Advances in Clinical Medicine
Vol.
09
No.
11
(
2019
), Article ID:
32945
,
5
pages
10.12677/ACM.2019.911195
Effects of Amlodipine on Carotid Atherosclerosis in Patients with Hypertension
Xinyu Du1, Peng Cui1, Jinpeng Pan2, Rui Zhang1, Hairong Zhao1*
1General Medicine Department (Hypertension Clinic), Qingdao Hiser Medical Group, Qingdao Shandong
2Department of Cardiology Medicine, Qingdao No. 9 People’s Hospital, Qingdao Shandong

Received: Oct. 25th, 2019; accepted: Nov. 7th, 2019; published: Nov. 14th, 2019

ABSTRACT
Objective: To further explore the effect of amlodipine on carotid atherosclerosis, and to provide a theoretical basis for the selection of clinical medication for patients. Methods: 120 patients were enrolled in the experimental group (60 patients taking amlodipine at 5 mg/day) and the control group (60 patients taking placebo at 5 mg/day). Carotid ultrasound was measured at the beginning, 6 months and 12 months, respectively. Results: 1) The experimental group compared with control group, now in gender, age, smoking, body mass index (BMI), total cholesterol (TC), low density lipoprotein (LDL), high-density lipoprotein (HDL), triglyceride (TG), fasting blood glucose, systolic pressure, diastolic blood pressure, atherosclerosis plaque volume, and the artery plaque thickness has no statistical difference (p < 0.05); 2) The carotid plaque volume in the experimental group ranged from 6 months (706.12 ± 90.08 mm3, p = 0.012) to 12 months (427.84 ± 69.62 mm3, p < 0.001), and the difference was statistically significant. In contrast, carotid plaque volume in the control group ranged from 6 months (793.63 ± 118.17 mm3, p = 0.964) to 12 months (690.52 ± 136.57 mm3, p = 0.088), with no statistically significant difference; 3) The thickness of carotid plaque in the experimental group ranged from 6 months (1.28 ± 0.13 mm, p = 0.379) to 12 months (1.00 ± 0.13 mm, p < 0.000). In contrast, carotid plaque thickness in the control group ranged from 1.33 ± 0.12 mm (p = 0.652) to 12 months (1.31 ± 0.13 mm3, p = 0.715), with no statistically significant difference. Conclusion: Amlodipine can reduce the incidence of atherosclerosis without affecting blood pressure.
Keywords:Hypertension, Amlodipine, Carotid Atherosclerosis
氨氯地平对高血压患者颈动脉粥样硬化的影响
杜芯瑜1,崔鹏1,潘金鹏2,张锐1,赵海蓉1*
1青岛市海慈医疗集团全科医学科(高血压门诊),山东 青岛
2青岛市第九人民医院心内科,山东 青岛

收稿日期:2019年10月25日;录用日期:2019年11月7日;发布日期:2019年11月14日

摘 要
目的:进一步探讨氨氯地平对颈动脉粥样硬化的影响,为患者临床用药的选择提供理论依据。方法入选120名患者,实验组(60例服用氨氯地平5 mg/日)和对照组(60例,服用安慰剂5 mg/日),分别测量初始、6个月、12个月患者的颈动脉超声情况。结果:1) 实验组与对照组比较,在性别、年龄、现在吸烟情况、体重指数(BMI)、总胆固醇(TC)、低密度脂蛋白(LDL)、高密度脂蛋白(HDL)、甘油三酯(TG)、空腹血糖、收缩压、舒张压、动脉粥样硬化斑块体积、劲动脉斑块厚度无统计学差异(p < 0.05);2) 实验组颈动脉硬化斑块体积6个月(706.12 ± 90.08 mm3, p = 0.012)到12个月(427.84 ± 69.62 mm3, p < 0.001),差异有统计学意义;相反,对照组中颈动脉硬化斑块体积6个月(793.63 ± 118.17 mm3, p = 0.964)到12个月(690.52 ± 136.57 mm3, p = 0.088),差异无统计学意义;3) 实验组颈动脉硬化斑块厚度6个月(1.28 ± 0.13 mm, p = 0.379)到12个月(1.00 ± 0.13 mm, p < 0.000);相反,对照组中颈动脉硬化斑块厚度6个月1.33 ± 0.12 mm, p = 0.652)到12个月(1.31 ± 0.13 mm3, p = 0.715),差异无统计学意义。结论:发现氨氯地平在不影响血压的情况下,可降低劲动脉粥样硬化的发生。
关键词 :高血压,氨氯地平,颈动脉粥样硬化

