Asian Case Reports in Surgery
Vol.3 No.04(2014), Article ID:14580,5 pages
DOI:10.12677/ACRS.2014.34004
The Use of Branch with Slot Coated Stent in the Treatment of Complex Thoracic Aortic Dissection
Department of Vascular Surgery, Xiangya Hospital of Central South University, Changsha
Email: *huangjianhua@medmail.com.cn
Copyright © 2014 by authors and Hans Publishers Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received: Oct. 26th, 2014; revised: Nov. 28th, 2014; accepted: Dec. 5th, 2014
ABSTRACT
Objective: To research the use of branch with slot coated stent for endovascular exclusion in the treatment of complex thoracic aortic dissection. Methods: Totally 2 patients with complex thoracic aortic dissection were treated by EVAR (Endovascular Aneurysm Repair) with branch slot coated stents between Oct. 2012 to Dec. 2012 at our department. Because the bow of thoracic aortic dissection and the crevasse are close to the left subclavian artery and common carotid artery which are unsuitable for standard EVAR, we choose EVAR with branch slot coated stent. During the procedure, by femoral artery incision, we introduced a guide wire through the thoracic aorta and another guide wire through the left brachial artery to reach the left subclavian artery, descending aorta, thoracic aorta and eliciting it from the femoral artery incision. And then, the main stent was placed through the guide wire in the thoracic aorta and the branch stent was placed through the guide wire in the left subclavian artery. Then make an angiography from the unknown artery puncture to make sure the placement of the stent is right, and release the main stent and the branch stent subsequently. Results: The success rate of the procedure was 100%. Angiography at the end of the operation showed normal blood flow into the left subclavian artery, common carotid artery and the crevasse of thoracic aortic dissection was well-separated. There is no inner leakage in the two cases. Conclusion: Branch slot coated stent is an effective supplement of conventional EVAR which is unsuitable for patients with complex thoracic aortic dissection. Further study is necessary to observe its long-term outcomes.
Keywords:Complex Thoracic Aortic Dissection, Endovascular Abdominal Aortic Aneurysm Repair, Branch with Slot Coated Stent

开槽带分支覆膜支架在弓部胸主动脉
夹层中的应用
黄建华*,李 刚,刘晓蕾,刘光强,欧阳洋,王宪伟,王 伟
湘雅医院血管外科,中南大学,长沙
Email: *huangjianhua@medmail.com.cn
收稿日期:2014年10月26日;修回日期:2014年11月28日;录用日期:2014年12月5日

摘 要
目的:探讨开槽带分支覆膜支架在弓部胸主动脉夹层中的应用的价值。方法:2012年10月~2012年12月,对2例弓部胸主动脉夹层采用血管腔内治疗技术(EVAR)治疗。对于弓部胸主动脉夹层,破口接近左锁骨下动脉、颈总动脉,不适于标准的腔内修复,我们采用的方法是开槽带分支胸主动脉覆膜支架植入术。切开股动脉穿刺置入导丝进入胸主动脉;另外,左侧肱动脉穿刺置入另一根导丝到左锁骨下动脉、降主动脉、胸主动脉,并从股动脉的切口引出;通过股动脉的两根导丝置入修复胸主动脉夹层的开槽带分支的覆膜支架主体和分支支架到达预定位置;然后,从无名动脉预置的导管造影,明确分支确实位于左锁骨下动脉中,再相继释放分支支架和主体支架。结果:2例手术全部获成功。腔内治疗最后的造影显示:胸主动脉夹层破口封堵良好,左锁骨下动脉、颈总动脉血流正常。术中2例均无内漏。结论:对于不适宜行传统治疗的弓部胸主动脉夹层,开槽带分支覆膜支架是传统EVAR技术的有效补充。远期效果尚需进一步观察。
关键词
复杂胸主动脉夹层,血管腔内治疗,开槽带分支覆膜支架

1. 引言
胸主动脉夹层的发病率为每年50~100人/10万人,大多数发生于降主动脉,通过覆膜支架治疗,可以达到满意的封堵,疗效良好。然而,约有15%的患者病情复杂,夹层破口很高,甚至累及左锁骨下动脉、颈总动脉。这一类病人,是我们传统介入腔内治疗的难点。因为支架型人工血管完全隔绝目标病变, 要求病变近端必需具备一定的锚定区,因此,锚定区不足的夹层长期被视为腔内隔绝术的禁区[1] [2] 。那么对于紧贴左锁骨下动脉的破口,左侧椎动脉为优势动脉,颈总动脉紧邻左锁骨下动脉的情况,不能封堵左锁骨下动脉怎么办?
