻璃样影(如图1)。呼吸科会诊,考虑不除外特殊病原体感染。于09月22日完善气管镜检查,病理回示:(双肺多部位盲检)少许肺及呼吸性粘膜组织呈慢性炎,肺泡上皮较增生,肺泡腔内见灶性泡沫细胞聚集及渗出物机化反应,肺泡间隔增宽伴间质纤维组织增生;肺泡灌洗液病原学检测阴性。NGS检查结果回示考虑为卡氏肺孢子菌肺炎。转入我院呼吸内科,给予卡泊芬净及复方新诺明抗感染治疗。患者胸闷、憋气及胸痛缓解,复查CT示肺内病变较前明显好转(如图2),于10月1日出院。出院后患者门诊复诊,截至目前为止未再出现明显胸闷、胸痛、发热等症状。
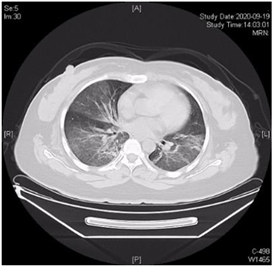
Figure 1. On September 19, chest CT showed extensive ground glass opacity in both lungs
图1. 9月19日胸部CT示双肺广泛磨玻璃影
Figure 2. On September 30, chest CT showed that bilateral lung lesions were significantly improved
图2. 9月30日胸部CT示双肺病变较前明显好转
3. 讨论
卡氏肺孢子菌肺炎(Pneumocystis carinii pneumonia, PCP),是由寄生于人体肺泡上皮细胞表面的卡氏肺囊虫大量繁殖造成上皮细胞损害,阻碍气体交换的一种机会性感染 [1]。该病是由T细胞和体液免疫反应(在较小程度上)介导的。在免疫抑制的患者中,感染会导致由单核细胞、CD8淋巴细胞和激活的巨噬细胞介导的免疫反应功能失调,从而导致弥漫性肺损伤 [2]。此外,吸入的肺孢子虫滋养体抑制肺泡内的上皮修复过程,导致严重的肺损伤 [3]。PCP感染后可以表现为轻微的炎症至重症肺炎,严重者导致呼吸衰竭甚至死亡 [4],临床特征是干咳、发热和呼吸困难。胸部X线片上,最常见弥漫性双肺间质浸润,高分辨率计算机断层扫描可能显示出广泛的磨玻璃影及囊性病变 [5] [6],是一种临床病死率极高的疾病。
本病多发生在免疫功能缺陷及长期应用免疫抑制剂的患者中。HIV阴性的患者PCP发病率较低,约为0.01%~0.10% [1]。但值得注意的是,随着免疫抑制剂的逐步使用,非HIV感染的免疫抑制人群的发病率也随之增加 [5] [7] [8]。在HIV阴性患者中,炎症性疾病占PCP的20% [9]。对于接受免疫抑制药物治疗的自身免疫性疾病患者,合并PCP目前还没有具体的共识指南 [10] [11] [12]。已经明确的是,炎症性疾病及其并发症和免疫抑制治疗方案增加了这类患者患PCP的风险 [13]。
肠系膜脂膜炎(Mesenteric panniculitis,MP)是一种临床上十分罕见的慢性肠系膜炎症性疾病。MP的病因可能是腹部手术、外伤、缺血、药物、过敏或自身免疫性疾病 [14] [15] [16] [17]。临床上根据MP患者的具体情况,通常选择保守治疗,如抗感染和/或免疫抑制治疗、糖皮质激素、非甾体类抗炎药物、秋水仙碱、黄体酮、环磷酰胺药物治疗等,但疗效报道不一致 [15] [16] [17] [18]。该患者炎症性疾病本身及糖皮质激素、环磷酰胺、吗替麦考酚酯等免疫抑制药物的使用,可能都是促进PCP的因素。
非HIV感染患者合并PCP的死亡率(27%~62%)高于HIV感染者(4%~15%) [6] [10] [19] - [24]。成人数据显示,与HIV感染者可能缓慢且隐匿的表现不同,非HIV感染的免疫功能受损者可能会出现快速进展性的病程,通常在几天内出现呼吸衰竭 [1] [5] [21] [25]。此外,非HIV感染患者合并PCP的临床表现也取决于所使用的免疫抑制剂,其中最常提到的有:长时间应用中到高剂量糖皮质激素、环磷酰胺、利妥昔单抗、阿林单抗和肿瘤坏死因子拮抗剂 [26] [27]。糖皮质激素可以减少CD4淋巴细胞,进而可能导致PCP更易发生。在非HIV感染免疫抑制人群中,使用糖皮质激素已成为PCP的主要致病因素,当强的松龙达到或超过16 mg时,风险尤其增加 [28]。有趣的是,在一些研究中,相当比例的PCP只在皮质类固醇逐渐减量过程中出现 [29]。本例病人在肠系膜脂膜炎治疗过程中先后应用环磷酰胺、吗替麦考酚酯等免疫抑制剂及糖皮质激素,且正是在糖皮质激素减量过程中出现PCP感染。值得注意的是,并非所有免疫抑制患者都会出现淋巴细胞减少症 [29]。与HIV感染者一样,监测CD4+ T淋巴细胞似乎不足以预测PCP发生风险 [30]。支气管镜、支气管灌洗或经支气管活检诊断率高于痰液诊断的诊断率,但不易获得 [31]。非HIV感染的PCP患者少见,缺乏特异有效且易行的诊断手段,是导致该病诊断困难乃至误诊、漏诊的重要原因。该病例CD4 + T淋巴细胞未见明显下降,支气管镜检测及肺泡灌洗液均未检见卡氏肺孢子球菌,但不能据此排除PCP感染。PCP患者临床病程凶险,病死率极高,尤其非HIV感染的PCP患者病情进展迅速,提示我们临床诊治过程中,辅助检查不十分支持的情况下仍不应忽视该病可能。另外,肠系膜脂膜炎罕见,对肠系膜脂膜炎的病因及治疗认识不足,导致未对患者免疫抑制药物及糖皮质激素用药史引起足够重视也是PCP诊断延误的原因之一。
PCP的一线治疗是甲氧苄啶–磺胺异甲噁唑静脉注射,因其具有良好的组织渗透性、快速反应和低成本等优点 [5]。不良反应包括白细胞减少、血小板减少和包括史蒂文斯–约翰逊综合征在内的皮疹 [32]。然而,这些反应在儿童中似乎不太常见 [33]。也有研究支持卡泊芬净用于PCP的治疗。目前已有TMP-SMZ治疗PCP失败换用卡泊芬净治疗成功的报道 [34],亦有卡泊芬净联合TMP-SMZ成功治疗PCP且减少TMP-SMZ不良反应发生率的报道 [35]。PCP早期确诊治疗反应较好,多数可以得到恢复,更严重的病程往往认为继发于更具播散性的肺部炎症反应和诊断延迟 [5] [36]。所以,临床工作中,应充分强调早期诊断的重要性,提高对非HIV感染合并PCP患者,乃至肠系膜脂膜炎合并PCP患者的认识。同时,提倡对于临床上疑诊PCP的患者,在第一时间,而不必须等待病原学证据确诊,果断、及时地给予经验性治疗。