Copyright © 2019 by author(s) and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


1. 引言
颈动脉粥样硬化是一种常见疾病。相关研究表明,颈动脉粥样硬化是短暂性脑缺血等脑血管疾病的重要病理因素之一 [1],并且颈动脉硬化可以提高对冠状动脉硬化性心脏病的预测 [2] [3]。而引起颈动脉硬化的危险因素有总胆固醇水平、低密度脂蛋白水平、收缩压水平 [4]。高血压在劲动脉硬化的发生发展中起重要作用,其可通过增加氧化应激、细胞因子水平、细胞粘附分子和趋化因子诱导动脉粥样硬化 [5]。相关文献研究表明,降压药可降低颈动脉硬化水平 [6]。氨氯地平作为一线降压药物,众多研究表明氨氯地平可以显著抑制动脉粥样硬化的进展,减少心血管事件 [7] [8]。但氨氯地平延缓颈动脉硬化的机制尚不明确。此次实验进一步探讨氨氯地平对颈动脉粥样硬化的影响,为患者临床用药的选择提供理论依据。
2. 材料和方法
2.1. 纳入人群
本研究为前瞻性研究。选择2016年1月至2016年6月,就诊青岛市海慈医院全科医学科的高血压患者120例,年龄在50~85岁之间。所有受试者住院期间均行颈动脉彩色多普勒超声检查(均有颈动脉斑块)。排除:1) 缺血性脑卒中患者;2) 颈动脉闭塞患者;3) 高危心脏病患者。将患者随机分为两组:实验组(60例服用氨氯地平5 mg/日)和对照组(60例,服用安慰剂5 mg/日),分别测量初始、6个月、12个月患者的颈动脉超声情况。最终完成研究的为实验组60例,对照组59例(1人随访丢失)。本研究已获我院机构审查委员会批准,并获得每位患者的知情同意。
2.2. 彩色多普勒超声
采用飞利浦HD15彩色多普勒超声仪(飞利浦超声)从近端到远端扫描双侧颈动脉。采用B型超声测量颈动脉板块的厚度、形态、大小和范围。采用无彩色血流信号的纵向和横向超声及多普勒频谱检测动脉壁是否存在栓塞物,判断颈动脉是否闭塞。所有研究数据均由2名心脏超声医师进行分析。通过协商解决读数上的差异,如果不能达成一致意见,就征求第三位有经验的读者的意见。
2.3. 统计分析
描述性统计以平均 ± 标准差或%表示。连续变量采用t检验或秩和检验,分类变量采用卡方检验描述临床特征。采用配对t检验(正态分布数据),比较不同时间点斑块参数。采用SPSS 17.0软件进行统计分析。p < 0.05有统计学意义。
3. 结果
3.1. 一般临床特征
实验组与对照组比较,在性别、年龄、现在吸烟情况、体重指数(BMI)、总胆固醇(TC)、低密度脂蛋白(LDL)、高密度脂蛋白(HDL)、甘油三酯(TG)、空腹血糖、收缩压、舒张压、动脉粥样硬化斑块体积、劲动脉斑块厚度无统计学差异(p < 0.05) (表1)。
Table 1. Clinical features of two groups
表1. 两组临床特征
*数据以均数±标准差或(%)表示。BMI:身体质量指数;TC:总胆固醇;LDL:低密度脂蛋白;HDL高密度脂蛋白;TG:甘油三酯。**差异有统计学意义(p < 0.05)。
3.2. 斑块体积比较
图1结果,实验组颈动脉硬化斑块体积6个月(706.12 ± 90.08 mm3, p = 0.012)到12个月(427.84 ± 69.62 mm3, p < 0.001),差异有统计学意义;相反,对照组中颈动脉硬化斑块体积6个月(793.63 ± 118.17 mm3, p = 0.964)到12个月(690.52 ± 136.57 mm3, p = 0.088),差异无统计学意义。