本研究采用北京裕恒佳医疗器械有限公司设计的开槽带分支覆膜支架,单分支支架可以有效保证左锁骨下动脉通畅,其前端的V型槽可以保护颈总动脉及头臂干不被覆盖,单分支使得支架定位更稳定达到了良好的治疗效果。现报道如下。
2. 病例介绍
2.1. 一般资料
病例1:男性,64岁,突发胸痛1周2012年12月14日入院,急诊主动脉CTA显示胸主动脉夹层(Stanford B型)。可见夹层的破口紧挨着左锁骨下动脉的后方,不到10 mm。颈总动脉和左锁骨下动脉之间<5 mm,而且左锁骨下动脉比较粗大,左椎动脉为优势动脉(如图1-A)。
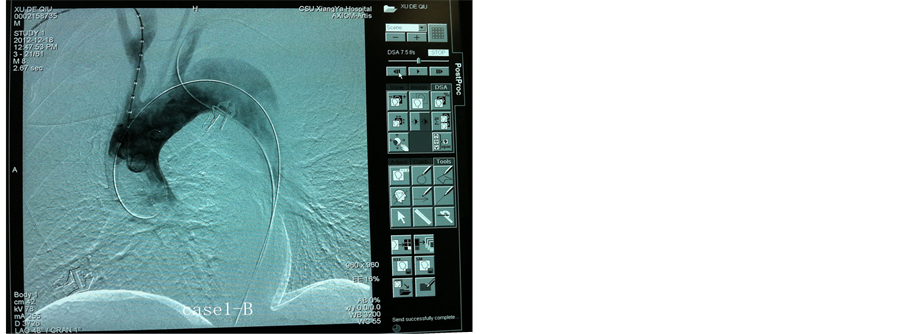
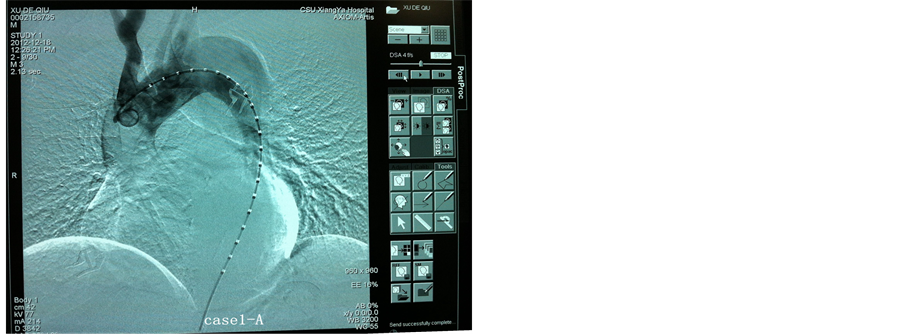
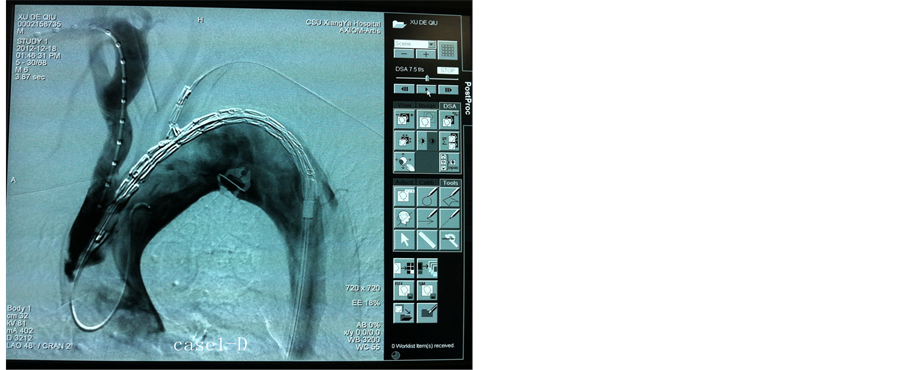
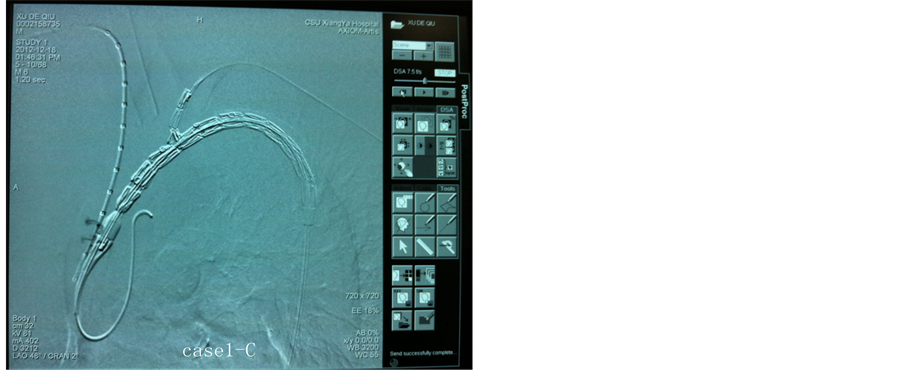
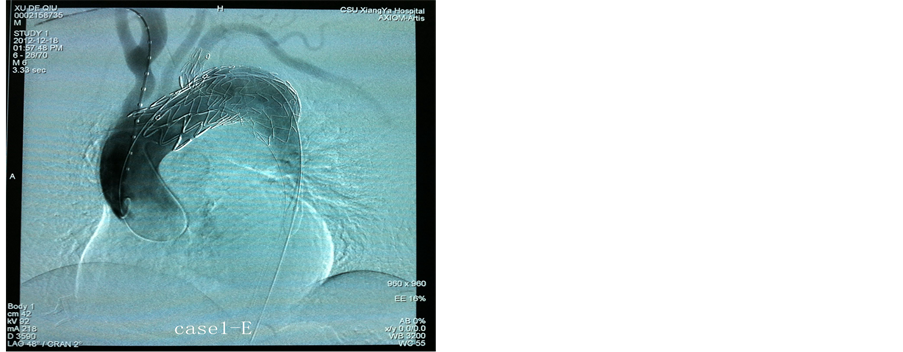
Figure 1. Surgery pictures of case one. A: The radiography of ascending aorta showed high cleavage and big pseudocoele. B: A guide wire was introduced through the thoracic aorta and another guide wire was introduced through the left brachial artery to reach the left subclavian artery. C: The main stent was placed through the guide wire in the thoracic aortic and the branch stent was placed through the guide wire in the left subclavian artery. D: An angiography was made from the unknown artery puncture to