文章引用
刘珍慧,王志强,栾琳慧,万甜甜,于文成. 肠系膜脂膜炎合并卡氏肺孢子菌肺炎1例报告
Reports of a Case of Mesenteric Panniculitis Complicated with Pneumocystis Carinii Pneumonia[J]. 临床医学进展, 2021, 11(04): 1202-1207. https://doi.org/10.12677/ACM.2021.114263
参考文献
- 1. Kovacs, J.A., et al. (1984) Pneumocystis Carinii Pneumonia: A Comparison between Patients with the Acquired Immunodeficiency Syndrome and Patients with Other Immunodeficiencies. Annals of Internal Medicine, 100, 663-671. https://doi.org/10.7326/0003-4819-100-5-663
- 2. Beck, J.M., et al. (1991) Inflammatory Responses to Pneumocystis Carinii in Mice Selectively Depleted of Helper T Lymphocytes. American Journal of Respiratory Cell and Molecular Biology, 5, 186-197. https://doi.org/10.1165/ajrcmb/5.2.186
- 3. Limper, A.H. and Martin, W.J. (1990) Pneumocystis Carinii: Inhibition of Lung Cell Growth Mediated by Parasite Attachment. Journal of Clinical Investigation, 85, 391-396. https://doi.org/10.1172/JCI114451
- 4. Chapman, J.R., et al. (2013) Post-Transplant Pneumocystis jirovecii Pneumonia—A Re-Emerged Public Health Problem? Kidney International, 84, 240-243. https://doi.org/10.1038/ki.2013.212
- 5. Morris, A. and Norris, K.A. (2012) Colonization by Pneumocystis jirovecii and Its Role in Disease. Clinical Microbiology Reviews, 25, 297-317. https://doi.org/10.1128/CMR.00013-12
- 6. Chen, M., et al. (2015) Pneumocystis Pneumonia in Patients with Autoimmune Diseases: A Retrospective Study Focused on Clinical Characteristics and Prognostic Factors Related to Death. PLoS ONE, 10, e0139144. https://doi.org/10.1371/journal.pone.0139144
- 7. Saltzman, R.W., et al. (2012) Clinical Conditions Associated with PCP in Children. Pediatric Pulmonology, 47, 510-516. https://doi.org/10.1002/ppul.21577
- 8. Bienvenu, A.L., et al. (2016) Pneumocystis Pneumonia Suspected Cases in 604 Non-HIV and HIV Patients. International Journal of Infectious Diseases, 46, 11-17. https://doi.org/10.1016/j.ijid.2016.03.018
- 9. Desales, A.L., et al. (2012) Pneumocystosis in a Patient with Crohn’s Disease Treated with Combination Therapy with Adalimumab. Journal of Crohn’s and Colitis, 6, 483-487. https://doi.org/10.1016/j.crohns.2011.10.012
- 10. Baulier, G., et al. (2018) Guidelines for Prophylaxis of Pneumocystis Pneumonia Cannot Rely Solely on CD4-Cell Count in Autoimmune and Inflammatory Diseases. Clinical and Experimental Rheumatology, 36, 490-493.