Figure 1. Comparison of carotid plaque volume
图1. 颈动脉斑块体积比较
3.3. 劲动脉斑块厚度比较
图2结果,实验组颈动脉硬化斑块厚度6个月(1.28 ± 0.13 mm, p = 0.379)到12个月(1.00 ± 0.13 mm, p < 0.000);相反,对照组中颈动脉硬化斑块厚度6个月(1.33 ± 0.12 mm, p = 0.652)到12个月(1.31 ± 0.13 mm3, p = 0.715),差异无统计学意义。
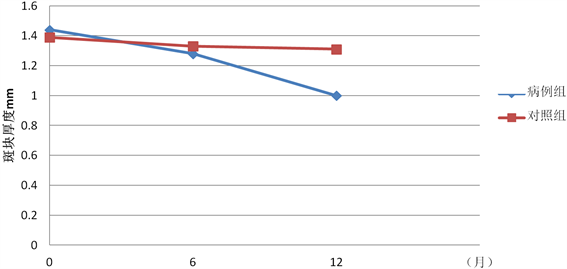
Figure 2. Comparison of carotid plaque thickness
图2. 颈动脉斑块厚度比较
4. 讨论
颈动脉粥样硬化是一种发病率高的疾病,与中风、冠心病、高血压的发生密切相关 [1] [2] [3]。氨氯地平在治疗颈动脉效果的评价并不一致,相关研究表明,氨氯地平可明显降低颈动脉粥样硬化发生风险 [9] [10]。相反,另一些研究表明,氨氯地平与颈动脉粥样硬化的进展关系并不密切 [11] [12]。相关文献结果不一致,可能与研究方法及药物用量不一致有关。此次我们通过小剂量氨氯地平应用,在不影响血压的情况下,收缩压6个月(130.55 ± 20.49 mmHg, p = 0.327)到12个月(133.97 ± 24.11 mmHg, p = 0.205),舒张压6个月(85.59 ± 11.87 mmHg, p = 0.658)到12个月(133.97 ± 24.11 mmHg, p = 0.796),发现氨氯地平可降低劲动脉粥样硬化的发生。这与相关动物实验的研究结果:“氨氯地平抑制血管细胞衰老和保护动脉粥样硬化的发生,至少部分是通过独立于钙通道阻断的机制”是一致的 [13]。这有待于大样本、多中心的临床研究进一步研究证实。
文章引用
杜芯瑜,崔 鹏,潘金鹏,张 锐,赵海蓉. 氨氯地平对高血压患者颈动脉粥样硬化的影响
Effects of Amlodipine on Carotid Atherosclerosis in Patients with Hypertension[J]. 临床医学进展, 2019, 09(11): 1261-1265. https://doi.org/10.12677/ACM.2019.911195
参考文献
- 1. Underhill, H.R., Yuan, C., Yarnykh, V.L., et al. (2010) Predictors of Surface Disruption with MR Imaging in Asymp-tomatic Carotid Artery Stenosis. American Journal of Neuroradiology, 31, 487-493. https://doi.org/10.3174/ajnr.A1842
- 2. Lorenz, M.W., Polak, J.F., Kavousi, M., et al. (2012) Carotid Inti-ma-Media Thickness Progression to Predict Cardiovascular Events in the General Population (the PROG-IMT Collabo-rative Project): A Meta-Analysis of Individual Participant Data. The Lancet, 379, 2053-2062. https://doi.org/10.1016/S0140-6736(12)60441-3
- 3. Nambi, V., Chambless, L., He, M., et al. (2012) Common Carotid Artery Intima-Media Thickness Is as good as Carotid Intima-Media Thickness of All Carotid Artery Segments in Improving Prediction of Coronary Heart Disease Risk in the Atherosclerosis Risk in Communities (ARIC) Study. Euro-pean Heart Journal, 55, 183-190. https://doi.org/10.1093/eurheartj/ehr192
- 4. Mathiesen, E.B., Joakimsen, O., BØNaa, K.H. (2001) Prevalence of and Risk Factors Associated with Carotid Artery Stenosis: The Tromsø Study. Cerebrovascular Diseases, 12, 44-51. https://doi.org/10.1159/000047680
- 5. Prasad, K. (2015) Pathophysiology and Medical Treatment of Carotid Ar-tery Stenosis. International Journal of Angiology, 24, 158-172. https://doi.org/10.1055/s-0035-1554911