make sure the placement of the stent was right. E: Angiography at the end of the operation showed normal blood flew into the left subclavian artery, common carotid artery and well-separated
图1. 病例1手术中图片;A:升主动脉造影显示破口高、假腔大;B:两根导丝分别进入升主动脉和左锁骨下动脉;C:主体支架进入主动脉弓,分支支架进入左锁骨下动脉;D:支架释放前经升主动脉造影显示支架的位置;E:主体支架和分支支架打开后造影显示各分支通畅,夹层破口封堵良好
病例2:男性,52岁,突发胸痛3天于2012年11月20日入院,急诊主动脉CTA显示主动脉夹层(Stanford B型)。破口宽约20 mm,而且位置离左锁骨下动脉不到10 mm,左椎动脉为优势动脉(图2-A)。

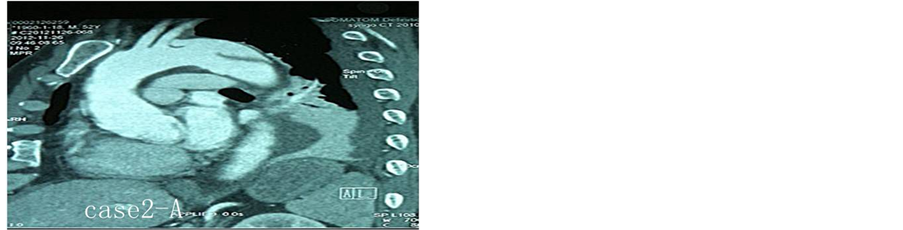
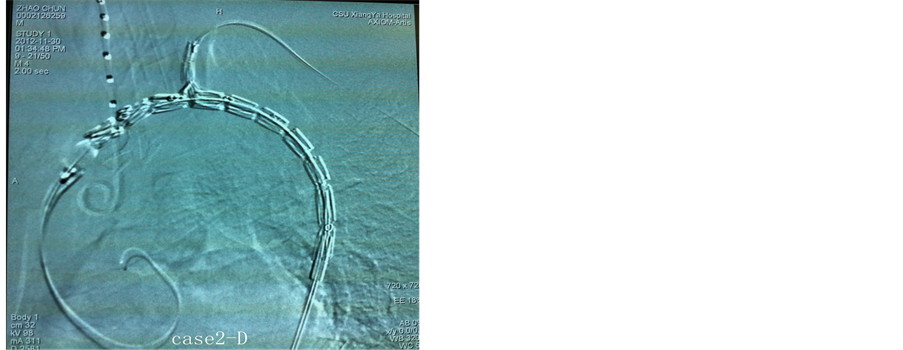
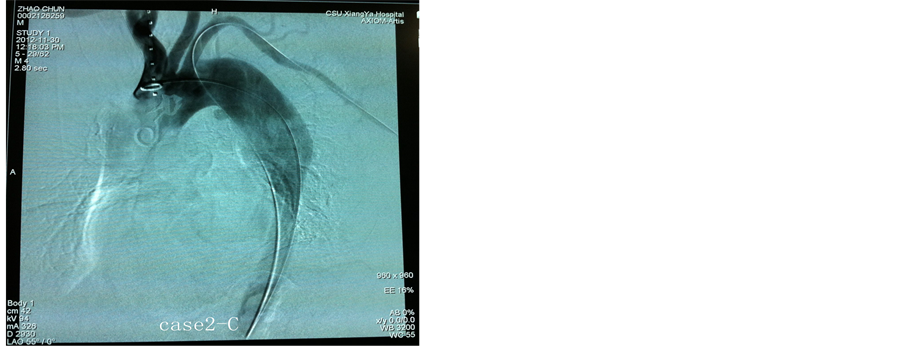
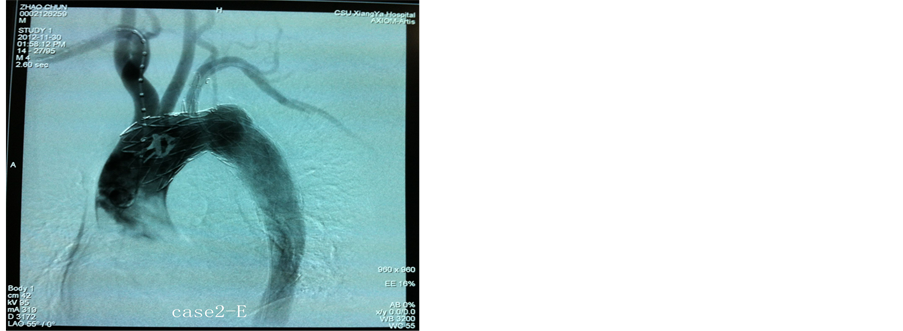
Figure 2. Surgery pictures of case two. A: The CTA before surgery showed high cleavage and big pseudocoele. B: Angiography during surgery showed big pseudocoele and the cleavage was closed to the left brachial artery. C: A guide wire was introduced through the thoracic aorta and another guide wire was introduced through the left brachial artery to reach the left subclavian artery. D: An angiography was made to make sure the placement of the stent was right before the stent was open. E: Angiography at the end of the operation showed normal blood flew into the left subclavian artery, common carotid artery and well-separated
图2. 病例2手术中照片;A:术前CTA显示破口大、位置高;B:术中造影夹层假腔大,破口紧贴左锁骨下动脉;C:双导丝分别进入升主动脉和左锁骨下动脉;D:支架打开之前再次造影定位;E:两支架完全释放后造影结果各分支通畅,破口封堵良好
像这样的病例,如果按照常规的方法将支架放在锁骨下动脉的后缘,无法堵住破口,通常只有把左锁骨下动脉覆盖才能堵住破口,此时椎动脉将会缺血,并且很有可能连颈总动脉也被封堵。所以,本组两例采用开槽带分支覆膜支架治疗。
2.2. 支架的设计
本款支架为前宽后窄的渐细型覆膜支架,整个支架全长140 mm。其前端有12 mm长的裸支架,裸支架后方有长18 mm,宽20 mm的V字型槽,此区没有覆膜部分,V型槽顶点后方3 mm为分支支架起始部,分支支架根据病人左锁骨下动脉直径有不同大小可供选择,长度为27 mm (如图3)。
2.3. 治疗方法
入院后常规控制血压在120/75 mmHg(1 mmHg = 0.133 kP a)以下,心率在60~70次/min左右。起病2 周左右施以腔内治疗。术前CTA和DSA检查,明确夹层破口位置与弓部分支动脉的关系,决定采用开槽带分支覆膜支架治疗。
手术操作:全麻,取一侧腹股沟区切口,暴露股动脉并预置阻断带;穿刺插入动脉鞘,以猪尾导管和泥鳅导丝顺真腔上行至升主动脉,造影后测量血管腔直径、破口位置及弓部分支动脉等供血情况;另外,从左侧肱动脉穿刺,导丝进入左锁骨下动脉到降主动脉、腹主动脉、从股动脉切口引出来。用分线器将两根导丝分开,使其处于平行状态。主体支架套入到达升主动脉的导丝,分支支架套入到达左锁骨下动脉的导丝,将支架一起向上推进(如图1-A),同时稍用力牵拉肱动脉的导丝,使分支更易进入左锁骨下动脉(如图1-B);再从无名动脉预置导管造影明确分支确实位于左锁骨下动脉(如图1-C)。相继释放分支支架和主体支架(如图1-D),最后造影证实支架位置良好(如图1-E)。退出各导管导丝,缝合股动脉切口。第2例方法与病例1完全一致,手术中照片见图2A-2E)。