- 11. Stamp, L.K. and Hurst, M. (2010) Is There a Role for Consensus Guidelines for P. jiroveci Pneumonia Prophylaxis in Immunosuppressed Patients with Rheumatic Diseases? The Journal of Rheumatology, 37, 686-688. https://doi.org/10.3899/jrheum.091426
- 12. Park, J.W., et al. (2018) Prophylactic Effect of Trimethoprim-Sulfamethoxazole for Pneumocystis Pneumonia in Patients with Rheumatic Diseases Exposed to Prolonged High-Dose Glucocorticoids. Annals of the Rheumatic Diseases, 77, 644-649. https://doi.org/10.1136/annrheumdis-2017-211796
- 13. Salzer, H.J.F., et al. (2018) Clinical, Diagnostic, and Treatment Disparities between HIV-Infected and Non-HIV-Infected Immunocompromised Patients with Pneumocystis jirovecii Pneumonia. Respiration, 96, 52-65. https://doi.org/10.1159/000487713
- 14. Akram, S., et al. (2007) Sclerosing Mesenteritis: Clinical Features, Treatment, and Outcome in Ninety-Two Patients. Clinical Gastroenterology and Hepatology, 5, 589-596. https://doi.org/10.1016/j.cgh.2007.02.032
- 15. Sharma, P., et al. (2017) Sclerosing Mesenteritis: A Systematic Review of 192 Cases. Clinical Journal of Gastroenterology, 10, 103-111. https://doi.org/10.1007/s12328-017-0716-5
- 16. Mizuno, S., et al. (2017) Increased Levels of Prostaglandin E-Major Urinary Metabolite (PGE-MUM) in Active Mesenteric Panniculitis Patients: A Case Report. Medicine (Baltimore), 96, e9237. https://doi.org/10.1097/MD.0000000000009237
- 17. Hussein, M.R. and Abdelwahed, S.R. (2015) Mesenteric Panniculitis: An Update. Expert Review of Gastroenterology & Hepatology, 9, 67-78. https://doi.org/10.1586/17474124.2014.939632
- 18. Coulier, B., et al. (2017) Synchronous Association of Typical and Transient Mesenteric Panniculitis with Acute Gastrointestinal Attack of Adult-Onset Henoch-Schönlein Purpura. Diagnostic and Interventional Imaging, 98, 571-573. https://doi.org/10.1016/j.diii.2017.03.002
- 19. Schmidt, J.J., et al. (2018) Clinical Course, Treatment and Outcome of Pneumocystis Pneumonia in Immunocompromised Adults: A Retrospective Analysis over 17 Years. Critical Care, 22, 307. https://doi.org/10.1186/s13054-018-2221-8
- 20. Roux, A., et al. (2014) Pneumocystis jirovecii Pneumonia in Patients with or without AIDS, France. Emerging Infectious Diseases, 20, 1490-1497. https://doi.org/10.3201/eid2009.131668
- 21. Fillatre, P., et al. (2014) Incidence of Pneumocystis jiroveci Pneumonia among Groups at Risk in HIV-Negative Patients. The American Journal of Medicine, 127, 1242.e11-7. https://doi.org/10.1016/j.amjmed.2014.07.010
- 22. Messiaen, P.E., et al. (2017) The Role of CD4 Cell Count as Discriminatory Measure to Guide Chemoprophylaxis against Pneumocystis jirovecii Pneumonia in Human Immunodeficiency Virus-Negative Immunocompromised Patients: A Systematic Review. Transplant Infectious Disease, 19, e12651. https://doi.org/10.1111/tid.12651
- 23. Ward, M.M. and Donald, F. (1999) Pneumocystis Carinii Pneumonia in Patients with Connective Tissue Diseases: The Role of Hospital Experience in Diagnosis and Mortality. Arthritis & Rheumatology, 42, 780-789. https://doi.org/10.1002/1529-0131(199904)42:4<780::AID-ANR23>3.0.CO;2-M