- 6. Cuspidi, C., Negri, F., Giudici, V., et al. (2009) Effects of Antihy-pertensive Drugs on Carotid Intima-Media Thickness: Focus on Angiotensin II Receptor Blockers. A Review of Ran-domized, Controlled Trials. Integrated Blood Pressure Control, 2009, 1-8. https://doi.org/10.2147/IBPC.S5174
- 7. Nissen, S.E., Tuzcu, E.M., Libby, P., et al. (2004) Effect of Antihyper-tensive Agents on Cardiovascular Events in Patients with Coronary Disease and Normal Blood Pressure: The CAMELOT Study: A Ran-Domized Controlled Trial. JAMA, 292, 2217-2225. https://doi.org/10.1001/jama.292.18.2217
- 8. Dahlöf, B., Sever, P.S., Poulter, N.R., et al. (2005) Prevention of Cardiovascular Events with an Antihypertensive Regimen of Amlodipine Adding Perindopril as Required versus Atenolol Adding Bendroflumethiazide as Required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): A Multicentre Randomised Controlled Trial. The Lancet, 366, 895-906. https://doi.org/10.1016/S0140-6736(05)67185-1
- 9. Weiss, D. and Taylor, W.R. (2008) Deoxycorticosterone Ac-etate Salt Hypertension in Apolipoprotein E−/− Mice Results in Accelerated Atherosclerosis: The Role of Angiotensin II. Hypertension, 51, 218-224. https://doi.org/10.1161/HYPERTENSIONAHA.107.095885
- 10. Chen, X.F., Rateri, D.L., Howatt, D.A., et al. (2013) Amlodipine Reduces AngII-Induced Aortic Aneurysms and Atherosclerosis in Hypercholesterolemic Mice. PLoS ONE, 8, e81743. https://doi.org/10.1371/journal.pone.0081743
- 11. Doran, D.E., Weiss, D., Zhang, Y., Griendling, K.K. and Taylor, W.R. (2007) Differential Effects of AT1 Receptor and Ca2+ Channel Blockade Onatherosclerosis, In-flammatory Gene Expression, and Production of Reactive Oxygen Species. Atherosclerosis, 195, 39-47. https://doi.org/10.1016/j.atherosclerosis.2006.11.030
- 12. Nakandakare, E.R., Charf, A.M. and Quintão, E.C.R. (2008) Dietary Salt Restriction Increases Plasma Lipoprotein and Inflammatory Marker Concentrations in Hypertensive Patients. Atherosclerosis, 200, 410-416. https://doi.org/10.1016/j.atherosclerosis.2007.12.034
- 13. Kayamori, H., Shimizu, I., Yoshida, Y., et al. (2018) Amlodipine Inhibits Vascular Cell Senescence and Protects Against Atherogenesis through the Mechanism Independent of Calcium Channel Blockade. International Heart Journal, 59, 607-613. https://doi.org/10.1536/ihj.17-265