此二例患者围手术期用硝普钠或硝酸甘油控制血压在目标水平,并尽早过渡为多联口服降压药控制血压。
3. 结果
2例手术均获得满意效果,术后即时造影显示破口封堵完全,分支支架血流正常,左锁骨下动脉无返血,无I型内漏,无术后脑缺血、左上肢缺血、围手术期心脑血管意外发生。术后5~7天出院。
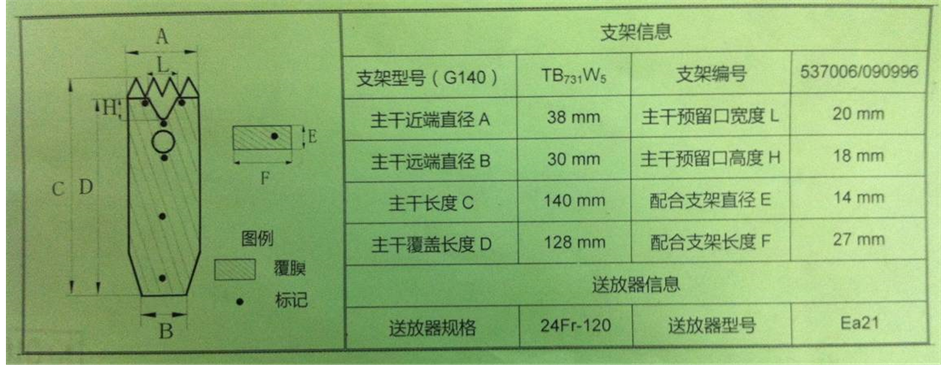
Figure 3. Mode picture of the branch slot coated stent
图3. 开槽带分支支架模式图
4. 讨论
近20年来,主动脉夹层的腔内支架治疗已经成为该病的标准治疗。然而,对于破口位于主动脉弓部,特别是紧邻左锁骨下动脉,并且左锁骨下动脉粗大、左椎动脉为优势动脉时,带膜支架是不能贸然封堵左锁骨下动脉的,以免造成椎动脉缺血的后果。
既往的治疗方法是行开放手术在左颈总动脉到左锁骨下动脉之间人工血管搭桥,然后结扎左锁骨下动脉的吻合口近端。再二期施行主动脉覆膜支架腔内隔绝术。但有创伤大、两次手术、费用高等缺点。
另一种方法是在颈总动脉或者锁骨下动脉各放置“烟窗”支架,对于复杂胸主动脉夹层是一种不错的选择,有学者报道“烟囱”技术可以为第一破口位于弓部重要分支动脉附近的动脉夹层患者,提供腔内隔绝术治疗机会,避免主动脉弓部血管重建开放手术带来的大的创伤。短期随访结果满意,远期疗效有待于进一步随访[3] 。但是,目前看来其最常见的并发症是Ⅰ型内漏,烟囱支架在从主动脉覆膜支架外侧向分支动脉提供血流通道的同时,也在主动脉壁和主动脉覆膜支架之间造成了一条潜在的通向假腔的路径,这极易形成I型内漏[4] 。而且需要颈部开口,增加费用与痛苦。
那么,是否有两全其美的方法,既保证不影响左锁骨下动脉、颈总动脉的血供的同时又将破口封堵完全,既减少手术创伤,又可以简化操作手术呢?