- 24. Falagas, M.E., et al. (2007) Infection-Related Morbidity and Mortality in Patients with Connective Tissue Diseases: A Systematic Review. Clinical Rheumatology, 26, 663-670. https://doi.org/10.1007/s10067-006-0441-9
- 25. Monnet, X., et al. (2008) Critical Care Management and Outcome of Severe Pneumocystis Pneumonia in Patients with and without HIV Infection. Critical Care, 12, R28. https://doi.org/10.1186/cc6806
- 26. Grubbs, J.A. and Baddley, J.W. (2014) Pneumocystis jirovecii Pneumonia in Patients Receiving Tumor-Necrosis-Fac- tor-Inhibitor Therapy: Implications for Chemoprophylaxis. Current Rheumatology Reports, 16, 445. https://doi.org/10.1007/s11926-014-0445-4
- 27. Martin-Garrido, I., et al. (2013) Pneumocystis Pneumonia in Patients Treated with Rituximab. Chest, 144, 258-265. https://doi.org/10.1378/chest.12-0477
- 28. Okafor, P.N., Nunes, D.P. and Farraye, F.A. (2013) Pneumocystis jiroveci Pneumonia in Inflammatory Bowel Disease: When Should Prophylaxis Be Considered? Inflammatory Bowel Diseases, 19, 1764-1771. https://doi.org/10.1097/MIB.0b013e318281f562
- 29. Yu, Q., et al. (2017) Outcomes and Prognostic Factors of Non-HIV Patients with Pneumocystis jirovecii Pneumonia and Pulmonary CMV Co-Infection: A Retrospective Cohort Study. BMC Infectious Diseases, 17, 392. https://doi.org/10.1186/s12879-017-2492-8
- 30. Calero-Bernal, M.L., et al. (2016) Intermittent Courses of Corticosteroids Also Present a Risk for Pneumocystis Pneumonia in Non-HIV Patients. Canadian Respiratory Journal, 2016, Article ID: 2464791. https://doi.org/10.1155/2016/2464791
- 31. Wasserman, S., et al. (2016) Burden of Pneumocystis Pneumonia in HIV-Infected Adults in Sub-Saharan Africa: A Systematic Review and Meta-Analysis. BMC Infectious Diseases, 16, 482. https://doi.org/10.1186/s12879-016-1809-3
- 32. Bakeera-Kitaka, S., et al. (2004) Pneumocystis Carinii in Children with Severe Pneumonia at Mulago Hospital, Uganda. Annals of Tropical Paediatrics, 24, 227-235. https://doi.org/10.1179/027249304225019046
- 33. Stern, A., et al. (2014) Prophylaxis for Pneumocystis Pneumonia (PCP) in Non-HIV Immunocompromised Patients. Cochrane Database of Systematic Reviews, No. 10, CD005590. https://doi.org/10.1002/14651858.CD005590.pub3
- 34. Tasaka, S., et al. (2007) Serum Indicators for the Diagnosis of Pneumocystis Pneumonia. Chest, 131, 1173-1180. https://doi.org/10.1378/chest.06-1467
- 35. Desmet, S., et al. (2009) Serum (1-3)-beta-D-glucan as a Tool for Diagnosis of Pneumocystis jirovecii Pneumonia in Patients with Human Immunodeficiency Virus Infection or Hematological Malignancy. Journal of Clinical Microbiology, 47, 3871-3874. https://doi.org/10.1128/JCM.01756-09
- 36. Mansharamani, N.G., et al. (2000) Management and Outcome Patterns for Adult Pneumocystis Carinii Pneumonia, 1985 to 1995: Comparison of HIV-Associated Cases to Other Immunocompromised States. Chest, 118, 704-711. https://doi.org/10.1378/chest.118.3.704
NOTES
*通讯作者。