开槽带分支覆膜支架在支架的前端背侧开一窗口接上一支带膜小支架,并且在分支支架的前端带膜部分开一V型槽,手术时分支支架进入左锁骨下动脉,V型槽对准左颈总动脉或无名动脉,支架释放后可以有效的封闭了主动脉夹层的破口,保护左锁骨下动脉,避免左锁骨下动脉和椎动脉缺血所带来的并发症,又可以避免带膜支架前端误封颈总动脉,真正实现了一箭三雕的效果。有效地简化手术步骤,降低手术风险,减少内漏的发生,大大的减轻了病人的痛苦,缩短了住院时间,降低了住院费用,具有良好的可操作性及推广性。
笔者认为使用开槽带分支支架腔内治疗的手术的适应症为:降主动脉夹层,破口距离左锁骨下动脉<10 mm,左椎动脉为优势动脉需要保留;左颈总动脉与左锁骨下动脉贴近,即使封堵左锁骨下动脉也没有拓展锚定区。
术中的关键环节是:右肱动脉穿刺,无名动脉到升主动脉造影;左肱动脉穿刺到左锁骨下动脉、降主动脉、股动脉穿出;从股动脉到升主动脉上加强导丝;分线器分开主动脉内的两根导丝,将支架循两根导丝上行,分支支架进入左锁骨下动脉,造影证实后打开支架。
但目前这样的病例在国内仅少数医院能够开展,病例还比较少,需要大量的病例积累,远期效果有待进一步观察。
参考文献 (References)
- [1] Antoniou, G.A., Mireskandari, M., Bicknell, C.D., et al. (2010) Hybrid repair of the aortic arch in patients with extensive aortic disease. European Journal of Vascular and Endovascular Surgery, 40, 715-721.
- [2] Canaud, L., Hireche, K., Dcannoville, T., et al. (2010) Hybrid aortic arch repair for a ruptured and infected penetrating atherosclerotic ulcer of the aortic arch . Annals of Vascular Surgery, 25, 266.e5-266.e7.
- [3] 郭伟, 张宏鹏, 刘小平, 等 (2010) “烟囱”技术在主动脉弓病变腔内修复中的应用. 中华普通外科杂志, 7, 536- 539.

NOTES
*通讯作者。